Patient Advocacy: Six Steps to Craft a Compelling Message
Patient advocacy involves sharing your unique knowledge and experience of a disease or condition with the ultimate aim of raising awareness and influencing people to create a desired change. This might include speaking at an event, telling your story in the media, or working with an organization to develop new treatment guidelines. This month’s post will show you the steps you should take to create a compelling message to get key issues across to your audience.
1. Develop Your Key Message
The first step is to work out the key message you want to communicate. Asking yourself the following questions will help you focus on the main issues.
- Why do I want people to know about this condition?
- Is very little known about the disease?
- Are doctors not very good at diagnosing it?
- What is the impact of the condition for me and for others?
- What improvements are needed? Locally? Nationally? Internationally?
An effective message is credible, clear and convincing – ideally you should be able to communicate it in less than one minute – for example, “Cancer-related fatigue is poorly understood, but has been reported in 30–50% of breast cancer survivors in the first 5 years after treatment.” The recommended approach is to have one primary message supported by two or three secondary messages. Write down your core message first. The purpose of the secondary messages is to support the core message and to explain how it can be achieved.
Insider Tip
Patient advocate and blogger, Kay Curtin (@KayCurtin1), who is a stage IV Melanoma patient, suggests taking a look at what other organisations are doing before committing “precious time and resources on replicating what’s already been done.” Christina Lizaso (@btrfly12), co-moderator of the #gyncsm Twitter chat, agrees. “Look first to collaborate and move things forward vs. starting from scratch,” she recommends, “then think outside of the condition – what is the most important thing for someone who has never heard of it to know?”
2. Identify Your Target Audience
Deciding who your target audience is and how best to reach them is the next step. There are several broad groups you might consider, including other people with your condition, healthcare professionals, the media, legislators or the general public. Which group you focus on depends on what you are trying to achieve. The more specific you are in identifying your audience, the more effective your message will be. To follow on from my example above, if I want the guidelines for cancer treatment to include cancer-related fatigue, I might want to target healthcare professionals, other patient organizations who are campaigning on similar issues, and organizations like the American Society of Clinical Oncology.
3. Craft Your Message
A persuasive message can be summed up in three words “Make Me Care.” Sharing your story and the stories of others affected by your condition is the most powerful and compelling way you can do this. As Jo Taylor (@abcdiagnosis) founder of After Breast Cancer Diagnosis says, “your story is everything – it raises awareness and shows the passion behind why you are trying to make change as a patient advocate.” Jo also believes your story connects you to others with a similar story, which in turns helps to build strong networks to bring about change. Dementia advocate, Pablo Barredo (@Diario1Cuidador) points out that stories help create bonds not just with patients but with their caregivers too. “Patients and caregivers want personal stories and people who will understand them, not scientific terms they may not understand,” he says. “They need to feel connected to someone who speaks their own language and understands them.”
Insider Tip
When sharing your story, author and breast cancer blogger, Nancy Stordahl (@NancysPoint) points out that “you have to be willing to share from your heart. Be real. Be you. It’s all about being authentic. Always come back to that. Allow others to see your vulnerabilities. When others see that you’re authentic, you’ve made it easier for them to care, not just about you, but about your message(s). Once they care they’ll want to learn more.” Antibiotic resistance campaigner, Vanessa Carter (@_FaceSA) agrees that authenticity is key. “You have to keep telling your story from the heart,” she says, “which is not easy when you’ve repeated it for so many years. It takes a lot of practice. I think it’s one of the greatest arts of advocacy.”
Be prepared that telling your story might make you feel emotional and vulnerable, so think carefully about how much you are willing to share before you make the decision to share it. Let the audience know your boundaries. Be mindful too of boundaries if you are talking about a family member. How conformable are they with you sharing their story or aspects of your own story that may affect them? In Nancy’s words, “each person needs to find her/his own voice over time, figure out what works and feels comfortable for you, and then go with it.”
4. Create a Compelling Call-To-Action
According to the WHO, “you cannot mobilize people unless you ask them to do something. Aim to craft messages that will convince your audiences to act – rather than messages that simply communicate what you want to say. As Christina Lizaso reminds us, “awareness is not the end goal – it should be taking you to education and to action.”
Think about what you want your listener or reader to do when you are finished telling your story? What will motivate them to act? Outline clearly the next steps they need to take. “Awareness should immediately be followed by an opportunity for action,” says breast cancer researcher and advocate, Jamie Holloway (@jamienholloway). While a “dramatic personal story is a more compelling ‘hook’ than just rhyming off a list of facts (no matter how alarming the facts are!),” says Carolyn Thomas (@HeartSisters), author of A Woman’s Guide To Living With Heart Disease, “a story by itself isn’t the message.”
Insider Tip
Alison Cameron (@allyc375) feels strongly that sharing a personal story should be a starting point for action, not the end goal. “For me, the personal story has its place yes, but is a starting not an end point, “she says. “The crucial thing is not to fall into ‘inspirational patient’ mode but to work with those listening to come up with concrete actions for change. I got very weary of being parachuted in to ‘tell my story’ then kicked out swiftly after being patted on the head and told how “inspirational” I am. What changed as a result of all that? Not a great deal.”
5. Communicate Your Message
Now that you have identified your target audience and crafted your message you need to think about how to communicate it. The most straight forward way of communicating is directly such as a face—to-face meeting, an email, or a phone call. Plan ahead for how you will share your story. What supporting material will make your story stronger? Can you share research data to support your key message(s)? You don’t need to use too many facts, and detailed data – pick the data that is most relevant to your audience to help make your point; for instance, state data would be important to a state legislator, while patient outcome data would be relevant to healthcare professionals. The WHO recommends you use facts and figures wisely – if you use too many it can overload and confuse your audience. Balance statistics with stories that convey the human cost of disease.
You should also use blogs and social media to spread your message to a wider audience. Bear in mind the content that works best on the platforms you have chosen. The continuing growth of visual platforms, such as Pinterest, Snapchat and Instagram means that creating visual content is more important than ever. There is a reason the most widely shared content nowadays is highly visual because visuals can rapidly create an emotional response and convey an idea very quickly. The type of visual assets you can create include images, videos, and infographics.
Insider Tip
Jo Taylor created her own infographic to raise awareness of the signs of secondary breast cancer. There are many tools out there which can help you create appealing images without any design skill. I’ve put together a list of free tools here which you may find useful.
6. Promote Your Message
People are more likely to believe and understand a message heard from more than one source. Promote your key message(s) through social media and encourage people to spread it through their social networks too. Research shows that 69% of people share information because it allows them to feel more involved in the world, and 84% share because it is a way to support causes or issues they care about. By making it easy for visitors to your website or blog to share your content, you increase the likelihood that they will take this action. Make sure your social sharing buttons are clearly visible on your site. This is the most obvious (though sometimes overlooked) way to encourage readers to share your content. By placing the buttons on the side or at the end of the article, people will be more inclined to share the article.
Insider Tip
Use a tool like Click to Tweet in your posts. This useful tool generates one-click tweet boxes or links that can be shared through your website, your blog, or via email, to increase social shares.
Wrapping Up
Raising awareness is the first step on the path to change. Change won’t happen right away and it will require patience and persistence. Siobhan Freeney (@breastdense) founder of Being Dense, an organization which raises awareness of breast density and its associated links to breast cancer and screening, believes “awareness is the precursor to change,” and you need “resilience, research, passion and patience” to succeed. If success feels slow in coming, don’t lose heart. As triple negative breast cancer blogger, Catherine Foy (@mytripleneglife) points out, “without you realizing it, your story may have given hope to someone struggling.” Even if your story hasn’t changed the world, it may, to quote Kay Curtin, “change somebody’s world.”

A Stanford Medicine X e-Patient scholar, Marie Ennis O’Connor is an internationally recognized keynote speaker, writer, and consultant on global trends in patient engagement, digital health and participatory medicine. Marie’s work is informed by her passion for embedding the patient voice at the heart of healthcare values. She writes about the experience of transitioning from breast cancer patient to advocate on her award-winning blog Journeying Beyond Breast Cancer.

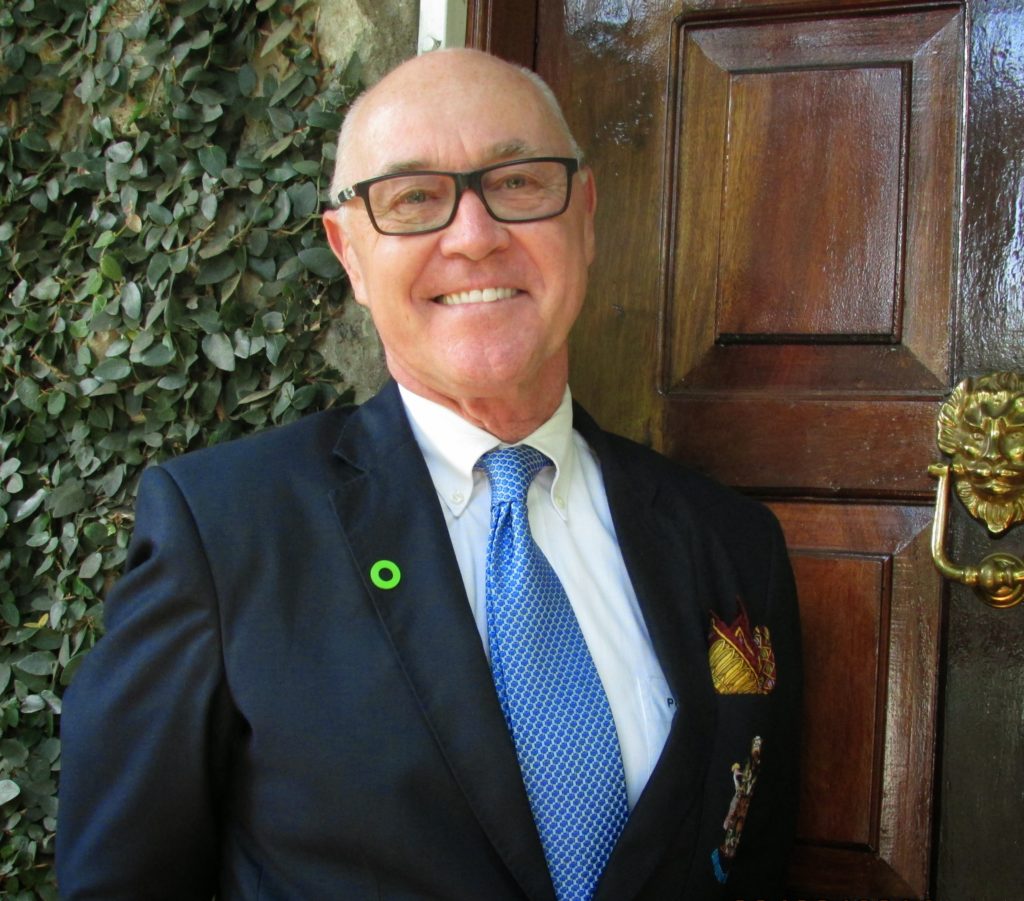 Peter Blaze Corcoran concedes that there is never a good time to get a stage four cancer diagnosis, but he says his diagnosis came at a time in his life when he felt secure in managing it. It was 2015 and he was a university professor nearing retirement. He had insurance, a supportive employer, and access to excellent medical care. “It came at a time when I was mature enough, secure enough, and knowledgeable enough,” says Peter. “I felt quite stable in dealing with it.” It was
Peter Blaze Corcoran concedes that there is never a good time to get a stage four cancer diagnosis, but he says his diagnosis came at a time in his life when he felt secure in managing it. It was 2015 and he was a university professor nearing retirement. He had insurance, a supportive employer, and access to excellent medical care. “It came at a time when I was mature enough, secure enough, and knowledgeable enough,” says Peter. “I felt quite stable in dealing with it.” It was 

