The Power of Positivity: Advice from an AML Patient
The Power of Positivity: Advice from an AML Patient from Patient Empowerment Network on Vimeo.
Casey Marsh, an AML patient advocate, shares advice that helped her through maintain her spirit throughout her diagnosis and stem cell transplant.
Casey Marsh is an AML survivor and patient advocate. Casey is giving back by volunteering for The Leukemia & Lymphoma Society and has been selected as Houston’s honored hero for the 2019 Light the Night.
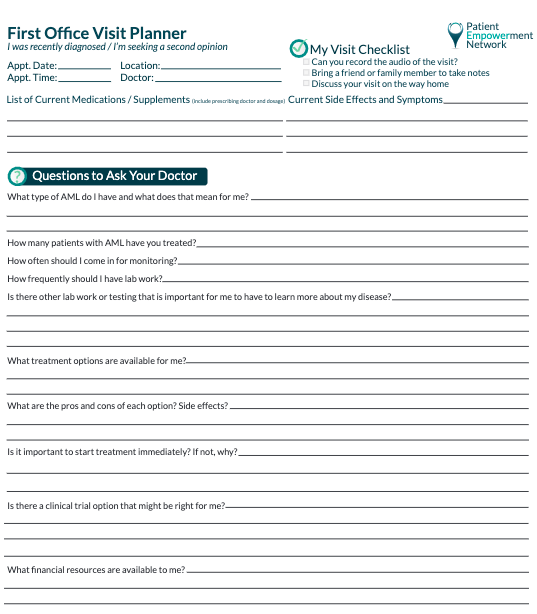
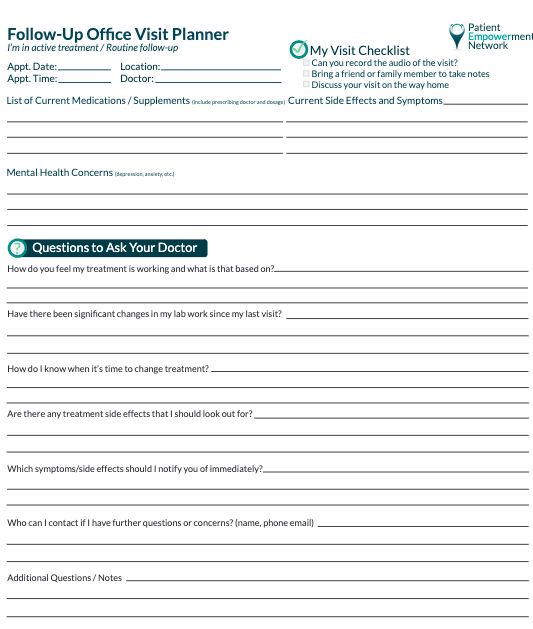
See More From the The Pro-Active AML Patient Toolkit
Related Resources

An AML Story: Casey Shares Her Stem Cell Transplant Experience |

|

|
Transcript:
Casey Marsh:
The three pieces of advice that I would give someone newly diagnosed with AML would be my three power “p” words; the first one being positivity. Having a positive attitude through all of this is key because not every step forward is physical, but it definitely is mental.
So, if you can strive to keep that positive attitude, then everybody else around you will get that same feeling, and it will just help you be competitive and motivated through this whole thing. And the second “p” word would be persevere. Having to persevere through all of that really gives you that encouragement and that strong foundation that when things are bad, you know that they will get better. So, having to persevere through all of that is essential to have.
And then the third “p” word would be the power of prayer. So, whether you have people just talking to their family or friends about your or to whomever they wish, you talking to anybody or even to yourself to me is considered a prayer. So, sending all of those messages just to anybody that will listen is essential because together everybody makes a stronger effort, and nobody will ever have to fight alone.
So, you want to be positive, you want to persevere, and you want to show some sort of prayer.