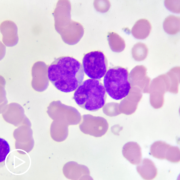
Is It Time to Treat Your CLL? What You Need to Know from Patient Empowerment Network on Vimeo.
When it’s time to move forward with a chronic lymphocytic leukemia (CLL) treatment plan, what determines the best therapy for YOU? In this webinar, Dr. Susan O’Brien, reviews key decision-making factors, current CLL treatments and emerging research.
See More From The Pro-Active CLL Patient Toolkit
Related Resources
Transcript:
Katherine:
Hello and welcome to the webinar. I’m Katherine Banwell, your host for today’s program. Today we’ll discuss how you could work with your physician to find the best CLL treatment path for you. Joining me is Dr. Susan O’Brien. Welcome Dr. O’Brien. Would you please introduce yourself?
Dr. O’Brien:
Sure. I’m Susan O’Brien. I’m the Associate Director for Clinical Sciences at the Chao Family Comprehensive Cancer Center in Orange, California.
Katherine:
Excellent. Thank you. And a note before we begin. This program is not a substitute for medical advice. Please refer to your healthcare team. Many CLL patients start in a period called watch and wait. Would you give us a brief overview of this approach?
Dr. O’Brien:
Sure. The reason that we do watch and wait, or as some patients like to call it, watch and worry, is because many people present asymptomatically. So, for example, it’s very common that a patient might be found to have CLL because they go in for a routine physical and they have a slightly elevated lymphocyte count. So, many people have no symptoms at all. The average age of the disease is about 71.
So, people at the age of 71 often have what we call comorbidities. So, what does that mean? High blood pressure, high lipids, coronary artery disease. So, they also have a lot of comorbidities and even though right now we have great treatments for CLL that are generally well tolerated, all drugs do have side effects. So, if a person feels fine and the disease is not causing any problem in their life, why give them a treatment for it?
Particularly if we think that we don’t have a curative strategy. There may be a cure fraction for a small subset of patients with CLL who are young and have what we call a mutated immunoglobulin gene. But they’re a minority of most patients with CLL. So, what we want to do is keep people alive as long as we can with CLL until they likely die of other causes that people die of as they age. Heart disease, et cetera.
So, if they don’t need any treatment, we don’t want to expose them to the side effects. And some people, if you take all comers, everybody diagnosed with CLL, about a third of people will actually never need treatment for their disease. And so, that’s the idea behind it. That we’re sparing people side effects from treatments when they feel fine and their quality of life is perfectly good.
Katherine:
How do you decide when it’s time to treat?
Dr. O’Brien:
So, it’s very variable because there are different indications from treatment in CLL. When I’m teaching my fellows, what I say to them is you basically treat the disease when it’s causing a problem. There are published guidelines, but they’re guidelines. They’re suggestions about when you might need to treat. But we take into account a number of different things. And in two different people the indications for treatment could be completely different. So, let me give you two examples.
We could have a patient where they have big lymph nodes maybe in their neck, under their arms, in the groin, in the abdomen. And those nodes are getting bigger and bulkier to the point where they’re really problematic. That could be an indication for treatment. Other people might have very small lymph nodes but have very abnormal blood counts. So, their lymphocyte count could be really high. They could be starting to get anemic where their hemoglobin is dropping.
If you get too anemic, what’s going to happen? You’re gonna be symptomatic with fatigue and shortness of breath. So, we want to intervene not at a time when the disease is not causing any problems, but we also have to kind of find a happy medium. We don’t want to intervene – and wait until the patient is sort of bedridden and then start to do anything about the disease.
So, it’s a little bit of a judgement call. We also take into account the symptoms that the patient might be having. Like, are they having really terrible night sweats and fatigue that’s impacting their daily activities? So, we look at symptoms, we look at blood counts, and we look at lymph nodes or bulk of disease.
Katherine:
Where does genetic testing fit into the plan to treat?
Dr. O’Brien:
There are certain tests that we definitely want to do before treatment. And some people have these tests done at diagnosis. So, the two main tests I would say are FISH, which just stands for fluorescence in situ hybridization, which is a fancy word for looking at chromosome abnormalities inside the CLL cell. The other thing we look at is the immunoglobulin mutation status. So, a patient’s immunoglobulin can be mutated or unmutated.
The immunoglobulin mutation status never changes. So, if a patient has had that test done once, they don’t have to have it repeated. However, the FISH, or the chromosome test, can change. So, it’s very important even if it was done at diagnosis that we repeat it at a time when a patient needs therapy. And why that’s so important is there is a particular chromosome abnormality called a 17p deletion where we know that those patients respond very poorly to chemotherapy.
And so, really should never receive chemotherapy and should receive a targeted therapy if that’s the case. There are other people that still could benefit potentially from chemotherapy, but not if they’re in that 17p deletion group.
Katherine:
All right. Dr. O’Brien, once it’s determined that it’s time to move forward with treatment, what do you take into consideration to help guide the treatment choice?
Dr. O’Brien:
Well, the good news and the bad news are kind of the same. The bad news is it’s a very complicated decision, but the good news is the reason it’s complicated is because we have a lot of good options. So, as I said, there are some people for whom chemotherapy would still be an option. One of the benefits of that is that it’s intravenous, i.e. there’s no copays for the patient. It’s administered over a finite period of time. Generally, six months.
And then, most patients will get several years of remission after that where they don’t have to be on any treatment. However, we now have what we call the small molecules or the targeted therapies and those come in two major categories. One is called BTK inhibitors. And there we have two drugs available in the same family, if you will. One is ibrutinib. One is acalabrutinib
And then we have a different category of oral treatment where we only have one drug, which is a BCL-2 Inhibitor, which is Venetoclax. So, what these drugs do, they’re not chemotherapy, but they interfere with certain proteins in the CLL cell. And by doing that, cause the cell to die off.
Katherine:
Okay. What do you feel is the patient’s role in this decision?
Dr. O’Brien:
Well, I think the patient plays a key role, which they usually do when there’s options because then you have – you with your doctor have to make a choice. So, for example, we talked about chemotherapy is time limited and you generally will be done after six months in contrast, with the BTK inhibitors, those are given indefinitely. They’re pills but given indefinitely for several years.
With Venetoclax it’s given with an antibody, which is given intravenously but the Venetoclax can be stopped after 12 months. So, the side effect profiles are different also. So, we have to take into consideration the duration of the therapy as well as the side effect profiles in determining what might be best for that patient.
Katherine:
Well, you talked about chemo and targeted therapies, but where – where’s stem cell treatment fit? Where does – where does stem cell treatment fit in and when is it considered?
Dr. O’Brien:
So, stem cell treatment – if we’re talking about stem cell transplant, allergenic stem cell transplant is a transplant where you need a donor and you receive stem cells from the donor. And that can be a curative therapy, but it can also be associated with significant risks including risk of dying from the transplant. Because we have so many effective therapies nowadays, we’re generally not needing to use allogenic transplant.
And what I mean by that is if these targeted therapies don’t cure people, and the jury is still out on that I would say, if we can sequence them such that we get five years from one, six years from another, et cetera, we’re going to be able to keep the patient alive long enough until they die of something else. So, where the stem cell transplant comes in is generally much younger patients with CLL.
I mentioned the average age is 71, but we have – all of us int eh field have seen patients, for example, in their 30’s. Well, yes, a sequence of therapies might not get that patient to a normal lifespan, because they’re so young to start. So, really the consideration is pretty much reserved for younger patients where we might need a curative strategy that we might not have otherwise.
But for older patients, we probably have enough active drugs now. We have other categories of drugs that we can use if the disease reoccurs. So, we have enough categories of drugs that I think we can keep most people who are the average at CLL alive for quite a long time.
Katherine:
What about CAR-T therapy? Where do we stand on that with that research?
Dr. O’Brien:
So, my answer is a little bit like allogenic stem cell transplant. CAR-T therapy is also associated with significant risks, but also significant benefit. Up until now, it’s pretty much been reserved because of the risks for patients who, to be frank, their disease has now kind of escaped everything. We don’t feel like we have great options that are similar and easier to use.
So, it can be effective, but it’s not something we do very early on because of the associated risks. If you take patients who go for CAR-T therapy, about 25 to 40% of them will wind up with some stay in the ICU. So, I’m really talking about some serious complications from these therapies.
It’s possible that as we learn how to minimize the toxicities of CAR-Ts, that they might become a more attractive strategy. And so, that could change with time. But the counterpoint to that is we’re having new drugs approved all the time for CLL. So, that gives us also more options before we would need to move to a CAR-T.
Katherine:
Dr. O’Brien, where do clinical trials fit in in all of this? Should patients discuss clinical trials with their physicians?
Dr. O’Brien:
Absolutely. If we think of these great drugs that we have now, and I’ve mentioned ibrutinib, acalabrutinib, Venetoclax. Before those drugs were available, the only options were chemo. So, that means that people that went on the clinical trial, so let’s say with ibrutinib, have access to a really treatment changing revolutionary drug in CLL years before it was commercially available.
So, clinical trials can be a great way to have access to drugs or combinations. So, for example, right now there are some clinical trials looking at combinations of a BTK inhibitor and a BCL-2 inhibitor. So, the patient might say, “Well, why can’t you give me that combination, doctor?” “Well, technically I could.” If the drug is approved by the FDA, a physician can prescribe it really pretty much anywhere they see fit.
However, does insurance pay for it? That’s the trick. And these are very, very expensive drugs. And so, outside of an FDA approved combination, it probably wouldn’t – I wouldn’t be able to prescribe that combination because it wouldn’t get paid for and it would cost thousands and thousands of dollars. But on a clinical trial in general, the drugs are paid for.
Katherine:
Mm-hmm.
Dr. O’Brien:
And so, clinical trials are testing, for example, combinations now, which are not standard and there are some preliminary data from some of these trials that look really promising, i.e. two drugs may be better than one. There are also patients who, perhaps we’re talking about younger patients now, who have kind of worked their way through the available therapies. And so, they might not have a standard therapy that’s really gonna work for them. And for whatever reason they might not be a good candidate for stem cell transplant.
And so, innovative or totally novel drugs that we don’t have that class of drugs available at all are also being tested in clinical trials and allow people access to them. So, sometimes it’s – I think some people think of it as, well, a last resort if the drugs that are out there don’t work. But don’t think of it that way, because as I mentioned, these combination trials are for people who’ve never had prior therapy, but their disease has progressed enough to need treatment and could potentially offer, at least at a preliminary level, looks like a dynamite combination of drugs.
So, it’s not just for people who failed other drugs or whose disease has failed other drugs. That could be one group that is particularly important for, but even patients who’ve never had treatment, there may be clinical trials that they would be highly interested in participating. And again, it generally has a big financial benefit too, because remember oral drugs have copays for cancer patients.
Katherine:
Right. But how is that treatment monitored to evaluate its effectiveness?
Dr. O’Brien:
Well, generally the things we’re – the same things we’re look – the same things we’re looking at when we treat. Right? So, we’re looking at abnormal blood counts. We’re looking at enlarged lymph nodes or spleen. We have symptoms. So, those three things are looked at when the patient is on the therapy. Are the lymph nodes shrinking? Are the blood counts improving? Are their symptoms getting better?
So, the same way pretty much that we would follow a patient who’s not on a clinical trial is the way we follow them on a clinical trial. Now, if it’s a very new drug which has never been given to humans before, let’s say, those trials probably have more frequent surveillance than we might do with a drug that we are familiar with and know what to expect with it. So, sometimes the trials might have more surveillance, more visits, more tests.
But generally, if those tests or visits are required – are not considered standard of care, the companies pay for them. So, usually what’s billed to the insurance is only what we would do treating any CLL patient with an already available drug.
So, it doesn’t wind up costing the insurance or the patient any more to be on a clinical trial. And they might get actually – there is some data the patients on clinical trials get better care because they’re being monitored very carefully as part of the trial.
Katherine:
Let’s turn to patient self-advocacy. How can patients feel confident in speaking up and becoming a partner in their own care?
Dr. O’Brien:
Yes, obviously for some people that’s going to be a lot harder than others. What I generally advice people is if you’re going in for your physician and you’re diagnosed with CLL, I would say this for any cancer because cancer is obviously a potentially life changing diagnosis, is you probably want to get an opinion with an expert. I would talk to my doctor first, ask them what their plan is so I know, and then see an expert in the field.
Then if the expert in the field says, “I think your doctor’s plan is great.” 1.) you’re now comfortable because you’ve got a second opinion, and 2.) that’s also a way, in my experience, to know if your doctor’s really gonna allow you to have an easy time participating. What I mean by that is that if your doctor is upset or finds it offensive, quite frankly you probably need a new doctor. That’s my take on that. Because that means they’re not going to be too open to your comments or you’re saying, “Well, I would prefer to do this.”
That’s just my quick take on how you can tell if it’s going to be easy or hard. But I think the relationship between the doctor and the patient is very important and you have to establish that relationship early on. If you go to a doctor who – where you start to ask questions and they’re in a hurry or they’re looking at their watch, you know that’s probably not the doctor that you want. I think most doctors realize that if they’re diagnosing a patient with a cancer, that’s going to be a pretty long clinic visit, because any patient is going to have a lot of questions to ask.
I also tell patients when you go to see a specialist or get a second opinion, bring somebody with you. It’s very well known that when patients have just been diagnosed with a cancer, they’re overwhelmed. Their emotional system is overwhelmed. Even if it’s “not a bad cancer”. Maybe early stage CLL. And that makes it very hard to process what a doctor is saying.
Particularly if they’re trying to give you quite a bit of information, which you need because you’ve just been diagnosed, and you need to know what to expect from the disease. So, having a friend or a spouse or a significant other there is really, really helpful.
Katherine:
Yeah. Yeah. That’s really good advice. Are there resources to help patients stay informed and educated?
Dr. O’Brien:
Oh, yes. Our Leukemia and Lymphoma Society is great at that. Lymphoma Research Foundation were two of the big ones. And then there’s patient spots. CLL Society is a very well-known one run by a physician who’s also a CLL patient. I know him very well. And they have online support meetings now.
They used to have them in person, but now they have them online. And those can be really helpful because that allows a patient to talk to another patient who has their same disease. So, there are quite a lot of resources for patients nowadays. Especially in our technology enabled world.
Katherine:
That’s great. We have a couple of questions from patients. Patrick asks, “I’ve discussed a treatment plan with my doctor, but I’d like to get a second opinion. What are your thoughts on that?”
Dr. O’Brien:
I think it’s a great idea. That’s exactly what I would do if I had a cancer. And again, I think Patrick made an important point that I’d like to emphasize. See what your doctor’s plan is first. Because then when you go to see the specialist or the second opinion, you can say, “This is what my doctor’s suggesting.”
And then if the specialist says, “Exactly what I would do.” But if you don’t know what your doctor is going to do – was suggesting to do when you go in to see the second opinion, it’s going to be really hard to make sure –put together that feeling of confidence that you’re on the right track.
Katherine:
Right. Right. To judge. A question from Julie. “How do you approach treating a relapse?”
Dr. O’Brien:
So, treating relapse we do the same thing that we do upfront. Namely “watch and wait”. So, for example, if a patient had a treatment on – let’s say they had some chemotherapy. And three or four years alter the lymphocyte count starts to go up, well, that technically would be indicating relapse.
But let’s say for the sake of discussion the person is asymptomatic, they feel fine, and their lymphocyte count is 20,000. Well, why do we need to do anything? So, in most cases we take the same approach of watch and wait when the disease comes back. And the first point at which it comes back is not always the time at which we need to initiate therapy.
Katherine:
Right. Right. Another question. Will is wondering, “If inhibitor treatments have to be taken forever?”
Dr. O’Brien:
Well, it depend on the group – the class. So, for the BTK inhibitors, all the trials so far have given those drugs indefinitely. For the BCL-2 inhibitor, Venetoclax, there are time limited regimens both in the frontline setting and in relapse. But realistically, I have talked to my patients who are going on a BTK inhibitor who say to me, “Do I really have to be on this forever?”
And so, my answer is, “I don’t know what life is forever, so I would never use that word. We generally use the word indefinite.” But what I’ve said to those patients is, “If you’re on the drug for a while – and I’m not talking months. I’m talking say two, three years. And you’re in a really good remission and you think you want to stop treatment. I’m not necessarily opposed to that.”
Because if you’re in a very good remission, even if it’s not complete, but most people who are not in complete remission, meaning they still have a bit of disease left, have very little disease if they’ve been on the BTK inhibitors for a while. So, maybe only some enlarged lymph node on a CAT scan or a little bit of disease in the bone marrow.
But basically, most people after a couple years, they’re blood counts are normal, they feel fine, unless they’re having side effects from the drug and their physical exam is normal. So, I’ve told my patients if you want to go off, I expect you’d probably be off for even a couple years. And then we could always restart therapy potentially with that drug again or with one of the other drugs.
So, I think it’s important to let people know that they have options. But I will say that all of the clinical trials with the BTK inhibitors have given those drugs basically until the patient loses their response or there’s a toxicity where they just don’t want to take the drug anymore.
Katherine:
Mm-hmm. Mm-hmm. One last question from Jen. “What should be considered related to side effects when choosing a treatment plan?”
Dr. O’Brien:
Well, the BTK inhibitors have some side effects. They can cause diarrhea, but that’s usually mild and self-limited. They can sometimes cause joint aches or arthrology. They – the two probably most serious side effects are atrial fibrillations, which is an irregular heart rate. But that generally is not frequent and tends to occur mainly in older men with heart disease.
Katherine:
Hmm.
Dr. O’Brien:
They also are more likely – they impact the platelet function. So, they can more likely cause bleeding, but it’s typically minor bleeding like a bruise. Major bleeding is quite rare. In general, I’m outlining a lot of side effects, but remember not all side effects occur in everybody and there’s some people who don’t have any.
For the BCL-2 inhibitor, Venetoclax, one of the things we have to be very careful of when a person first goes on that and this would be particularly true if they have a very high lymphocyte count or a bulky lymph nodes, it that drug can cause something called tumor lysis. Tumor lysis, lysis is just a fancy word for breakdown, is where the disease responds so rapidly that their lymph nodes shrink very quickly. Lymphocyte comes down, which sound really good.
But what can happen is that breakdown of the cells can release potassium which can cause heart arrythmias. The cells can clog the kidneys and cause kidney failure. So, we have to be very careful about that when we start. And the way that drug is started is it comes with a starter pack actually to help make it easy where you go up, you start at a low dose, and go up weekly until we get to the target dose.
But we have to monitor very carefully during that escalation phase. The other thing that the Venetoclax can cause is neutropenia, meaning low neutrophil counts. What – that’s important because neutrophils are what we use to fight infection. So, if we get low neutrophil counts, the options are either to add a growth factor transiently, in other words a shot to – the subcutaneous injection that stimulates the bone marrow to release neutrophils. Or if it’s really a persistent problem, then we can go down on the dose of Venetoclax.
Katherine:
All right. How do you feel – how do you feel about the future of CLL treatment? Are you hopeful?
Dr. O’Brien:
Absolutely. I think we’ve had something like six drugs approved in the last seven years, which is mindboggling. I think in the 30 years before that, we didn’t even have six drugs approved. That’s how rapidly – it’s mindboggling, really. That’s how rapidly the field is moving forward. And not just CLL, but other cancer fields also are moving at a very dizzying pace.
Which is great because that – anything that gives us more options is wonderful. So, I am very, very optimistic about CLL going forward. And I’m also very hopeful that some of these combination regimens might actually be – small molecules might actually be curative in the long run. But I will say it’s way too early to know that.
Katherine:
Are there emerging treatments that patients should know about?
Dr. O’Brien:
So, one of the categories we haven’t talked about, where there actually are two FDA approved drugs, are PI3K inhibitors – that’s another oral small molecule. They’re not approved for frontline therapy. So, that’s kind of why we weren’t talking about them so much today where we’re talking about making a choice for the first therapy. But they are approved for patients where the disease reoccurs.
And there’s two of those as we mentioned. We have antibodies, which we really haven’t talked about very much, and then there’s new classes of drugs that are being explored in clinical trials. So, for example, there are interesting drugs which are antibodies that bind to the patient’s own T-cells and they also mind the CLL cells and they redirect the T-cells towards the CLL cells.
Kind of like CAR-T but inside the body without having to take out the T-cells. So, those are really interesting class of drugs. None have been yet approved in CLL or lymphoma, but I think those are on the horizon and looking very promising.
Katherine:
Hmm. One last question, Dr. O’Brien. In this uncertain time, do you have any advice related to COVID-19 for CLL patients?
Dr. O’Brien:
It’s a hard time for everybody and particularly CLL patients because we know that they’re immunocompromised by – and even if you’ve never been treated and you probably never get any infections, which is quite a number of people with CLL, unfortunately you do have to think about yourself as being a high-risk patient.
So, masks are very important. Washing hands. Avoid – social distancing. Avoiding crows. It’s really important for patients with CLL to follow those same guidelines that we’re giving to everybody. But very important for them because they are in a higher risk group.
Katherine:
How do you feel telemedicine is working for CLL patients?
Dr. O’Brien:
Telemedicine works I’d say better for CLL patients than some other patients, particularly watch and wait patients. Obviously the one thing that we can’t do in telemedicine is a physical exam. But in patient we can get – have patients get their blood counts done and then talk to them and see how symptomatic they are and know what their blood counts indicate anything is changing.
And then what I’ve been doing is, say I have a watch and wait patient – or it also applies let’s say to a patient who’s been on ibrutinib for years now and they’re in remission. There’s probably nothing to exam anyway. Right? So, those patients are good. I think it’s not going to work very well if you’re starting a new treatment. But for people who are watch and wait or have been on established treatments that are doing well, it works really well.
And then you can use the video visit if the patient says, “This is going on.” Whatever it is. “And I think I’m worried about this or I have this pain here.” Or whatever. If that’s an issue, you can always then schedule a regular visit. Right?
But I think that it – because it’s a chronic disease as opposed to acute leukemia where you really can’t do video visits, I think it lends itself to it very well. And my expectation is that moving forward, even after hopefully COVID has died down or we have a vaccine, that video visits are definitely here to stay.
Katherine:
Yeah. Yeah. I agree with you. What about patients who are fearful going into a medical center? Do you have any advice for them?
Dr. O’Brien:
Usually – and it does vary. I also would be nervous if it was a hospital-based place where I had to go for my visit. But for example, where we are in the cancer center, it’s a completely separate building. Everybody is temperature checked before they get in. Everybody has to fill out a questionnaire about their symptoms. If they do have a low-grade temperature, we immediately triage them to another area.
So, actually I think the cancer center is probably a pretty safe place to be. Probably safer than the grocery store in that sense, because of the screening and the testing of the temperature of everybody who comes in there. And, of course, everybody has a mask on.
So, I would be probably a little bit weary in a hospital setting where they may be many sick patients hospitalized with COVID. But I think in a lot of clinic buildings or freestanding buildings, I probably would not be that worried.
Katherine:
Well, Dr. Susan O’Brien, thank you so much for joining us today. And thank you to all of our partners. To learn more about CLL and to access tools to help you become a proactive patient, visit powerfulpatients.org. I’m Katherine Banwell. Thank you so much for joining us.

 How Do You Know If Your CLL Treatment is Working?
How Do You Know If Your CLL Treatment is Working? Key CLL Treatment Decision-Making Factors
Key CLL Treatment Decision-Making Factors