Social media is a powerful addition to our patient advocacy toolbox. We can use it to raise awareness of our cause, build a community of supporters, promote our key messages and highlight our patient advocacy activities. To help you strengthen your online presence and create more visibility for your cause, I’ve put together this list of ten actionable tips you can put into practice right away.
1. Optimize Your Social Profiles
Your social media profile should be considered a key element of your advocacy brand. What will people’s first impression be of you when they encounter your online profile? What might make them decide to follow you? Review each of your existing social profiles with the following points in mind.
- Is it time to use a more professional picture to represent yourself online? Upload an image that is clear and easy to see, like a head and shoulders shot, or your organization’s logo. Make sure to upload images with the correct dimensions for each social platform (check out this guide to social media image sizes).
- You have an opportunity to personalize your profile on Facebook and Twitter by uploading a custom header image. Use this opportunity to bring more authenticity to your account, for example you might use a picture of yourself holding a sign with a hard-hitting message. Or perhaps there’s a project or campaign you are currently working on. If so, include an image to represent this in the header space.
Take Action: Complete all sections of your profile to convey a stronger message and identity. Schedule a review date every few months to check your information is still current.
2. Focus on Being the Expert One Platform at a Time
Each year brings shiny new social media tools and new features for existing tools. It’s tempting to jump on board the latest social media platform with the aim of being everywhere at once; but rather than spreading yourself too thinly, focus on mastering one or two platforms really well before moving on to the next one.
Take Action: Look back on the past six months and ask yourself which social media platform worked best for you? Which gave you the most engagement? And which platform had the least engagement? Consider focussing your efforts on the high-performing platform and becoming known as the go-to expert on this channel before adding anything new to your social media mix.
3. Schedule Your Social Media Posts
The internet is global and if you want your message to reach further than your own backyard, you need to hit multiple time zones. Tweets have the shortest lifespan of any social media post. Even though the latest Twitter algorithm means that posts are no longer displayed chronologically, Twitter is fast-paced, and messages get buried quickly. To counter this, you need to share your post multiple times on Twitter to increase visibility. Scheduling tweets allows you to reach followers when they are most likely to be online (even if you aren’t there at the same time) and allows you to maintain a regular and consistent online presence.
Take Action: Use a scheduling tool like Buffer or Hootsuite to schedule your updates to reach more people, more often. Don’t just post the same update every time. Vary your updates by changing around the headline, highlighting a statistic or quotation or adding different images.
4. Curate Content
The ability to curate credible content to share with our communities is a key skill for patient advocates. Hereditary cancer advocate, Amy Byer Shainman believes “patient advocates not only have a responsibility to curate trusted content but that it is an imperative if you are even going to be calling yourself a patient advocate.”
Content curation is defined as the process of gathering information relevant to a particular topic or area of interest. While this definition sounds simple, there’s a world of difference between simply gathering information and being an effective curator. A good curator knows how to find, aggregate, and synthesize reliable information, putting it into context for their communities and sharing it in a format that is easy to access and understand.
Take Action: Set up Google Alerts for the healthcare topics of interest to you. Google Scholar is also useful as it indexes most peer-reviewed online journals of Europe and America’s largest scholarly publishers.
5. Create Visual Impact
You’ve surely heard this before, but it’s worth reiterating: images matter — a lot. In an age when people’s attention span averages 8 seconds (that’s shorter than a goldfish!) visuals are memorable and effective because they help people process, understand, and retain more information more quickly.
Visual content is 40x more likely to get shared on social media than other types of content according to research by Buffer. Furthermore, people connect more emotionally with images than text, and in an increasingly crowded digital landscape images can break through the online content clutter. The type of visual assets you can create include images, videos, infographics, quotes and GIFs.
Take Action: Add an image to all your online posts — even those that are text-based. Create a strong visual identity and maintain consistency across all your images by sticking to the same colours, fonts, and layouts. Read How To Create Professional Graphics — Even If You’re Not a Graphic Designer for more tips.
6. Use Relevant Hashtags
Hashtags are a powerful way to increase your visibility on social media. According to Twitter’s own research tweets with hashtags show a 100 percent increase in engagement (clicks, retweets, likes and replies). Jo Taylor, a moderator of the UK-based breast cancer Twitter chat #BCCWW, explains that “finding disease hashtags opens up connections. If you connect with others you will be able to meet others easily online and you will build and learn from there.”
Take Action: Visit symplur.com to find the relevant hashtags for your disease area. If you can’t find a hashtag related to your topic, you might consider creating your own. For more information on using hashtags strategically read Everything You Ever Wanted To Know About Hashtags in Healthcare…But Were Afraid To Ask!
7. Live-Report Conferences and Events
Reporting live from an event is a way of engaging your followers by sending updates about an event as it occurs. It allows you to expand the reach of in-person events to provide valuable insights to those who are unable to attend in person. It’s also a way to increase your visibility as an attendee and enhance your credibility.
Live reporting tools include live-streaming using Facebook Live, Instagram Live, and Periscope (Twitter’s live-streaming app). You can also share posts to your Facebook page and share photos and video clips via Instagram and Snapchat during the event.
Take Action: Read The Advocate’s Guide to Reporting Live from Conferences and Events for more tips on live-reporting.
8. Take Part In Twitter Chats
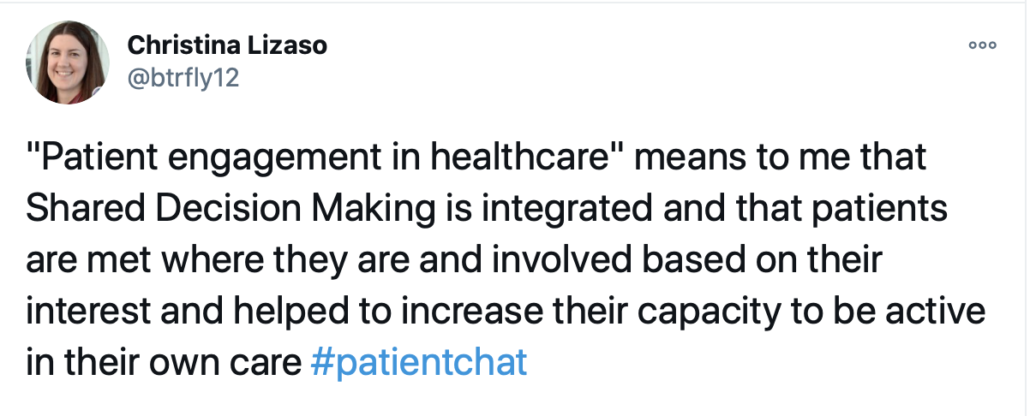
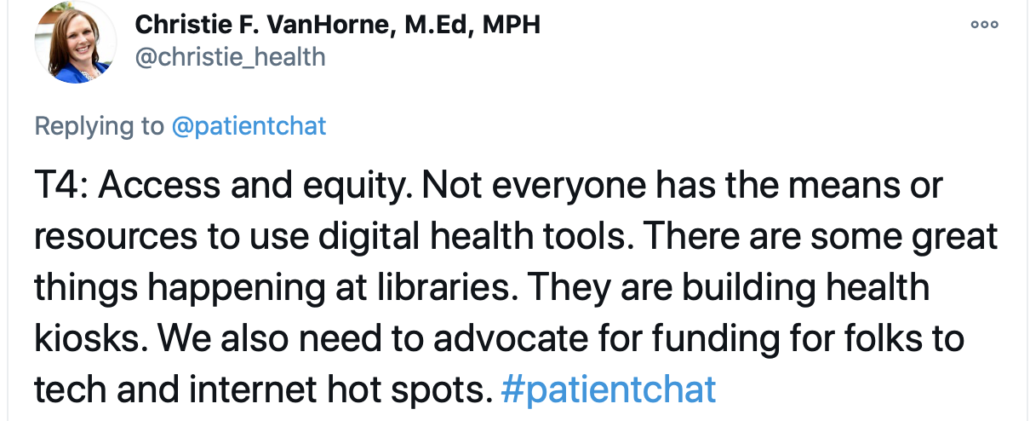
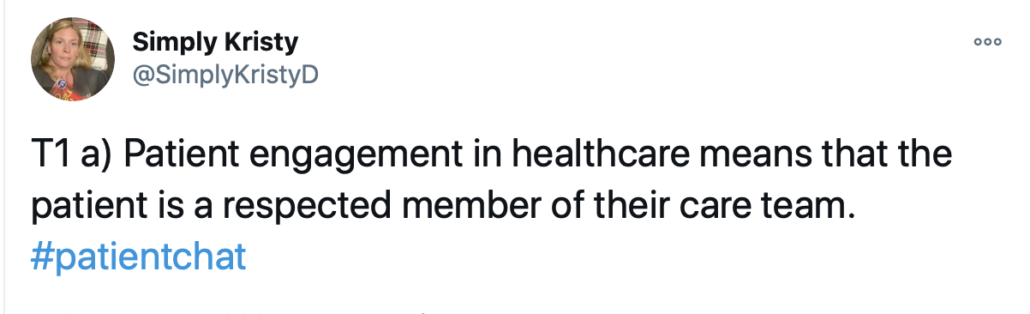
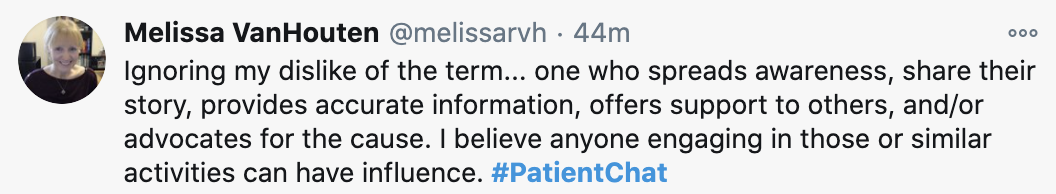
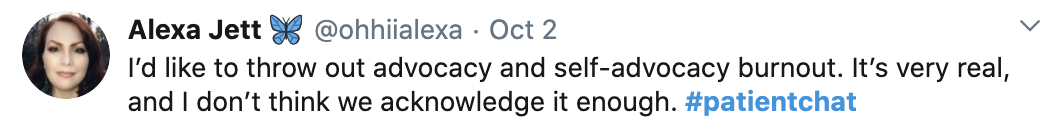
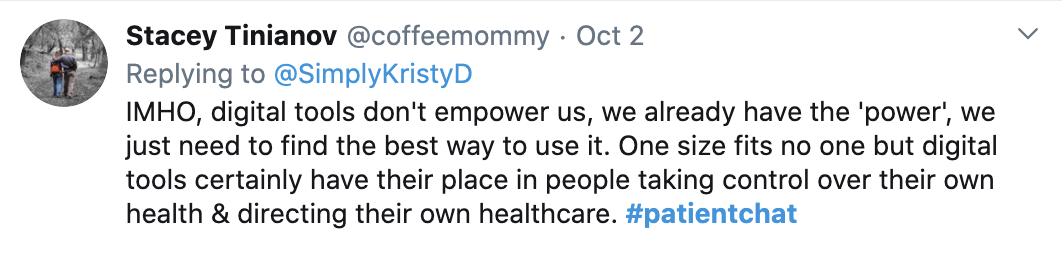
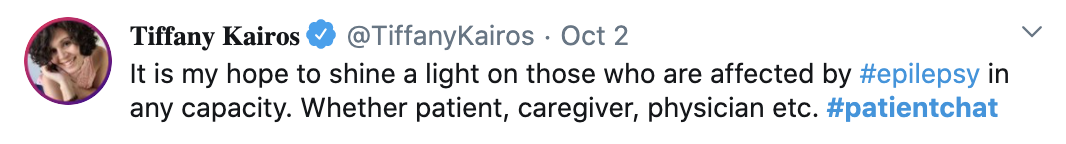
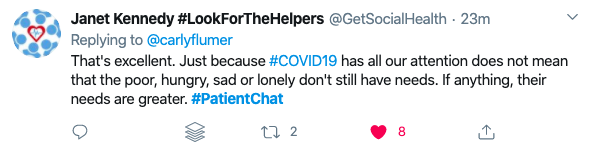
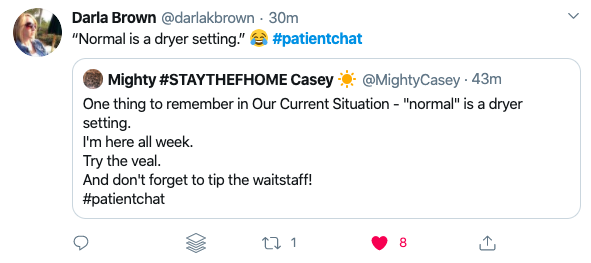
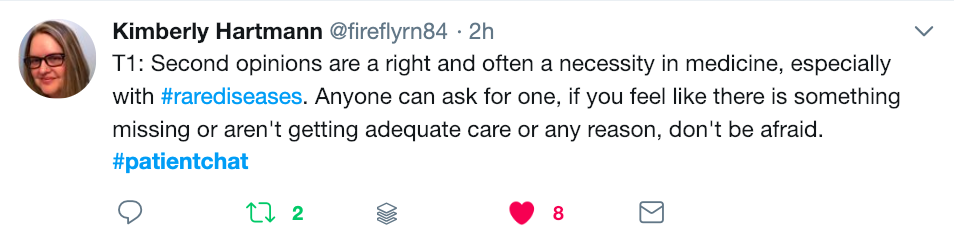
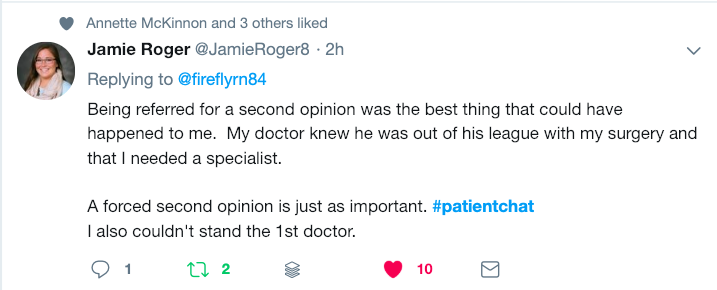
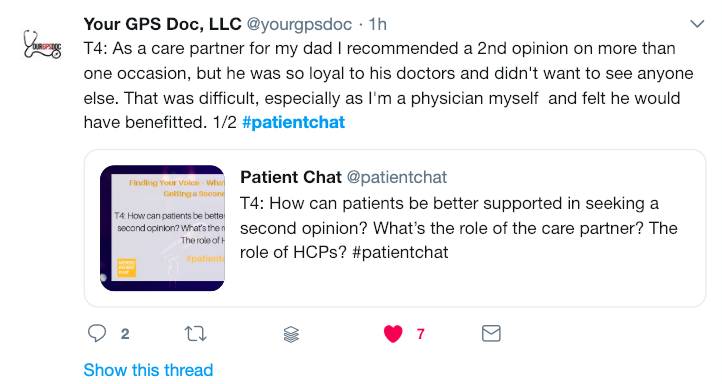
Twitter thrives on its community and the more you connect with other users the more quickly you will grow your own following. Joining a Twitter chat is a super way to connect and engage. When you attend a Twitter chat regularly, people will get to know you and in this way, you can quickly develop and grow your own network of supporters. If you’re not familiar with them, a Twitter Chat is a public Twitter conversation around one unique hashtag. This hashtag allows you to follow the discussion and participate in it.
Twitter chats can be one-off events, but more usually are recurring weekly chats to regularly connect people, for example #PatientChat held every other Friday at 10:00 am Pacific/1:00 pm Eastern. The chat will be hosted and the host will ask questions along the way to stimulate discussion and sharing of ideas. There are chats for most disease topics and a full list can be found by searching the database of the Healthcare Hashtag Project. This is also a useful resource to find Twitter users to follow. In addition you will find past transcripts of chats on the website so you can familiarize yourself with the chat and its norms before taking part.
Take Action: There are chats for most disease topics and a full list can be found by searching the database of the Healthcare Hashtag Project. And “if you can’t find a tweet chat you enjoy,” recommends patient advocate, Annette McKinnon, “start a new one, register it @symplur and build a new community.”
9. Create a YouTube Channel
People engage with video more than any other form of content (written, audio, images, etc.). YouTube with more than 1.8 billion monthly active users remains the online video leader. 4 million YouTube videos are viewed every day, and the average session duration of 9 minutes and 28 seconds. That’s more than many other social networks.
Take Action: While producing your own video may seem daunting, video creation has never been more accessible through smartphones. You can also create simple videos for your channel using free tools such as Adobe Spark and Lumen5 (see my YouTube channel for examples of Lumen5 videos).
10. Maintain a Consistent Content Creation and Promotion Schedule
Social media is an ongoing commitment. You need to post consistently to stay in front of your audience’s eyes and keep growing. One key to maintaining a steady stream of quality content is to re-purpose what you already have. Check your blog’s analytics (or Twitter and Facebook analytics) to see the most popular posts you’ve written or shared. Can you expand on these to include new research or thinking? Perhaps the content can be turned into an infographic or a slide-deck.
Take Action: Set aside one day each month to map out upcoming cause awareness days. Then use a simple excel spread sheet to create a calendar for social media postings. Include relevant hashtags and images. A content calendar helps you maintain a consistent content production schedule, enabling you to plan for seasonal content, and annual campaigns.
Social media is an ever-evolving and fast-moving field, and with so much to learn and do, it’s easy to feel overwhelmed. You don’t have to implement all these tips at once. Try adding one new strategy to your social media plan each week and measure its impact at the end of each month. This way you will know which of these strategies are moving you closer to a stronger online presence.
Here’s to your social media success!
A Stanford Medicine X e-Patient scholar, Marie Ennis O’Connor is an internationally recognized keynote speaker, writer, and consultant on global trends in patient engagement, digital health and participatory medicine. Marie’s work is informed by her passion for embedding the patient voice at the heart of healthcare values. She writes about the experience of transitioning from breast cancer patient to advocate on her award-winning blog Journeying Beyond Breast Cancer.