Cancer.Net®: Doctor-Approved Patient Information from ASCO®
Head and Neck Cancer: An Introduction
What is Head and Neck Cancer?
Ezra E. W. Cohen, MD, FRCP, Member, American Society of Clinical Oncology:
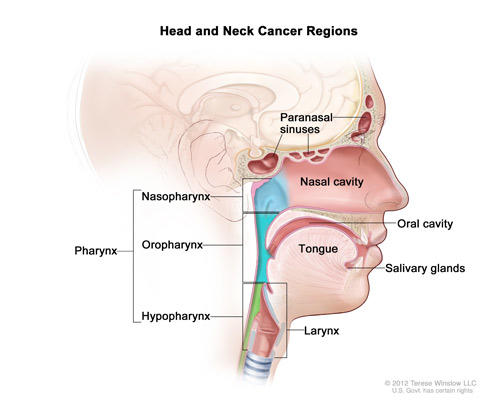
When we think about head and neck cancer, we are really talking about diseases or cancers that occur essentially above the clavicles, but not including the brain. Brain cancers are really a different entity. So these are cancers that start in the mouth or the throat. Often we see patients with cancers that originated in the thyroid gland or the salivary glands.
Essentially, that part of the body that is responsible for speech and swallowing, communication. And most of those cancers start on the surface, what we call the mucosa of those areas, the lining of the mouth or the throat or the tongue.
Types of Head and Neck Cancer
Dr. Cohen:
The primary types of head and neck cancer we really put into, I think, three major categories and they are based on their origin in terms of the tissue. So the main type, and I would say this accounts for 90 percent of the cancers that we see, we call squamous cell carcinomas. Those are cancers that start in the lining of what we call the upper air digestive track, so the mouth, the throat, the upper esophagus, the voice box or larynx, the upper trachea. Those are all lined by a mucosal surface that when there is a cancer from it, we call those squamous cell carcinomas.
Then the second most common are thyroid cancers, they come from the thyroid gland. Those fall into a couple of categories, either medullary thyroid cancer or what in broad terms what we call differentiated thyroid cancer. And then the third category that we see most often are cancers that start from the salivary glands or salivary gland cancer.
Potential for Cure
Dr. Cohen:
When we think about a head and neck cancer diagnosis and when a patient gets a diagnosis of head and neck cancer, one of the things that they need to begin to think about are what their potential for cure is and potential for organ preservation.
Let me expand on both of those. In terms of this disease, the majority of patients that we see present with what we call local regional disease. And what we mean by that is that they have a tumor that often has spread to lymph nodes, but has not spread widely. So no metastases to other organs like the lungs or the bones or the liver and what we are really talking about is disease that is confined to the area of the head and neck.
And that’s important because those patients we would consider for curative intent therapy. We are going to try to cure that disease. And that becomes obviously incredibly important to both the patient and the physician. And the first thing that we think about when we see a patient with head and neck cancer is, is this a patient that can be cured of their disease.
If they are, that obviously takes us down a road of what we can do to cure that patient. And if they are not, that takes us down a completely different therapeutic avenue. Then we begin to think about well, as you can imagine, because the organs of the head and neck are so critical to day to day interaction, to really what defines us as human beings – our ability to talk to each other, our ability to have a meal, to eat normally, our facial expressions. So much of what we do as people, as humans happens above the clavicles.
And so functional preservation becomes so important in patients with head and neck cancer, especially ones that we are going to try to cure. So the next question that we ask is how can we cure this patient and return them to normal function. And that is exactly the questions that patients should be asking their physicians. Do I have, can I be cured of this and if I can be cured of this, how can I maintain my normal activity once I am done with therapy?
And then we need to think about what are the other medical professionals that are going to be important in this person’s care. So because many patients have, will get radiation to the mouth or the oral cavity is going to be included in the radiation field, dentists and dental professionals become incredibly important to the ongoing care.
You can imagine that as we, as patients go through therapy they are going to have trouble swallowing. So nutrition and speech and swallow therapists become incredibly important.
Treatment Options
Dr. Cohen:
Going back to the idea that many of our patients will present with local regional disease, the main treatment option really focuses on curing these patients. And when we talk about curative intent therapy, we are really talking about three major modalities – surgery, radiation therapy and medical oncology or chemotherapy.
And what we’ve done really for the last couple of decades is learned how to integrate those three modalities to produce the best outcomes possible. For some patients it is going to be surgery upfront, possibly followed by radiation or chemotherapy and radiation. For other patients, we want to, and for many patients, we want to think about a non-surgical approach in an attempt to preserve function and preserve the organ.
And then lastly, I do believe it’s very important to ask about clinical trials. Because not only is this the way that we move the field forward, but honestly, clinical trials offer novel therapies to patients, new approaches to patients that very often prove to be the next standard of care, especially now with the excitement around immunotherapy. So I think it is very important to ask what clinical trials are available to me for the disease that I have.
Beyond that, I think the important things to ask are what should my caregivers be thinking about, what support team do I need to have in place. And it is good to think about that proactively and get that in place. How much help will I need as I go through this treatment and who is going to be available to supply that help.
Latest Research Developments
Dr. Cohen:
When we think about where the research is going and the most recent research advances in head and neck cancer, I really like to group them into two categories. The first is what we are learning about the cancer and our better understanding of really the biology of this disease. And the second falls into what are the new therapies, what treatments are coming online or about to come online that we can take advantage of to improve outcomes for patients.
But we are learning that clearly there are two distinct types of squamous cell carcinoma, the head and neck. One is related to a virus called human papilloma virus or HPV, the same virus that causes cervical cancer and some other cancers. And we are understanding that HPV related head and neck cancer behaves a lot differently than non-HPV related head and neck cancer.
And what I mean by that is the patients tend to be younger, they are often non-smokers and non-drinkers. And that is a real, that is a very important thing to point out. Because we are learning as practioners is that patients don’t need to smoke to be at risk for head and neck cancer. And in a non-smoker, we need to be still concerned if somebody begins to complain of symptoms around the head and neck area, pain, a lump in the neck. We need to be very concerned and begin to think about is this possibly a viral related cancer, even in a non-smoker and patients, of course, should be aware of that as well.
So HPV positive head and neck cancer behaves differently. And then HPV negative cancer, which is often related to tobacco exposure, occurs in patients who are a little bit older. It has a different presentation in terms of where it occurs, it often occurs in the voice box or the oral cavity. And again, it is often associated with, especially cigarette smoking.
We have also begun to understand that there are mutations and alterations that we can target specifically. So for instance, there are patients who have mutations in certain pathways or in certain genes that now we have drugs that specifically target those genes.
We have also begun to understand that immunotherapy is going to play an incredibly important role in this disease for both HPV positive and non-HPV related head and neck cancer. And that we are seeing some incredibly exciting data with the first wave of immunotherapy drugs in this disease. In fact, now we have randomized data of an immunotherapy drug versus standard of care in patients that are current in metastatic disease that are showing a dramatic improvement for immunotherapy.
And truly, this is just the first step, the first drug that has shown this type of efficacy. We are going to see many, many more in the next few months and an explosion, really, in the next few years for immunotherapy in head and neck cancer.
Where to Get More Information
Dr. Cohen:
For head and neck cancer, there’s some especially relevant websites that would be worth looking into. Cancer.Net is a site designed by the American Society of Clinical Oncology specifically for patients to address patient questions, patient needs, caregiver questions and needs. And it’s really geared towards the patient. So Cancer.Net would be certainly one of those.
[Closing and Credits]
Cancer.Net®: Doctor-Approved Patient Information from ASCO®
ASCO’s patient education programs are supported by Conquer Cancer Foundation of the American Society of Clinical Oncology. ConquerCancerFoundation.org