Could a Clinical Trial Be Your Best Cancer Treatment Option? from Patient Empowerment Network on Vimeo.
Is a clinical trial right for you? Cancer expert and researcher Dr. Seth Pollack is joined by PEN board member and empowered patient, Sujata Dutta, to discuss key information about clinical trials. The guests review clinical trial terminology, debunk common misconceptions about trials, and Sujuta shares her own story of participation in a clinical trial.
Dr. Seth Pollack is Medical Director of the Sarcoma Program at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University and is the Steven T. Rosen, MD, Professor of Cancer Biology and associate professor of Medicine in the Division of Hematology and Oncology at the Feinberg School of Medicine. Learn more about Dr. Pollack, here.
Sujuta Dutta is a myeloma survivor and empowered patient advocate, and serves a Patient Empowerment Network (PEN) board member. Learn more about Sujuta, here.
Download Guide
See More from Clinical Trials 101
Related Resources:
Transcript:
Katherine Banwell:
Hello, and welcome. I’m Katherine Banwell, your host for today’s program.
Today we’re going to discuss clinical trials, what they are and how they work, and debunk some misconceptions along the way. Before we get into the discussion, please remember that this program is not a substitute for seeking medical advice. Please refer to your healthcare team about what might be best for you. All right. Let’s meet our guests today. Joining me is Dr. Seth Pollack. Dr. Pollack, welcome. Would you please introduce yourself?
Dr. Seth Pollack:
Yeah. Thanks so much. It’s a pleasure to be here, my name is Seth Pollack. I’m a medical oncologist here at Northwestern University Medical Center.
And I specialize in treating patients with cancer, and I have a specific interest in patients with a type of cancer called sarcomas.
Katherine Banwell:
Excellent. Thank you for taking the time to join us today. And here to share the patient perspective is Sujata Dutta, who is on the board of the Patient Empowerment Network and is currently participating in a clinical trial. Sujata, it’s a pleasure to have you with us.
Sujata Dutta:
Pleasure to be here Katherine. Hello, Dr. Pollack. And hi everyone, my name is Sujata Dutta, and I was diagnosed with a cancer called multiple myeloma in December of 2019. And I’ve been on a clinical trial since September of 2020.
Katherine Banwell:
Thank you, for that information. And we’re going to go into that further in just a few moments. Let’s start with a basic question, Dr. Pollack. What is a clinical trial?
Dr. Seth Pollack:
Yeah. It’s a basic question, but actually, sometimes, it can be harder to answer than you might think.
I think everybody has an idea in their mind about what a clinical trial is, you’re going to test a new approach. But actually, there’s a whole variety of different things that can be a clinical trial, right? A clinical trial a lot of the times is testing a new drug, could be testing something for the very first time, could be testing something in combination with other drugs for the very first time. It could be testing a standard approach but doing it in a new way. It could even be giving less treatments than we usually do. For example, if there’s a very intense, harsh, standard of care treatment we might even have a clinical trial where we try a little bit less and see that patients do just as well. So, all of those things are clinical trials, but really the clinical trial in its heart is a very organized and careful approach to testing a new treatment strategy for patients.
Katherine Banwell:
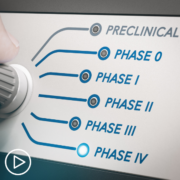
Okay. What are the phases of a clinical trial?
Dr. Seth Pollack:
Yup. So, the Phase I clinical trial is usually when we’re testing something for the first time in however we’re doing it. So, it could be the first time we’re testing a new drug, or the first time we’re testing a drug in combination with other drugs. And the real thing about a Phase I trial is that the main goal of the trial is to look at the safety and tolerability of the regiment. That doesn’t mean that we’re not really trying to figure out if the regiment works, I mean, that’s also one of the most important things. But the most important thing for a Phase I trial is making sure that it’s safe and tolerable. A Phase II trial is where we, sort of, shift and we’re still making sure, and double checking, that the drug is, but now our main focus becomes on the efficacy of the strategy.
So, now we’re trying to really figure out if this is a strategy that seems affective enough to go to a Phase III. And a Phase III is a big multi-center trial. Frequently those will be placebo controlled where a lot of the times there’ll be randomized trial where we really try to absolutely prove, beyond a shadow of a doubt, that, that strategy is affective. And those are most of the types of trials that patients will encounter.
Katherine Banwell:
Okay. Thank you for providing clarity around the phases. Before we move onto safety and benefits of clinical trials, let’s hear from Sujata. Sujata, I understand that you went through a series of treatments for your multiple myeloma, which is a type of blood cancer, including a stem cell transplant.
At what point did you and your doctor consider a clinical trial might be best for you?
Sujata Dutta:
Yes, you’re right. I was diagnosed with multiple myeloma in December, and so the line of treatment or the standard protocol is that you go through what is called an induction therapy. Which is like a few cycles of chemotherapy which get you ready for a transplant. And the transplant, the hope is that it kind of washes away, or cleans off all the cancer cells for you, or at least brings the cancer to a very, very minimal level. And I did go through six rounds of chemo which got me ready for the transplant, and I went through the transplant in June of 2020. However, I’m amongst the very few, small percentage of people that just did not respond with the transplant. So, I was at the same point as where I started. So, it was a little bit disappointing, but my doctors were there to help me understand the situation. It was a hard pill to swallow.
But anyways, there were options. And that’s what I feel very hopeful about with multiple myeloma is that there are so many options available today through treat, or to at least bring the disease under control to a very large extent. And I expressed a desire to be in a trial very earlier on, so my doctor did know that I would lend a year or two listening to what the trials were. And it just so happened that there was a trial that was very apt in my situation, somebody who had gone through a transplant. They have some criteria, and I was able to meet that criteria. And so, for me, it seemed to be the right decision to make. And so, that’s how I agreed to be part of the trial.
Katherine Banwell:
Can you go into some detail about why you thought a clinical trial was a best thing for you?
Sujata Dutta:
Yeah. So, initially before knowing much about the strain that I’m a part of, I just had the desire to be part of a trial because I was always in awe of patients who had been in trials before me.
And because of whom I was benefiting. But whatever regiments, medications, combos, whatever was happening. And so, from that perspective I always wanted to give back in some way. Unfortunately, we are having more people being diagnosed with cancers, with multiple myeloma, and so I was very motivated to do something for the community that I was now part of. And so, I had my transplant at Mayo, and I knew that they had a whole bunch of trials and had access to different types of trials. So, that was my first motivation and it just so happened that, as I said, my experience with transplant didn’t go the desired way. And so, when I heard that there was a possibility that I could be part of a trial, I kind of leaned into actually agreeing to be part of that.
Katherine Banwell:
Yeah. It sounds like that was the next step for you.
Sujata Dutta:
Yup.
Katherine Banwell:
Yeah. Well, I’d like to address a list of common concerns about clinical trials that we’ve heard from various audience members prior to this program.
And this is probably the most common; I will be a guinea pig. Dr. Pollack, how do you respond to that?
Dr. Seth Pollack:
Yeah. I know that is a common concern. I mean, I think the thing that people have to understand about clinical trials is there is just so much oversight that happens for these clinical trials. Every document, every procedure, is scrutinized by multiple committees. There’s a scientific review committee, there’s a review board, IRB, that reviews these. Many of these trials are reviewed by the FDA and they’re reviewed by your doctor and your doctor’s colleagues that are also participating in the trial. So, every detail is discussed at length.
In fact, a lot of the times there’s a lot more structure to being on the clinical trial than just routine clinical care because they’ve thought so thoroughly about when everything needs to be done and what the right timing of is for the various procedures.
Katherine Banwell:
Right. And another concern that people have is; clinical trials are my last resort treatment option. What do you say to that Dr. Pollack?
Dr. Seth Pollack:
Yeah, no. That’s a common misconception. So, we like to have clinical trials for every phase of the patient’s cancer journey because we’re trying to make every single part of the cancer journey better. So, I think a lot of people think that, okay, when they hit their last resort that’s kind of the time to try something new. Even in the very earliest parts of the cancer journey, even in the diagnosis phase sometimes we’ll have clinical trials where we’ve tried different images, modalities, or look at things in a different way in terms of the biopsies.
But then, in terms of the cured-of treatments, when somebody is in the cured-of setting we don’t usually try something very brand new. But a lot of the times we’ll try something that is very affective for patients at the end, and we want to try and make the cured-of strategy even better. So, a lot of the times for those patients we’ll have new therapies that are very safe and established that we’re trying to incorporate earlier into patients’ treatments because we know they work really well, right? And then, even in patients who have incurable cancer a lot of times it’s better to try a clinical trial earlier on just because sometimes the clinical trials have the most exciting new therapies that are bringing people a lot of hope.
And a lot of the times you want to try that when you’re really fit and when you’re in good shape. So, that’s why I think that you really want to think about doing a clinical trial when the opportunity arises.
Katherine Banwell:
Yeah. Beause it could be beneficial to you and it’s certainly going to be beneficial to other people. Is this fact or fiction; it will be expensive? Dr. Pollack?
Dr. Seth Pollack:
That’s fiction because the way the clinical trials work is we go through everything very carefully to figure out what things are standard and what things are unique to the clinical trials. So, if you are getting chemotherapy, you’re going to need blood work, you’re going to need the chemotherapy drugs, you’re going to need some sort of imaging, CT scan, or whatever your doctor would do.
And all those sorts of things are considered standard, so your insurance company is built for those. Then there’s a bunch of things that are considered research. For example, there’s special research bloodwork, maybe there’s an investigational agent that’s being added to standard chemotherapy. Those things are billed to the study, so you don’t actually have to pay anything extra, it’s just like you’re getting the normal treatment as far as you’re concerned. I mean, that’s the way it always is, and I haven’t had any of my patients ever get into real problems in terms of the finances of these things. It always works very straight forward like standard therapy.
Katherine Banwell:
Okay. That’s good to know. The logistics will be a nightmare and I don’t live close to a research hospital. Sujata, did you have that issue?
Sujata Dutta:
Yeah. That’s a very interesting one, and actually I’ll share my experience. I did have this concern about logistics, because I got my transplant at Mayo Rochester, which is a two-hour drive from where I live. And so, when I got to know about it literally me and my husband were like, “Oh, my gosh. What are we going to do?” It’s not just me, my husband is my caregiver, he has to take the day off to drive me to Mayo, wait through my treatment, and drive me back. Then we have boys who were distance learning at the time, and so what do we do with them? Do we drop off a friends or take a favor from a friend? And so on and so forth.
So, the logistics was an issue and we literally said, “Thanks but no thanks” and we walked out of the room. And we came downstairs, and my husband was like, “What the heck?” My team understands everything, and I fortunately work for a very good employer, and they understand everything, people first. And so, he was like, “I can figure this out. Let’s do it if this is what’s going to help you, then let’s just figure this out.” And at that time, it was so good, and I have total respect for Dr. Pollack.
You and everybody in this medical community. My doctor who leads the trial at Mayo, she actually said, “Why don’t you check with your local cancer center? Maybe they are also approved by FDA, and they may be able to administer this treatment to you.” Unfortunately, at that time they weren’t but we were like, “We’re going to go ahead with the trial. It doesn’t matter.” My husband was like, “I’ll take the day off, you don’t worry about it.” And then, four months later my institute did get approved by FDA, and so I was able to transfer from Mayo to my local cancer center, Abramson Cancer Center, which is 20 minutes from home. And so, there are options, I know that it can be an issue and it can be overwhelming at the time which was the case with me. But I was able to overcome that, so maybe there are options available that the patients can consider.
Katherine Banwell:
Yeah. Dr. Pollack, do you have anything to add?
Dr. Seth Pollack:
No. I think the logistics and the location are real concerns with clinical trials.
Clinical trials do sometimes require you to have an extra visit, sometimes they’re a little bit less flexible in terms of when you can get your medication. If you’re getting a standard treatment your doctor may say, “It’s probably okay for you to wait an extra week.” Whereas sometimes on a clinical trial, not always, but sometimes they could be a little bit more strict about when you’re supposed to get certain things. And likewise, with the travel for some people that can be an issue. I mean, the clinical trial is not available everywhere. I mean, Sujata was very lucky that she was able to do the clinical trial she was doing close to home, but that doesn’t always happen. So, I think that’s an important thing to talk to your clinical team about.
Katherine Banwell:
Yeah. Some patients feel that clinical trials aren’t safe, is that the case, Dr. Pollack?
Dr. Seth Pollack:
No. I mean, we go through, as I was saying before, these clinical trials are extensively vetted. So, the safety is, of course, one of the things that we look most carefully about. But as I was saying before, like with any treatment’s cancer treatments have toxicity, that’s a common problem. So, and when you’re dealing with something brand new sometimes there is a little bit more risk. So, when you’re talking about these very early-stage Phase I trials you probably want to talk to your doctor about what sorts of toxicities you can expect and where they are in the Phase I trial. Are you the first ever to receive this new drug? And if you are nobody’s making you go in the clinical trial, so it can only help to get more information. Right? So, you should ask your team about it, you should find out.
Most of the time there’s going to be a lot of patients that have been treated already, I mean, they can’t give you definitive data about how things are going but they can maybe say, “Hey. I’ve already treated a few patients on it, and they seem to be doing great.”
Katherine Banwell:
So, you need to weigh the pros and cons of the trial.
Dr. Seth Pollack:
You do need to weigh the pros and cons. Now, when you’re talking about these Phase IIs and Phase IIIs, I mean, these are drugs now that have really been vetted for their safety and we have a lot of data about it. And even the Phase Is, it’s not like these things are coming out of nowhere, they’ve been scrutinized, we really expect that they’re going to be safe but we’re doing the trial to prove it. So, it’s a good thing to ask about.
Katherine Banwell:
Yeah, yeah.
Sujata Dutta:
Yeah. I would also add that it’s so closely monitored that safety is a top priority, it’s front and center. So, the advantage, I think, with being on a trial is the close monitoring of the patient exactly for this reason.
If something is amiss it’s going to be picked up as quickly as possible and you’re any issues are going to be addressed as soon as. So, I think, safety does get addressed pretty quickly.
Katherine Banwell:
Good, good. Okay. That’s good to know. Another concern is; I’ll get a placebo. Dr. Pollack, what is a placebo first of all? And is that true in a clinical trial setting?
Dr. Seth Pollack:
So, there are clinical trials with placebos, it’s a real thing. And what a placebo is, it’s a pill and it’s made to look just like the real pill, but it doesn’t have any active drug in it. Sometimes people say it’s a sugar pill, but it may or may not be sugar, but it’ll probably be something without a taste. But it’s an inert substance that is not going to affect you at all.
And your doctor won’t know whether you’re getting a placebo or not, so a lot of the times they’ll call these things double-blind because your doctor doesn’t know, your pharmacist doesn’t know. And to unblind you they have to go through special procedures to find out whether you’re on the studied drug or not.
Katherine Banwell:
Would a placebo be given solely? Or would it be given in addition to this new drug that’s being tested?
Dr. Seth Pollack:
Yeah. So, it’s unusual for a placebo to be given solely. Usually there’ll be a clinical trial where you’re getting the standard treatments plus the new drug or standard treatment plus the placebo, so no matter what you’re getting the standard treatments. There are still some trials where, and these are usually for patients with very advanced cancer, who there’s not really any treatment options that are good. Where they will randomize people to just be on the standard drug versus the placebo.
Sometimes what they’ll do is if they want to do a trial that’s the standard drug versus a placebo, they’ll do the imaging very frequently and they’ll have a crossover. So, a crossover means that everybody gets to be on the new drug, but some people will have to go on the placebo first. So, and then they watch you very closely. So, if you get randomized to go on the placebo and your cancer starts to grow, they figure it out very quickly and then they give you the opportunity to go on the new drug.
Katherine Banwell:
I see, okay. I’ll be stuck in the trial forever and I can’t change my mind. Sujata, did that happen to you?
Sujata Dutta:
No. I mean, when I finally agreed and signed the dotted line it was made very clear to me that it was voluntary, I was volunteering to be part of the trial and I could get out of the trial at any point of time. So, in my case I’m in Phase III of a trial, the first commitment was for two years and then the next was five years.
So, again, it sounds daunting to me right now, two years is coming to an end in July of this year. I’m like, “Wow! Two years are over already?” And then five years, I’m not thinking about that, but again, it was at any point I could just say that I’ve had enough, or whatever be the reason, I could get out of the trial. So, no. Yes. There’s an option.
Katherine Banwell:
Can data from trials even be trusted? Dr. Pollack, is that the case?
Dr. Seth Pollack:
Well, of course, I mean, it can be trusted. Because the thing with the clinical trial data is that you really see the data and there’s all kinds of scrutiny making sure that the data is reported accurately. Now, there’s a whole other conversation we could have as to whether we could interpret the data differently. And sometimes that is an issue that comes up, but the data is reported very accurately.
So, and there are statistics that are very well understood, and the bar is actually pretty high to say one arm of the trial was better than the other arm of the trial. So, if patients have better survival on one arm, if we say that, usually it means they did considerably better. Enough better that it wasn’t a random chance that one extra patient did better on the treatment arm. No. There were enough patients that did better that the statisticians can go through it with a fine-toothed comb. And they can be absolutely sure up to exactly how many percent sure they can tell you, 0.05 percent or less chance of error that this was a real difference between the study arm and the standard of care arm.
Sujata Dutta:
I think you mentioned too that one is trust, and one is data. So, Dr. Pollack mentioned a lot about the data, I think the trust is also a very important thing. I like to go with positive intent because I do not have a reason to believe my doctor has some ulterior motive to suggest a clinical trial. And so, I trust them wholeheartedly. The first hurdle is you have to trust the system or what is being proposed to you because, as Dr. Pollack said, it’s gone through a lot of vetting. A recommendation to be part of a trial itself is vetted by your doctor when they make the recommendation. So, have faith, trust, that they are making a good recommendation. And then, of course, the data, I don’t know much about that, but as I said, I trust it. So, I would trust the data too.
Katherine Banwell:
Of course. Of course. Some patients feel like they’re going to lose their privacy. Sujata, did you feel that at all?
Sujata Dutta:
No. Not at all.
I mean, with everything else that is also taken care of, my information, or whatever, is not made available to anybody. And so, obviously there’s a lot of people will get those, and I had a huge pile of paperwork to go through, but I think that’s a good thing. For my peace of mind that I knew that my information was not going to be shared outside of the study, the trial, etc., and things. So, no, I don’t think that’s a problem.
Katherine Banwell:
Beyond these misconceptions is there anything else you hear? Dr. Pollack?
Dr. Seth Pollack:
Well, I hear a lot of people really interested in clinical trials. I mean especially, I treat some patients with rare cancers or with unusual presentations and I think people are very excited to be a part of something that could be new, that could be the next wave. A lot of times the clinical trials have new things with the most exciting science that could be the future of treatment.
So, I think a lot of people are excited about clinical trials. And I also hear some of the reservations that you’re expressing. I think usually when patients ask their questions are very straightforward and easy to address so that people can make their own decisions.
Katherine Banwell:
Dr. Pollack, I’d like to go back to you and ask you the same question about privacy. Do patients need to be worried about that?
Dr. Seth Pollack:
No. I mean, look, in our crazy modern world there’s concerns everywhere, but the clinical trial is very, very careful. Whenever possible we use the medical chart.
And then, we have a very stringently protected database that’s storing people’s information, but it’s deidentified. So, I mean, we have a separate key to figure out who the patients are and then we try to limit the use of the patient’s name or any identifying information about them beyond that. So, and your information is not shared. For example, if there’s a drug company involved in the trial, your information is not shared with the drug company, you have a new identifier that is unique and not traceable back to you that is provided to whoever, if there’s outside groups working on the trial with you. So, your information is very carefully protected, and everyone is very conscious about issues regarding privacy.
Katherine Banwell:
That’s great to know. Sujata, there’s clearly a lot of hesitation and misconceptions out there. What would you say to someone who’s considering a trial but is hesitant?
Sujata Dutta:
I would say speak to your provider, speak to your doctor, and get all these myths kind of busted to say, “it’s going to be expensive” or whatever those questions are. And then, through that process also try and understand what is it that the study is trying to achieve? How is that going to be beneficial to you? So, in my instance, it wasn’t the last line of defense, it was just one of the processes or combos that would help me. And so, that was important for me to understand and then a little bit of education as well. So, I was asking, I have questions on my phone every time I meet my provider, and I did the same thing. So, I think that one of the good practices is keep your note of your questions and have those questions ready. And no question is silly, all questions are important. So, ask as many questions as you can and use that opportunity to educate yourself about it.
And maybe you realize, “No. I don’t think it’s working for me” or “I don’t think this trial is good for me.” But it’s good, important, to have that conversation with your provider, that’s what I would recommend highly.
Katherine Banwell:
Excellent. Thank you, Dr. Pollack, if someone is interested in participating, how can they find out about what trials are even available for them?
Dr. Seth Pollack:
Yeah. I mean, the best thing to do is to start just by asking your doctor if they know about any clinical trials. And a lot of the times the clinical trials are run at the big medical centers that may be closer to you, so you could ask your doctor if there’s any clinical trials at the big medical center even. Or I always think it’s good to get a second opinion, you could go get a second opinion at the big medical center that’s close to you and ask them what clinical trials are at your center.
And sometimes they’ll be conscious about some of the clinical trials that may be even run around the country. And you can ask about that as well.
Katherine Banwell:
Would specialists have more information about clinical trials than say a general practitioner?
Dr. Seth Pollack:
So, I specialize in rare cancers, so a lot of the times the general practitioners they’ve got my cell phone number, and they text me, and they say, “Hey, do you have a clinical trial going on right now?” And that happens all the time, but yeah, the specialists will usually because frankly there’s so much to know. And the general practitioners really have a lot to keep track of with all the different types of diseases that are out there. Whereas at the big centers, the specialists, part of their job is really to keep their tabs on what’s going on with the clinical trials.
So, they’re good people to ask, either your local doctor could reach out to them, or you could go get a second opinion and ask.
Sujata Dutta:
There’s also a lot of information, Katherine, on sites such as LLS, or PEN, or American Cancer Society that they also publish a lot of information. Of course, I would recommend once you have that information then vet it by your specialist, or whatever. But if you’re interested in knowing more about clinical trials in general and some that would work for you, then those are also some places to get information from.
Katherine Banwell:
That’s great information. Thank you, I was going to ask you about that Sujata. Well, before we end the program, Dr. Pollack, I’d like to get your final thoughts. What message do you want to leave the audience with related to clinical trial participation?
Dr. Seth Pollack:
Yeah. I think clinical trials it can be a very rewarding thing for a lot of patients to do, I think patients really like learning about the new treatments. And I think a lot of patients really like being a part of pushing the therapies forward in addition to feeling like sometimes they’re getting a little bit of an extra layer of scrutiny, because there’s a whole extra team of research coordinators that are going through everything.
And getting access to something that isn’t available yet to the general population. So, I think there’s a whole host of advantages of going on clinical trials, but you need to figure out whether or not a clinical trial is right for you.
Katherine Banwell:
Yeah. Sujata, what would you like to add?
Sujata Dutta:
Absolutely, I second everything that Dr. Pollack is saying. And in my personal experience I wouldn’t say everything is hunky-dory, everything is fine. I’m going through treatment, I have chemo every four weeks, I started with chemo every week. That’s when the logistics pace was really difficult because going to Mayo every week was not easy. But anyways, as the trial progress itself every four weeks, but as I said the benefits are huge because I have labs every four weeks. I meet my provider every four weeks.
So, we go through the labs and anything amiss, I’ve had some changes to my dosage because I’ve had some changes in the labs. And so, there’s a lot of scrutiny which I like, but the flip side, for maybe some maybe like, “I have to have chemo every four weeks. Do I want to do that or not?” Or whatever. In my case, I knew it, and I signed up for it, and I’m committed to doing that for two years. And so, I’m fine with that. So, I would say all in all, I’d see more benefits of being in a clinical trial. One, you’re motivated to give back to the community. Two, you are being monitored and so your health is important to your provider just as it is to you. And so, I highly recommend being part of a trial if it works for you and if you’re eligible for one.
Katherine Banwell:
Yeah. Sujata Dutta, and Dr. Pollack, thank you both for taking the time to join us today.
Sujata Dutta:
Thank you.
Dr. Seth Pollack:
Thank you.
Katherine Banwell:
And thank you to all of our partners. To access tools to help you become a proactive patient, visit powerfulpatients.org. I’m Katherine Banwell, thanks for joining us.