How Can Care Partners Combat Burnout?
How Can Care Partners Combat Burnout? from Patient Empowerment Network on Vimeo.
Care partners Diahanna, Sherea, and Patricia discuss how they have learned to overcome burnout. Often times when caring for a loved one, we don’t even realize the burnout until after the fact. As care partners, you have to know when to step away and take time for yourself, so you can effectively care for and support your loved one.
Transcript
Diahanna:
Hello, we’re going to talk about care partner burnout. So the question I would like to pose is, how would you describe caregiver burnout? And how do you feel it coming on? And how can you counteract it? And Patricia or Sherea, either one of you can answer those questions, it would be great to hear from you.
Patricia:
Let me just start with, I have been a caregiver. Although I am right now experiencing multiple myeloma, my father had multiple myeloma and passed in 1990 and I was his caregiver. At that time, a very young person. So, he actually had to have part of his breast bone removed and they left the wound open, and it had to be pack everyday, twice a day with gauze and an iodine thing. And so, my mom could just not do it and my though was, well she can’t, I have to. So every morning before work, I would go and take care of him in that way. Every evening when I came home from work, before he went to bed, I would go over and do the same thing. And that went on for several months. Because I was young and because I really did not have any understanding of what as going on with my father. I mean multiple myeloma, what is that? Not like today. Today there is information. You know you go online, you can find the information. It worked out anyway that I was able to take care of him. I didn’t know that I even had a burnout cause I just continued to do what I was doing. I worked everyday, I had three kids, you jut do what you have to do and I think that’s what most caregivers get to a point of saying to themselves, “I’ll do what I have to do”. And whether they know they have burnout or not, they just do it.
Diahanna:
You know, I think that is very interesting, Patricia, because I think women have a tendency to do that more so than man because we are already maternal. We’re caregivers.
Patricia:
Yeah.
Diahanna:
And we, if someone else drops the ball, and you know we are used to being on call 24 hours a day, 7 days a week, vacation or not. And so, we do always step in and tack up the slack and put ourselves on the back burner. A lot of the time we don’t realize we’re burnout until after the fact.
Patricia:
Way after.
Diahanna:
And we have no more energy. We have nothing else to give ourselves. So Sherea, how would you describe it? How would you look at this?
Sherea:
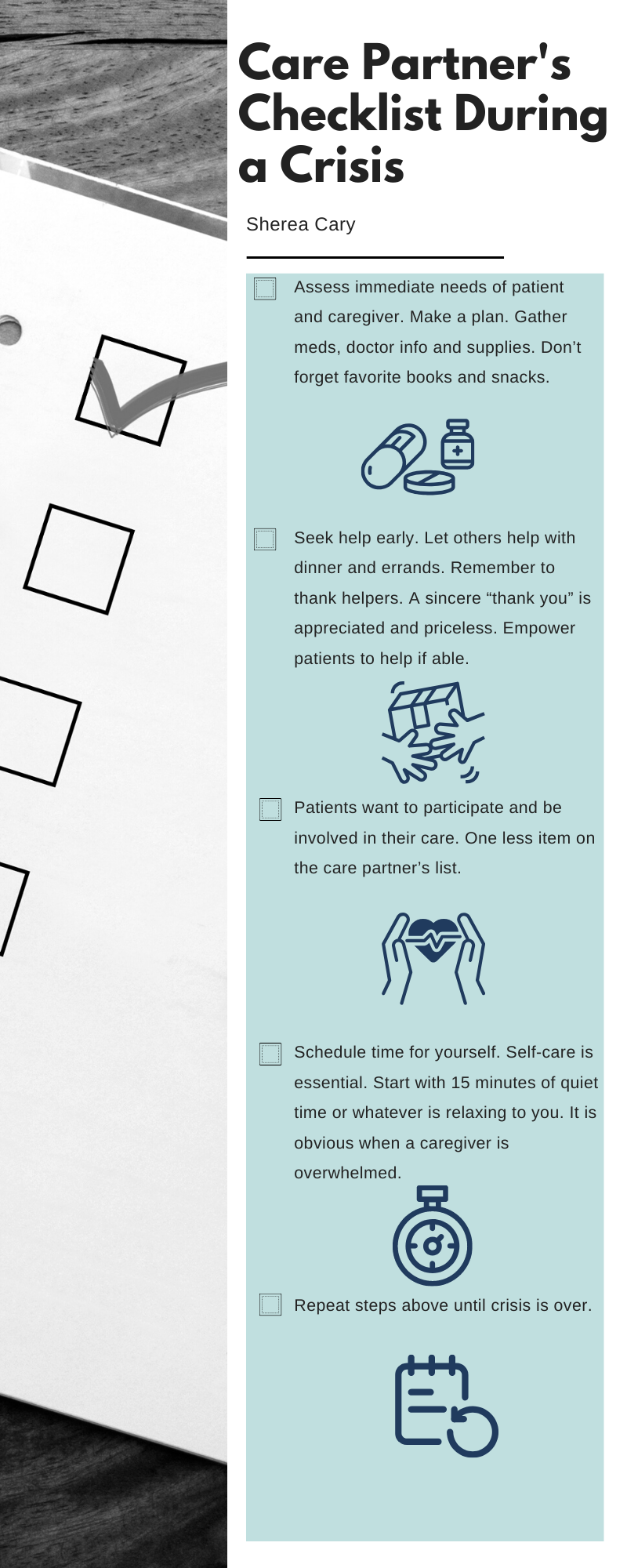
I would describe…I was a caregiver for my father, now I’m doing some caregiving for my mother who is having some memory issues. And what I can tell you about the feeling is, the feeling of being overwhelmed, the feeling of pressure, and what I notice with is that I have a short fuse. When I’m feeling burnout, things that normally would just not be a problem become an issue. And so, what I try to do is recognize that I’m having a moment and that I’m going to need to step away for a little bit and get recentered. And I do understand that yes, as women, we just do what we have to do, but there does come a point where you have just had it. You’re at the end of the rope. And I’m starting to recognize that more. So it is a feeling of pressure and just being overwhelmed. And the moment I start feeling it, it used to be I kind of just keep pushing, but now the moment I start feeling it, ok let’s work on that now so it doesn’t become an issue later.
Diahanna:
Mhmm. I can appreciate that. When I was taking care of my husband, I probably put myself in a position where I was taking care of him at times when he didn’t need to be taken care of. It was that thing as I felt I could do better or more for him that he probably didn’t know about or I thought he didn’t know about. And I was mistaken on that. It got to the point where I wasn’t sleeping, there was a lot of anxiety, a lot of stress, I wasn’t eating well, and I was getting colds all the time, which I normally wouldn’t get. So my immune system, everything, was messed up as a result of what I was doing. And I remember coming home from work thinking I can’t do this anymore. If I’m going to be a partner to him, I have to step aside. And I called because I was going to every appointment, I was looking at everything, I was doing all the research because he thought he didn’t have to research as long as he felt good, everything was ok. He said, “I’m going to let you be the person that worries because I know you worry enough for the both of us.” And I did. I worried enough for everybody in the household and it was taking me down a path of being mentally, physically, emotionally stressed. And I had to step away and say, “Honey, I don’t need to go to all your appointments. I don’t need to continue to do this.” And that’s how I realized that I was doing way too much and that I was going to be doing a disservice to him – to everybody in my household.