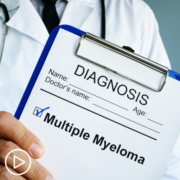
How MPN Researchers Collaborate to Advance Patient Care
How MPN Researchers Collaborate to Advance Patient Care from Patient Empowerment Network on Vimeo.
MPN specialist and researcher Dr. Gabriela Hobbs discusses how collaboration and data sharing among researchers around the world impact MPN treatment advances.
Dr. Gabriela Hobbs is a hematology-oncology physician specializing in the care of patients with myeloproliferative neoplasms (MPN), chronic myeloid leukemia, and leukemia. Dr. Hobbs serves as clinical director of the adult leukemia service at Massachusetts General Hospital. Learn more about Dr. Hobbs.
See More From MPN Clinical Trials 201
Related Programs:

|

The Risks and Benefits of Participating in an MPN Clinical Trial |

|
Transcript:
Katherine:
I’d like to start by discussing your role as an MPN researcher. You’re on the front lines for advancements in the field. What led you to there, and why is it so important to you?
Dr. Hobbs:
Many things in my life led me to becoming an MPN clinician. First, I wanted to be a clinical investigator since I was very little, and I read a Louis Pasteur book about – you know. And I was fascinated by the fact that you could be both a scientist and a clinician. And after that, I had phenomenal teachers and mentors. And I was really always drawn to patients with hematologic malignancies. I thought that that interaction was very intense and intimate.
And I was honored to be a part of that interaction. And then from a research perspective and from a scientific perspective, I very clearly remember seeing when the first targeted therapy, Imatinib, was approved when I was an undergrad. And I just thought that was the most fascinating thing. And so, I’ve basically continued to feel that way as I’ve gone through my training, and I’m thrilled to be able to have actually become an MPN clinician so many years later.
Katherine:
With the American Society of Hematology or ASH meeting taking place this month, it demonstrates how researchers work together around the world to advance care.
Can you share with the audience how this collaboration works?
Dr. Hobbs:
Yeah. So, the American Society of Hematology meeting – or the ASH meeting – is really one of my favorite events of the year.
And it really highlights what you said. It is such a positive environment, and it’s so exciting to use that opportunity to talk to my collaborators from across the globe. And I really think that that’s where the scientific community shines because really all of us are actually trying to figure out how to work together and overcome sometimes a lot of obstacles – bureaucratic obstacles, regulatory obstacles – to make sure that we can share data, do it the right way. But really we always have one thing in mind.
And that is to be able to advance the care that we give our patients. And so, that collaboration and really that collaborative environment is always very positive. And I always come back home very energized from that. And then just seeing all my colleagues presenting all the wonderful things that they are working on and getting updates on their research is just an exciting environment.
Katherine:
In your view, why is it essential to present and share data at these larger conferences like ASH?
Dr. Hobbs:
So, for many different reasons. I mean, there are many different ways of presenting data that can be done through just publishing a paper. But the nice thing about conferences – and especially large conferences – is that you really get an opportunity to present work in progress. And some of these research projects may not end up turning into bigger projects or they may not become bigger trials. But all of them have at least an opportunity to learn something from them, whether or not they worked or they didn’t work.
Oftentimes when things are published in journals, especially the high-impact journals, we are seeing trials that had positive results. But sometimes we don’t see those smaller trials that never went anywhere. And so, having a forum when we can discuss work that’s ongoing, discuss about projects that are maybe having issues, all those things actually really help us to change our research questions or develop new research questions based on what’s working and also really what’s not working. And so, having this large forum to present all of that data, I think, is really, really important to helping us design future clinical trials and projects.