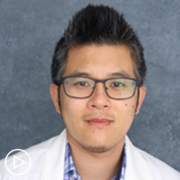
Dr. Beth Faiman is an Adult Nurse Practitioner in the department of Hematologic Oncology and Blood Disorders at the Cleveland Clinic. Learn more about
Dr. Faiman.
See More From Thrive CAR T-Cell Therapy
Download Resource Guide
Related Resources:
Transcript:
Katherine Banwell:
Welcome. I’m your host, Katherine Banwell. As patients navigate their myeloma care, it’s essential for them to feel formed when engaging with their care team. That’s why the Patient Empowerment Network developed the Thrive series, to share support and educational resources so that patients can feel confident at every stage of their care. In today’s program, we’re going to hear from a renowned myeloma expert as we discuss CAR-T therapy. Before we meet today’s guest, please remember that this program is not a substitute for seeking medical advice. Please refer to your healthcare team about what might be best for you.
Well, joining us today is Dr. Beth Faiman. Dr. Faiman, welcome. Would you please introduce yourself?
Dr. Beth Faiman:
Thank you so much, Katherine, and it’s such an honor and a pleasure to be here today. My name is Beth Faiman. I am a nurse practitioner and a PhD researcher at the Cleveland Clinic in Cleveland, Ohio, where I have worked since 1994, in the field of myeloma mostly. Thank you.
Katherine Banwell:
Excellent. Thank you so much for joining us today. As I mentioned, today’s program is part of our Thrive series. So, from your perspective, what does it mean to thrive with myeloma?
Dr. Beth Faiman:
So, to thrive with myeloma is something that when I started managing patients in the 1990s individuals didn’t live very long, maybe two to three years, because we did not have good therapies. Now, we talk about living well with myeloma, thriving with myeloma. It just makes me so happy. I think for plants. I think of flowers that can grow in the right environment. I had a plant in my office recently that somebody had gifted me, and it sat there and tried to soak up the little bit of sunlight that it could muster and just wasn’t doing well.
So, I brought it home and I put it in a big window. That plant is beautiful now and I just love looking at it and thinking about it. And it reminds me of how if you’re in your right environment with multiple myeloma you surround yourself with friends, families, coworkers, church friends, or places of worship, then you can really thrive in that environment or you can grow. And even though you have a cancer diagnosis, that is not – and I hate to use the D-word – a death sentence anymore. You can live many years and live well with myeloma in the right environment like my little plant.
Katherine Banwell:
That’s a great idea to think about. Thank you. Well, we’ve covered this in recent webinars but it’s worth sharing again. Can you give us an overview of the process and timeline for someone choosing CAR T-cell therapy for myeloma treatment?
Dr. Beth Faiman:
Yes. So, CAR T-cell therapy, when we first started discussing this in the mid-2000s, I thought this was science fiction.
Taking somebody’s own cells, engineering them to be fighters against the cancer cells. I thought it was science fiction. But now, we have two FDA approved therapies for multiple myeloma. It’s Ide-cel, which was approved in 2021 and Cilta-cel, approved in 2022.
Now, the process is lengthy and I know you’ve covered this before but from my perspective, I think if you want to take something home form this webinar, plan early. So, you need to have three prior lines of therapy as a myeloma patient to qualify for this treatment. But you can start planning for it ahead of time.
So, it’s not available in every center. So, you want to start researching what the closest center would be for you to have this therapy. Many different patient support networks will have these centers on their websites. So anyhow, you find out.
“Okay. I want to learn more about a CAR T-cell therapy.” Then you have to meet with a specialist. So, you get that education, have that referral, and meet with a specialist at a center that does CAR T-cell therapy. And that might be where you got your initial transplant if you’ve then returned to the community. After that, then we find a slot for you when it’s ready. So, there is that process of financial, physical, social things that are checked in the background. You meet with a social worker, nurses, etc.
Once you’ve confirmed that you’re going to go through this process – now, it might be three, six, nine months in the future, if you’re a planner – but if you want to just gain information, it’s that harvesting and storing of the cells. That’s where I try to tell people age is not a number. You can be at any age and you qualify for this therapy. We’ve had people well into their late 70s to early 80s who have gotten these therapies.
Long story short, it’s a process.
You get your cells harvested and then while they’re being manufactured into fighters, they take the T cells from your blood through an apheresis machine and freeze them, send them off, make them into fighters, and then reinfuse them in your bloodstream. It’s a long process. It can take anywhere from two to three months from when you decide it’s right for you.
Katherine Banwell:
Well, thank you for explaining that. That’s really important. It puts into perspective. It’s a big undertaking. But also, quite manageable, I think, right, with the right team and support. Who are the members?
Dr. Beth Faiman:
Absolutely. The family members, friends, and, of course – I like to use the words the multidisciplinary team. That’s your physicians, your social workers, nurses, nurse practitioners like me, pharmacists, and then all your other specialists.
So really, mounting that team from diagnosis and throughout your whole journey as a myeloma patient can really enrichen your life and help you thrive in that environment.
Katherine Banwell:
Yeah. It sounds like there’s a lot of support for someone going through this process and that the care partner also plays a critical role on the care team, right?
Dr. Beth Faiman:
Oh, absolutely. So, I am a big advocate for care partner though not everybody has a caregiver. So, it can be a formal caregiver, somebody’s spouse, daughter, son, significant other. Or it can be an informal caregiver. So, I’ve had patients that – because you need to have a care partner to qualify for CAR T-cell therapy, because patients need to be monitored for about 30 days afterwards. So, that might be pulling in friends from your place of worship, people from the community, and then also people from the cancer center.
Some of the larger centers that do the CART-cell therapy have a network setup where you get this list of people that have volunteered to drive you to appointments or maybe arrange for Uber help to drive you back and forth. I am not plugging Uber or Lyft, but a rideshare company. And so, finding out those resources can help anyone – just about anyone – access these CAR T-cell therapies, because you can have a long-term remission. Think about somebody who’s been through treatment A, B, C, or D and then now, “Gosh, maybe my life is going to be shortened.”
Not necessarily. If this is the right recipe to control their myeloma then they can get 11, 24 months off of everything – just antibiotics – and be monitored. And so, it puts them at a position where if you can get the care partner, get a care team, to support you then you can have access to a potentially life extending with good quality of life therapy.
Katherine Banwell:
Yeah. I’m sure many of our viewers today are wondering who the therapy is right for and when is it most appropriate in the course of myeloma? Could you address that?
Dr. Beth Faiman:
Yeah, absolutely. So, currently, you have to have had three prior lines of therapy with drugs such as a CD38, which is – daratumumab (Darzalex) is a name of a medication.
You have to have a drug such as lenalidomide (Revlimid) as well as a drug like bortezomib (Velcade). And you have to have had three lines of therapy. So, that’s how you can access the therapy. But if you’re willing to participate in a well-designed clinical trial there are studies with CAR T-cell therapy earlier on.
So, one of the things that we’re advocating in the myeloma world is clinical trials. We haven’t gotten to where we are in 2024 with the advances in sciences, the advances in living longer and living well with myeloma, without the brave people before us that have participated in clinical trials.
So, people who it’s right for would be if they qualify for a clinical trial before their third or fourth line of therapy or if they’ve had three or four prior lines of therapy. And there are other points to that which I’m sure we’ll talk about later on.
Katherine Banwell:
In your opinion, what are three key considerations that myeloma patients and care partners should think about related to the CAR T-cell therapy approach?
Dr. Beth Faiman:
Oh, gosh. Well, I would like to say that always when you’re selecting a therapy, think of the physical, the financial, and the social implications of that therapy. So, physically is the medication too strong for you? Are you too weak to take it? Or is it just right for you? So, finding the right medication for the right patient at the right dose at the right time. So, the physical component. The financial component is also very important. So, maybe your insurance now won’t cover it but then there’s open enrollment in Medicare towards the end of the year or you can find financial support reimbursement through many of our generous organizations that will provide grants for certain medications.
And then, the social. Do you have a care partner, as we discussed? The importance of being monitored for 30 days. If you don’t have a formal care partner, is there some system that we can help support you through so that you can have the different supports throughout. It’s not only that beginning part where you’re gaining the information – and I think of it like a timeline. The beginning part, you’re thinking about gathering information to the – in that process of getting yourselves back because of the side effects, which I think have been talked about in a prior webinar.
And then, the post-monitoring where you go back to your community, taking antibiotics, antiviral medications, etc., to keep you living well longer. So, it’s a process.
Katherine Banwell:
Well, it’s great advice, Dr. Faiman, thank you. I’d also like to add that if you’re considering CAR T-cell therapy, the Patient Empowerment Network has a wealth of information on this topic, including resource guides and interviews with experts like Dr. Faiman.
And you can find those at powerfulpatients.org/myeloma. So, Dr. Faiman, when a patient is talking with their care team about CAR T-cell therapy, what questions should they be asking to help determine if CAR-T is even right for them?
Dr. Beth Faiman:
Katherine, that’s an excellent question. So, let’s just say that somebody from Patient Empowerment Network heard about CAR T-cell therapy for myeloma and then sought out a local institution that might be conducting that procedure. So then, they come for that visit and what you mentioned was just spot on, getting a list of questions together. What we do at my institution, as well as many throughout the country, is a process called shared decision-making.
You might’ve talked about this on prior webinars, but shared decision-making occurs when that healthcare team, such as the physician, nurse practitioner, pharmacist, whoever, shares information with the patient and their care partner.
You mutually share information to arrive at a decision. So, many studies have been done on shared decision-making. It’s done in many different areas. And so, through that sharing of information, you might think of different questions.
Some of the things that I try to proactively offer – we all have our list of things that we educate our patients on, but some of the things I proactively will recommend to patients and their care partners when you’re seeking an opinion at these centers is, “How long will I be sick? What are the biggest side effects of the medication I have to worry about?” Asking your care team – I know it sounds silly, but are they aware of all your prior health concerns, especially if you’re coming for an evaluation.
Maybe you have peripheral neuropathy where you have numbness and tingling in your fingers or toes or a history of kidney disease. Your kidneys look fine now but maybe a few years ago at the myeloma diagnosis the kidneys had a temporary failing and now they’re better so they’d want to protect you with future medications. How long will you have to take medications after the CAR-T procedure? There’s antiviral medicines, antibacterial medications, and medications called IVIG, which strengthens your immune system.
And then, finally, asking about the infection protection afterwards. Do you have to get vaccinated again against pneumococcal, shingles, and all of those other things that we do. The cellular therapy guidelines suggest timepoint for one, three, five, etc., months after CAR T-cell procedure to get revaccinated. So, who’s going to do that for you?
How are you going to know what to get? So, make sure that they give you a timeline, calendars, and set expectations for what you need to do as a patient and then you’ll help them set expectations for what they need to do to provide you the accurate education.
Katherine Banwell:
Well, talking about what to expect after CAR T-cell therapy, would you tell us what some of the potential side effects are?
Dr. Beth Faiman:
Oh, absolutely. So, CAR T-cell therapy – again, it harnesses your immune system using your T cells. Your T cells are so important in your immune system to be programmed as fighters. And as people age, or as long as – after they’ve had myeloma or other kinds of cancers, those T cells just don’t work as well. So, what we want to do is engineer them and program them with what we call a viral vector to be fighters. So, those T cells, as I mentioned, are harvested, stored, and then manufactured to go.
And I tell people it’s like that Pac-Man video game. It goes around in your bloodstream just kind of eating away at the myeloma cells. So, you don’t take any medications. You don’t go in for IVs every week or twice weekly, or taking pills at home to treat the myeloma. It’s what we consider a one-and-done thing. So, if it works for you, it can keep you in remission for quite some time. But if it doesn’t work then there still are other therapies down the road.
So, the CAR T-cell therapy is something that is an option but there are other therapies out there in many cases. There’s something called a bispecific antibody. There are three currently approved for multiple myeloma now. So, maybe a CAR T-cell therapy doesn’t seem right for you because you’re not in a good remission or the cancer’s too active right now so you don’t have the time to wait for manufacturing of the cells and putting them back in your bloodstream.
Those bispecifics will fill that gap. So, when you’re discussing the options, aside from clinical trials and other drugs, the bispecific antibody is very similar. One of the things that I wanted to highlight is that nowadays we’re into these things called sequencing. So, we’re trying to figure out what order to give these super effective drugs. Should we give the bispecific antibodies first or should we give the CAR T-cell therapy first? And in most centers, if you have time to wait and you’re planning, the CAR T-cell therapy is right for most people and then the bispecifics would come later.
Katherine Banwell:
All right. So, after CAR T-cell therapy is completed, what potential side effects might people experience, and what should they look for?
Dr. Beth Faiman:
Absolutely. I think of things in short-term and long-term side effects. So, the short term, you’re going to be admitted to the hospital and you have a risk for – when we get those T cells back – that cytokine release syndrome, or it’s abbreviated CRS – where you’re body’s immune system’s fighting.
I tell folks it’s kind of like if you got a vaccine for a flu vaccine or pneumonia and you had a reaction it’s just way worse. So, you can get a high fever – the big first sign of this CRS. Usually, the providers will jump in with giving you a medication called tocilizumab (Actemra) or a similar drug that blocks IL-6, which is a chemical that is triggered when we get the CRS. And then, it stops those symptoms. And so, most of us know how to do that and will approve your insurance to get access to that tocilizumab or similar drug when we approve your CAR T-cell therapy.
So, that CRS can get you really, really sick. You can get low oxygen levels in your blood. You can get a high fever and you can drop your blood pressure. But most CAR T-cells centers, the nurses and the staff are very well-trained to monitor this every eight hours, in most cases.
Another rare side effect we worry about is ICANS and it’s a neurotoxicity kind of thing.
It can be with CRS or without CRS. But they’ll ask you to do things like write your name on a piece of paper every eight hours or tell me – draw a clock or count backwards from 100. And so, if you have any deviation, even minor, from what you reported back beforehand then we worry about neurotoxicity. Now, that’s short term but that’s the reason why you can’t drive a car for 30 days is because it could be delayed.
The CRS can start with the one thing, the ide-cel usually occurs within one day so most people are admitted to the hospital for that CAR T-cell therapy. The Cilta-cel, it onsets to about seven days. So, some people get the cilta-cel outpatient and then are monitored daily, whether in person or through virtual telehealth monitoring.
But at any rate, those are the short-term. Long-term, we worry about low blood counts maybe for the first month afterwards. And then, those will come back to normal. And then, we worry about infection. So, I mentioned the antibacterial, antiviral, which is usually a medicine called acyclovir (Zovirax), which most myeloma patients will have been on anyhow. And then, that IVIG to protect against viruses and bacteria when your immune system is so low.
But fortunately, if we control the CRS, it usually comes with the CRS, although it can be independent. We try not to give steroids, because we don’t want it to interrupt the CAR T-cell process. But many institutions will give that tocilizumab for ICANS. And if that doesn’t get better then they’ll give you a steroid, such as dexamethasone (Decadron).
And so, that will usually reverse itself pretty quickly. Longer term, after 30 days, you can get with the Carvykti, particularly something called Parkinsonian things where you can get a little bit shaky or something like that. Again, it’s very rare and I have had hundreds of people who have undergone the CAR T-cell procedure at my institution. And knock on wood, fortunately, I’ve not seen first-hand that side effect. And I think it’s because we’re so good now at treating the – preventing the ICANS and CRS as best as we can while they’re inpatient and doing real close following.
One other thing I want to note is if somebody who’s watching this does go in the hospital for any reason, get up and walk around and stay strong, as well as you can, during the procedure. You might be bored if you’re in the hospital anyhow, but try to stay as strong as you can in the hospital. It’ll help your post recovery for sure.
Katherine Banwell:
Well, what about more mild side effects like fatigue and changes in appetite?
Dr. Beth Faiman:
Absolutely. So, the fatigue and the changes in appetite are generally mild for most but I see it, in my experience, if your myeloma’s acting up really quickly, if you’re having a rapid disease progression, the medications that we give you to control the myeloma during this bridging therapy phase might cause some of that as well, not necessarily the CAR T-cell process. But think about it. We’re using your own cells engineered to be fighters.
And so, that first month or two is probably when you’re going to be the most tired as your body is being programmed to fight against the myeloma cells. That fatigue tends to get better. And as I mentioned just a moment earlier, the importance of just walking around in the halls, getting out of bed when you’re in the hospital, that can really help your post recovery. It doesn’t seem like much, but there have been many studies about how muscle mass declines, energy declines when you’re hospitalized.
And we want you to be as strong as you can and thrive as much as you can for when you’re out you can then do the things you want to do at a quicker pace.
Katherine Banwell:
Right. That’s great advice. Beyond monitoring of any issues, what can someone expect related to returning to life as they knew it before the diagnosis? Is there a timeline for resuming lifestyle and activity?
Dr. Beth Faiman:
Yeah. So, I should say I because it’s from my perspective. I am a real strong advocate. I tell people to do what you feel like you can physically do. We know that myeloma can affect the bones and put your bones at risk for breaking and so we give you medicines to protect it. So, I do put some restrictions however on physical activity in terms of, “I don’t want you to bench press 40 pounds or 20 pounds,” in most cases. And depending on what the bones look like on x-ray, I’ll even restrict it to about five to 10 pounds.
If you think about it, that’s a bag of potatoes. So, you don’t want to put too many restrictions on for everybody. But talk to your healthcare provider about what your specific restrictions are with physical activity. Because I don’t really put any restrictions on but I encourage things like riding a bike, especially a stationary bike in your own home, so that if you fall off – hopefully, you won’t fall off a stationary bike. But if you injure yourself, then you’re able to be in a place that somebody can help you.
But riding a bike. Also, exercising in water. Water therapy is a great weight bearing exercise and there are times of day where you can go when the YMCAs or YWCAs aren’t as busy – or community centers. So, you’re less at risk for bacterial or other illnesses. But during that first month, I try to limit their exposure to people because you’re at risk for the different viruses that are all over the place, the bacterial infections.
So, that first month is the critical period where I try to say, “Okay, try to lay low. Let’s get you through this period. Your immune system will start getting stronger on its own after this period.” And then, that month two you start feeling like doing more. You go to the grocery store. You maybe go to eat out at a restaurant but pick a time of day that’s less busy. So, go for an early dinner. There’s no shame in eating at 5:00 p.m. if you want to go out. And then, get a table in the corner with your own wipes. And so, that’s where your immune system is getting stronger.
And then, by month three, I think most people will feel much, much better and much, much stronger. And if you can keep moving throughout this whole time, then you’ll be stronger on the way out.
Katherine Banwell:
Dr. Faiman, from what you’ve described, undergoing CAR T-cell therapy can be a very intense process. Why would someone consider this option over another myeloma treatment option?
Dr. Beth Faiman:
Yeah. So, the CAR T-cell therapies have really transformed myeloma, in my opinion.
When we first started using CAR T-cell therapies, there was a long wait list because people who had had three, five, seven, 10, 12 prior therapies, they had very few other options. So, we had ethically assigned scores to people as to who – we’d get one or two slots a month and then we’d have 80-some people on this list. And we’re thinking, “How do we allocate who’s going to get this therapy?” And it’s because you can have a nice, long remission off of all therapy.
It’s a great, great option for most people. Again, I would hope that we can get this moved further into the disease trajectory. There are actually two studies. One was a KarMMa study. It was published in the New England Journal of Medicine in 2023, early part of 2023.
And it showed that when people get this therapy earlier, the Ide-cel first, you can have a longer remission. So, we’re talking about three, four, five or more prior lines of therapy you can get about 11 months with the Ide-cel.
You could even get a longer remission off of all therapy if you move it earlier. Same with Cilta-cel. We had studies and different cohorts and you can be in a long remission. So, think of somebody who’s – myeloma’s incurable. It’s very treatable but it’s incurable for most. And so, you go from the expectation of staying on treatment until disease progression, much like other chronic conditions like diabetes. We don’t stop medicine for diabetes or high blood pressure.
And it’s the same with myeloma and many of the cancers that we treat these days. And so, a CAR T-cell therapy will give patients the option of having that disease free interval where you can go and travel the world. I have patients that have bought RVs after their CAR T-cell therapy and now they’re going around the world – well, not the world. But around the United States.
Katherine Banwell:
The country.
Dr. Beth Faiman:
The country. And just really enjoying life and taking that time off and being realistic, knowing that we have to do bloodwork every month to make sure the myeloma’s still in remission because it can come back. But at least it’s sleeping for right now. So, you can go out and enjoy your life and take those trips and enjoy the little things and the big things.
Katherine Banwell:
Yeah. Well, thank you for that advice. I’d like to get to a few audience questions that were sent in prior to the program. Alice asks, can you share more information about T-cell collection? A recent webinar mentioned that myeloma must be in good control. Can you share specifics about the bridging therapy prior to infusion?
Dr. Beth Faiman:
Yes. So, again, the process is the lengthy process as we mentioned before. But for the actual T-cell collection, we will have approved you to get the therapy. Financially, we’ve cleared you. Socially, you’ve gotten your support systems and now we’re getting those cells out.
We use a process called apheresis where a temporary catheter is placed under the skin, and it separates your white blood cells and then returns the red bloods and plasma back into the blood. And it sorts out those T cells. The process itself, you’re on the machine for anywhere for two or three hours. Hopefully, it’ll just be one day’s time. And then, they’ll manufacture those cells.
So, during that period where we’ve put your cells and sent them away to wherever’s going to be doing the manufacturing, you’re going to need to get a treatment that’s going to keep you in remission from the myeloma. And it’s not going to prevent you from getting those cells safely back. So, we don’t want anything that’s too toxic for most people. So, what we’re doing now is we have that information that early on is better for myeloma to get these treatments. And so, the hope that bridging therapy won’t be as common of a thing anymore.
Because now we’re selecting people that are – the myeloma’s just starting to act up. Let’s get those cells out, send them off, so we don’t have to do bridging therapy. We can just keep you – add a medication or take away another medication to keep you in remission. So, that’s the goal of bridging therapy. What’s that bridge to get your cells back in for some people? It might be a chemotherapy type of a thing. But for other people it’s just trying to get you that CAR T-cell collection and manufacturing so we don’t really have to change everything all up.
And we’ve been very fortunate now that the wait lists have cleared in most institutions. CAR-T cell is available at more centers across the country and so we don’t have that backlog. And so, fortunately, bridging therapy will hopefully be a little bit less of a thing.
Katherine Banwell:
We have another question. This one from Rita. What kind of monitoring takes places in the months following CAR T-cell therapy and what kinds of medicines are required afterward?
Dr. Beth Faiman:
Oh, excellent. So, the monitoring is usually on the short-term, within the first 30 to 60 days afterwards, oftentimes depending on what your blood counts are showing. You might have to get blood counts tested more frequently. So, that complete blood count shows you the white cells, the red cells. The white cells fight infection. Red cells carry oxygen. Platelets clot the blood. That’s a marker of how well your bone marrow is functioning. It also can be – those innocent bystanders can go low temporarily after this procedure.
So, definitely those CBCs need to be tested, for some people weekly and for some people every other week. And your healthcare team will tell you how often. After that first two to three months and your blood counts are all in good shape, then we can just go oftentimes to a monthly monitoring of the myeloma labs. So, that’s the CBC and the chemistry panel but also the paraproteins in the blood and the urine get monitored.
There’s also another test called a CD4 count that’s something that you wouldn’t have had beforehand. The CD4 count is an immune count that we want to be over 200. Oftentimes, you’ll be on an antibiotic called Bactrim or an inhaled called pentamidine to lessen the chance of a certain kind of infection called PJP, or pneumocystis. So, those are those atypical infections that we’re now seeing with CAR-T cell and other therapies.
And as I mentioned, acyclovir to protect against shingles is a medication but you’re not going to be on any anti-myeloma medications other than maybe a bone strengthener if you get that intermittently. Fortunately, after CAR-T cell, you don’t have any anti myeloma therapy as long as you’re in remission.
Katherine Banwell:
We also received this question from a viewer named Rob. If you receive CAR-T therapy, how long does it last and have you seen remission for a long time?
Dr. Beth Faiman:
So, I’d like to tell Rob that I’ve seen a little bit of a remission and I’ve seen long-time remissions. Unfortunately, it goes back to the biology of the disease. People that have a more aggressive type of myeloma tend to not have as long of a remission but that’s not always the case. So, if you have what’s called a standard type of myeloma, which fortunately about 80 percent of the people have a standard or good type of myeloma, you can get an 11- to 24-month remission if you’ve had many prior therapies.
Now, if we’re moving the CAR-T earlier lines of therapy, as in those two studies that I briefly mentioned with the Ide-cel and the Cilta-cel studies that are moving it to one to three prior lines of therapy, people are getting longer remissions.
Unfortunately, I do not have a crystal ball. I can look at your disease genetics. I can look at how deep your remission status is and I can generally predict based on other studies how long of a remission you might get, but it’s not a guarantee. What works for one person might not work for the other so you take it with a grain of salt. We just say, “Gosh, this is a great therapy. We need to offer it to you while we have that window of opportunity. You’re in a good remission. We have a slot for you. We’re going to pick the best product for you. Let’s give you this option.”
You might be one of those exceptional responders that are in remission for several years, which I do have people that have been in remission several years, fortunately.
Katherine Banwell:
Okay. Well, thank you so much for the thoughtful responses to those questions. As we close out today’s program, can you talk about some of the ongoing research in CAR T-cell therapy and what you’re excited about?
Dr. Beth Faiman:
Oh, my gosh. I am so excited about CAR T-cell therapy research. There are these what we call CRISPR gene edited technology, which is really personalizing the treatment in CAR-T.
There’s what we call an off-the-shelf approach where we don’t have to manufacture one’s T cells to be a fighter. So, these CAR T-cell therapies are the kinds of clinical studies where if you are in a position where you want to hopefully get an earlier access to a great therapy, this CRISPR edited at – Caribou is what it’s called, that we have at my institution. That might be right for you.
There’s also the different targets. For example, the Ide-cel and the Cilta-cel target what’s called BCMA or B-cell maturation antigen. Basically, the BCMA is expressed mostly on cancer cells and less so on healthy cells.
And so, that’s what the target is for these current CAR-Ts. We have different targets. So, what does that mean for you? If you had a CAR T-cell therapy against BCMA or a bispecific against BCMA now we have these different targets so that gives you other options for remissions status. So, if you can, I am a big, strong advocate for clinical trials. Like I said, it’s getting better access. You have a healthcare team. There’s so much stigma associated with clinical trials, but every single person is a candidate for some sort of a trial or another.
So, talk to your healthcare team or you can go to clinicaltrials.gov and then all the patient care organizations – International Myeloma Foundation, Multiple Myeloma Research Foundation, has access to clinical trial information as well for patients. So, yes, lots of good things. New targets. Off-the-shelf so you don’t have to manufacture. So, that represents new treatment options for many patients.
Katherine Banwell:
Dr. Faiman, thank you so much for taking the time to join us today.
Dr. Beth Faiman:
My pleasure. Thank you for having me.
Katherine Banwell:
And thank you to all of our collaborators. To learn more about myeloma and to access tools to help you become a more proactive patient, visit powerfulpatients.org. I’m Katherine Banwell. Thanks for being with us.