Chronic Lymphocytic Leukemia: Fran’s Clinical Trial Profile from Patient Empowerment Network on Vimeo.
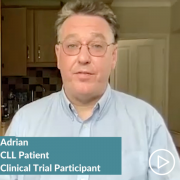
Chronic lymphocytic leukemia (CLL) patient Fran was diagnosed over 20 years ago and has traveled long distances for care. Watch as she shares her CLL journey and the benefits that she’s experienced from seeking out CLL specialists and clinical trials.
“I just think that clinical trials play such an important role in the future…we’ve come such a distance in my 20 years that we would have never come had we not had people that came before me in clinical trials.”
See More from Patient-to-Patient Diverse CLL Clinical Trial Profiles
Related Programs:
Transcript:
Fran:
Hi, my name is Fran, and I am 80 years young, just celebrated my birthday. And I have had CLL for 22 years. So, I developed CLL while I was still working as a nurse and as a diabetic specialist within a hospital setting. I was diagnosed as many are, by a simple blood test, having no symptoms. It was really done as part of my military requirement.
And I continued to work and continue my military career. I was a single parent, I am/was a single parent at that time, and I was raising three girls, so I had a busy life, and this was just a sideline as far as my health was concerned. I was in good health, but as the years went on, after two-and-a-half years, my count started to rise again, no symptoms. And the local oncologist that I was seeing decided that it was time for me to begin my first treatment, which was a very simple treatment again, as far as I was concerned, because it was an oral medication that I had no side effects whatsoever from, and it was easy to take once a day, and I did get some improvement in my blood work, of course. It did not put me in remission, but it brought down my numbers a little bit, and I was able to go sort of morally along for another two years when then it became evident again, not because of how I felt, but because of my numbers that I needed additional treatment. This treatment was a little bit more complicated because it was FCR, and that’s chemotherapy intravenous.
But I did say myself, “You need to start paying more attention to this disease,” and I went…I did go for a consultation at a university, about two hours from my home, and the physician was pretty direct with me and saying, “You need to start to pay more attention, get more information, have more testing done regarding the type of CLL you have,” at that point, it was the first time I had heard mutated, unmutated, which I know sounds probably a little crazy with my medical background. But again, I was able to put it in the rear-view mirror, the disease because I felt so well, and/or maybe it was denial.
I was able to come out of retirement and start to teach nursing part-time and work some other jobs. I got married. Life was good, I mean it was even better than good, and my pattern has been that I would get the treatment, get my CLL under control for about three to three-and-a-half years, that was about the time that I started, the numbers started to increase. And so my local oncologist here in Maryland said, “Well, we really need to be looking for something different,” and it was at that time when iguratimod (IGU) had just come out of clinical trials and been approved, so I was in this area, at least one of the first people in their practice to go on iguratimod.
Even though it’s not comfortable geographically, but to begin to look for a specialist and…so three years into iguratimod, I did that. I went to a university hospital setting, about three hours from my home and had way more thorough work-up, but more a work-up that included more tests that were able to give a clearer picture of my CLL, where it was at that point. And this group of doctors at this university setting said, Well, you were on track to maybe another year, and iguratimod to the end of the line as far as treatment for you, and you probably need to be looking at perhaps venetoclax (Venclexta) as your next option.
And I discussed actually with one of the local oncologists about going to see a specialist, and he encouraged me, he did not discourage me, he said, “We’d like to continue, we can play a role here, but we understand where you’re coming from.”
I am so glad that I made the decision, I did, because there is no doubt that this decision at the end of the iguratimod journey for me. I was going to be faced with another crossroads of where do I go from here as far as treatment, and I am quite sure had I not made the decision to go to a research university setting with a specialist that really is heavy into research.
I’m not sure that I would have…I would have ended up on a clinical trial, I’m not sure…I could have navigated all that myself, even with my medical background. Sure, enough the iguratimod did come to an end. And as I did, I was truly, really ready for venetoclax and a physician specialist, CLL specialist that had been at the university setting that I went to, as I mentioned, for my care, he had left that university and moved on a little further away from where I live, I contacted him just for an opinion, and he said, “Well, why don’t you come to see me?” I was in Florida at the time, and so I said, “Okay,” I would. And I did. And he broached the clinical trial.
The benefits definitely outweigh the risks for me. I didn’t realize that I was one of the first 10 or 12 people to take this drug, but I don’t think it would have made any difference because I knew that I had faith, first of all, in my physician and his knowledge, I had faith in the drug as they explained it to me, it was a new way of addressing mutations, and I just felt that this was a good pathway to be on, and that the risks, I felt would be handled by my physician and I would be watching for them, so…I do feel in my case, it was definitely worth the risk. I would say though, that people should really think and read and get as much information as they can about the specific trial that they’re considering, but know that there are just some questions, especially early on, that can’t be answered because they don’t know the answers.
I believe wholeheartedly in trials, and I would say that you have to deal with the, I think the emotion and the fear, the trepidation, this is something new, and try to work through that and concentrate on the positive. I just think that clinical trials play just such an important role in the future that you know of all of medicine, but particularly CLL we’ve come such a distance in my 20 years that we would have never come had we not had people that came before me, in clinical trials. On the other hand, I think you really do need to think about not only the immediacy, but the intermediate and the long range. What do I do if this happens or that happens? That I have to think of this.
This is part of my life now. This is something I have to commit to.
So it’s given me years with my family, with my girls, with my grandchildren, I’m getting to see kids off to college, into high school, Bob and I, my husband have had years that I never thought that I would have.