Tag Archive for: hematology
What Is the Role of Bispecific Antibody Therapy in the Future of Myeloma Care?
What Is the Role of Bispecific Antibody Therapy in the Future of Myeloma Care? from Patient Empowerment Network on Vimeo.
From the 2023 American Society of Hematology (ASH) annual meeting in San Diego, Dr. Peter Forsberg discusses how new data and learnings around bispecific antibodies may allow this newer myeloma therapy to be used more broadly in the clinical setting.
Dr. Peter Forsberg is associate professor of medicine at the University of Colorado School of Medicine and is a specialist in multiple myeloma. More about Dr. Forsberg.
Related Resources:

Dr. Peter Forsberg | Myeloma Research News From the 2023 ASH Annual Meeting |

|

What Myeloma Patients Need to Know About Bispecific Antibodies |
Transcript:
Dr. Peter Forsberg:
The role of bispecific antibodies is one that’s evolving quickly. We’ve had new therapies approved over the past 12 months. We may get more approvals in the future. And we’re certainly going to get increasing data around using those treatments in our clinics outside of the controlled clinical trial setting as well as maybe information around more diverse utilization in different treatment settings.
So, I think these are going to be medicines that are used much more broadly in the future than they are now. Right now, they have a really impactful role in a certain group of patients.
I think that’s going to become something that’s broader in the future. And I really do think there’s something that’s going to help us to improve on already a really good group of options in earlier relapsed settings and maybe even upfront treatment of myeloma in the future.
So, a lot to be figured out, a lot of refinement in the future about how and when to use these treatments. But it’s very clear that they’re going to have a huge impact in different settings.
Dr. Peter Forsberg | Myeloma Research News From the 2023 ASH Annual Meeting
Dr. Peter Forsberg | Myeloma Research News From the 2023 ASH Annual Meeting from Patient Empowerment Network on Vimeo.
Myeloma specialist Dr. Peter Forsberg reviews highlights from the 2023 American Society of Hematology (ASH) annual meeting. Dr. Forsberg shares what this promising news means for patients as well as advice for talking to your doctor about emerging therapies.
Dr. Peter Forsberg is associate professor of medicine at the University of Colorado School of Medicine and is a specialist in multiple myeloma. More about Dr. Forsberg.
Related Resources:
What Is the Role of Bispecific Antibody Therapy in the Future of Myeloma Care? |

|

|
Transcript:
Dr. Peter Forsberg:
My name is Peter Forsberg. I’m an associate professor at the University of Colorado. I am a specialist in multiple myeloma and other plasma cell disorders. And I’m here at ASH, where it’s always the most exciting time of the year for those of us in the hematology and hematologic/oncology community, where we are getting all the breaking information around all kinds of diseases.
But a really exciting time in terms of new findings for myeloma and the other diseases we deal with.
I think it covers a really broad spectrum. That’s been one of the really exciting things about myeloma over the past decade really is that we’ve had developments in so many different directions in terms of new therapies, new options for patients who need later line treatments, new options improving early line therapy.
Certainly exciting to have a couple of very big studies that are being presented this year, two Phase III trials that look at four drug combinations in the newly diagnosed myeloma setting, which both show fantastic effectiveness. So, hopefully, really going to help expand that for patients with new myeloma to get really the best treatment out of the gate. And then, really maturing data around new immune therapies, both in the settings where they’re currently approved, which are sometimes later lines for myeloma patients. And then, more data on earlier lines for those therapies where they’re likely to be used in the very near future.
At this meeting and over the past year, and ASH is always a big summation of a lot of the research that’s going on at any given time, the breakthroughs that are happening in myeloma, the innovation that’s happening in myeloma is very impactful for patients. It’s giving us great, improved options for earlier line patients allowing them to live better, live longer, preserving quality of life and then, giving us diverse new options in relapsed myeloma where we’ve had good tools but the broadening of that toolbox is very exciting.
And it allows new and really effective options across all kinds of patient types. So, it’s really impactful across different settings.
Patients shouldn’t hesitate to ask what are the new and developing treatment options, to ask their physicians are there new treatment options for myeloma that might be a fit for me now or in the future? Don’t hesitate to think about what might come down the road, even if you’re in a steady place with your myeloma because things are changing quickly.
Our options now are different than they were six or 12 months ago and they’re going to be different six or 12 months from now.
So, don’t hesitate to ask what’s new, what’s coming, should I meet with a myeloma specialist to discuss some of those specific options and whether they’re a fit for me. So, don’t hesitate to be the squeaky wheel a little bit and say what might be out there for me now or in the future.
Expert Perspective | Understanding the Recent FDA CAR T-Cell Therapy Warning
Expert Perspective | Understanding the Recent FDA CAR T-Cell Therapy Warning from Patient Empowerment Network on Vimeo.
The Food and Drug Administration (FDA) announced in December 2023 that it is investigating reports of secondary cancers in some patients who have undergone CAR T-cell therapy, noting that “the overall benefits of these products continue to outweigh their potential risks for their approved uses.” Timothy Schmidt, a myeloma specialist, shares his perspective on the recent news.
Dr. Timothy Schmidt is an Assistant Professor in the Department of Medicine, Division of Hematology, Medical Oncology and Palliative Care at the University of Wisconsin School of Medicine and Public Health. More about Dr. Schmidt.
Related Resources:

|

|
Transcript:
Dr. Timothy Schmidt:
So, in terms of the FDA update about CAR T-cell therapies, there was a recent warning, essentially, about an increased risk for a specific type of lymphoma involving T cells. And we don’t really know a whole lot about this just yet. But what we do know is that these events are rare and that we need to investigate it further. I think as of right now, this is not a huge area of concern for most of us, myself included.
When we have patients who are candidates for CAR T-cell therapy in multiple myeloma, generally, this means that patients are in need of a very effective treatment to get their disease under control and to do so for a long period of time. And the potential benefit of this therapy dramatically outweighs any of these kinds of long-term consequences or these newer things that are starting to develop. Now, I do think that this is something that we’re going to need to continue to keep an eye on. And we certainly can’t ignore this, especially as we start to move CAR T-cell therapy into earlier lines of therapy.
But as of right now, I would not weigh this very heavily in my decision whether to do a CAR T-cell therapy for somebody with multiple myeloma.
What Should Myeloma Patients Ask About Developing Research?
What Should Myeloma Patients Ask About Developing Research? from Patient Empowerment Network on Vimeo.
Myeloma research is evolving quickly, so what should patients ask their doctor to stay up to date? Dr. Timothy Schmidt, a myeloma specialist, shares advice.
Dr. Timothy Schmidt is an Assistant Professor in the Department of Medicine, Division of Hematology, Medical Oncology and Palliative Care at the University of Wisconsin School of Medicine and Public Health. More about Dr. Schmidt.
Related Resources:

|

|

Myeloma CAR T-Cell Therapy: How Does It Work and What Are the Risks? |
Transcript:
Dr. Timothy Schmidt:
I think that in terms of new and developing options, patients should be asking their healthcare provider, their oncologist if they have experience using some of these newer drugs, specifically, the bispecific antibodies and CAR T-cell therapies.
A lot of centers are starting to use these, particularly academic centers and some larger community centers as well. But not everywhere has experience using these. And so, asking your provider if it’s something that they would be a candidate for, particularly if the current treatment that patients are on is not working. And if your provider is not necessarily familiar with them, do they know somebody who is.
And could you go at least for a discussion to talk to a myeloma specialist about whether these medications are right for you or whether there’s a clinical trial that they might be a candidate for, because what we’ve learned is that earlier implementation of some of these really effective therapies can really be a big deal for patients with myeloma.
Patients can learn more about clinical trials from a variety of different outlets. I think the first place to start is with your local provider, your oncologist, asking that person if there is a clinical trial available. Most likely, the local provider is going to be able to point the patient in the right direction or at least let them know if something is going to be feasible for them. After that, often it involves reaching out to a local center, an academic center and getting a referral to somebody to see what is available at that site.
But there are also a variety of websites that can be used to search for clinical trials if there are particular patients who are very interested in specific therapies, CAR T, bispecifics, or others that you can look around and try to find places that would be best for them.
Myeloma Research Highlights From ASH 2023
Myeloma Research Highlights From ASH 2023 from Patient Empowerment Network on Vimeo.
Dr. Timothy Schmidt, a myeloma specialist, walks through research and treatment news from the recent 2023 American Society of Hematology (ASH) annual meeting.
Dr. Timothy Schmidt is an Assistant Professor in the Department of Medicine, Division of Hematology, Medical Oncology and Palliative Care at the University of Wisconsin School of Medicine and Public Health. More about Dr. Schmidt.
Related Resources:

|

Expert Perspective | Understanding the Recent FDA CAR T-Cell Therapy Warning |

|
Transcript:
Dr. Timothy Schmidt:
So, there’s constantly a lot of new information and data coming out about multiple myeloma and new therapies. I would say at this ASH ’23 meeting, I think the biggest highlight is further confirmation of the utility of using CD-38 antibodies in patients with newly diagnosed multiple myeloma. We have a plenary abstract for the use of isatuximab (Sarclisa) in combination with carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (Decadron) that I’m anxiously awaiting hearing the data of later today, as well as a late breaking abstract talking about the use of daratumumab in combination with bortezomib (Velcade), lenalidomide, and dexamethasone.
And both of these are studies that appear to show superiority of a four-drug regimen over a three-drug regimen. And we’re certainly looking forward to seeing the finalized data presented and extending the implementation of these highly effective therapies for patients with newly diagnosed multiple myeloma.
I think what we’re also seeing here is just further data being presented about bispecific antibodies, CAR T-cell therapies, and other novel combinations in the relapsed and refractory setting, as well as some really interesting insights coming out in terms of the myeloma pre-cursor setting of MGUS from the IStopMM Trial and some other research. So, really excited to learn more about how to use all of these exciting new tools that we’ve got for patients with multiple myeloma across the disease spectrum.
So, what this news means for myeloma patients is that outcomes are getting better. What it means is that we now know how best to use some of these tools that we’ve been developing for over a decade now in terms of maximizing responses, maximizing the number of patients who achieve remission and not just achieve remission but have a lasting remission in that first-line setting. And this is really going to lead to improved survival as well as improved quality of life when we start seeing year upon year of really high-quality survival from most of our patients with multiple myeloma.
We’re also learning how best to use some of the even newer therapies. T-cell directing therapies such as CAR T-cells and bispecific antibodies. We are incredibly excited about how effective these drugs are for patients with multiple myeloma.
And these are things that we’re already using in the clinic. And it’s important for patients to be aware so that when it becomes time to use these strategies that we can make sure that all patients have access to them.
Becoming an Empowered and [ACT]IVATED MPN Patient
Patient Empowerment Network (PEN) is committed to efforts to educate and empower patients and care partners in the myeloproliferative neoplasm (MPN) community. MPN treatment options are ever-increasing with research advancements in treatments and testing, and it’s essential for patients and families to educate themselves with health literacy tools and resources on the latest information in MPN care. With this goal in mind, PEN kicked off the [ACT]IVATED MPN program, which aims to inform, empower, and engage patients to stay abreast of up-to-date information in myeloproliferative neoplasm care.
The [ACT]IVATED MPN program is aimed at newly diagnosed MPN patients, yet it can help patients at any stage of disease. [ACT]IVATED MPN helps patients and care partners stay updated on the latest options for their MPN, provides patient activation tools to help overcome care disparities and barriers to accessing care, and powerful tips for self-advocacy, coping, and living well with a blood cancer.

Myeloproliferative Neoplasm Disparities
Race or ethnicity may have an impact on some health conditions, including MPNs. Cancer patient Lisa Hatfield interviewed Dr. Idoroenyi Amanam, Assistant Professor in the Division of Hematology at City of Hope. He explained about MPN risks and outcomes that may be impacted by patient race or ethnicity. “…we know that if you have high blood pressure, you have a higher risk for these complications-associated MPNs. And we know that African American males have a higher risk for that, so I think those things are…that example is a clear indicator that really identifying these basic risk factors that are related to diet, exercise, your weight, and other behavioral, possibly behavior-related factors may put you at higher risk to have complications from MPNs.”
Dr. Amanam further shared research findings and what needs further study to draw conclusions. “We have looked at incidences of thrombotic events in patients who have MPNs, and we tried to see if there was a difference between racial groups, and we didn’t. We did see that if you’re younger, you do have a higher risk of thrombosis over time, but there was no difference for if you were white, Hispanic, or African American. What we did find though, in a small single center study is that if you are non-white, there’s a higher risk of death over time. And I think we still need a lot of work to get a better understanding as to why that’s the case.”
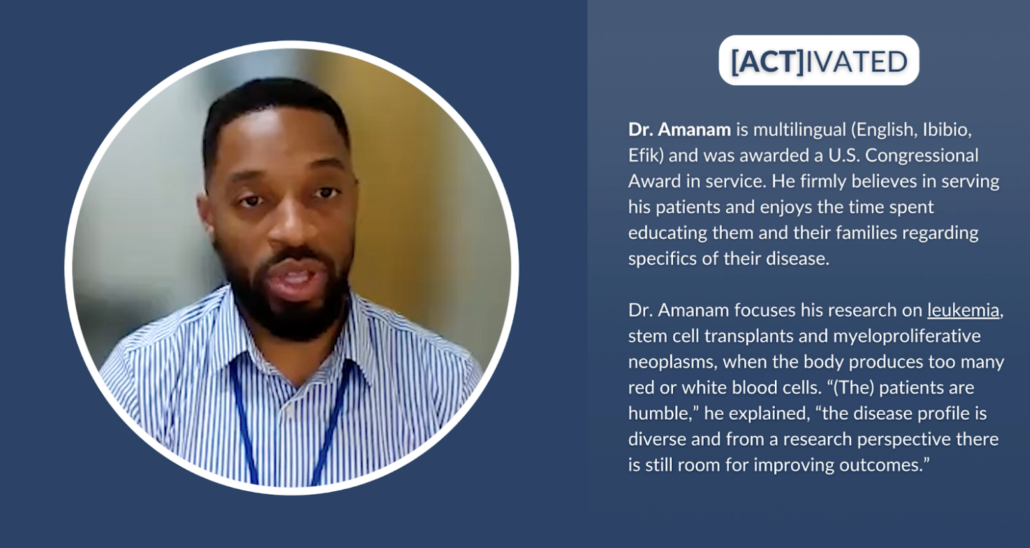
Solutions for Improved Myeloproliferative Neoplasm Care
Clinical trials are key in moving MPN research forward to improved treatments and care. Dr. Amanam shared his perspective about other players besides patients who can help move the needle forward. “I think that going back to the idea that we want to practice the best science, we want to be able to publish the best data. The responsibility is on the clinicians, the scientists, the clinical trialists, the drug companies, the institutions to really be able to structure clinical trials that are relevant to our real world experience. And so how can we better encourage that? I think from a government perspective, potentially incentivizing drug companies and institutions and the other major players that really are involved in pushing this field forward to practice better science.”
Dr. Amanam expanded on how clinical trials can be diversified. “And once we’re clear that being able to have a diverse participant pool will give us the best results and therefore will lead to your drug being approved. I think we will have more participants from all groups.”
Some underrepresented patient communities may experience obstacles to MPN care. MPN Nurse Practitioner Natasha Johnson from Moffitt Cancer Center provided advice to help patients. “Patients themselves can research clinical trials by looking at clinicaltrials.gov and see what’s out there and contact the academic center that’s performing those trials. There’s free information online that provides recorded sessions from conferences or speakers or speaking done by the MPN experts that you can just look to and get to easily to help understand the disease, knowing the symptoms, and then guiding treatment.” Natasha Johnson continued with additional advice for optimal care. “.…to try to get into a large cancer center or academic center and see an MPN expert. Many times, this is just by self-referral. Charity is sometimes provided through these. Zoom visits can be done as consults or follow-up visits. So my encouragement would be search these out, find out who the experts are, and contact them directly and see if there is any possibility or a way that you can get in to see an MPN expert for a consult so you can get the best care possible.”
Signs of MPN disease progression is something that patients and providers must be on the lookout for. Natasha Johnson shared her advice for patients to empower themselves against disease progression. “…monitor your blood cell counts, be your own advocate. Think about if they’re changing, could it be medication, or is it disease progression? Monitor your symptoms. Look at the total symptoms score or write down your symptoms and try to record where you’re at in intervals. Are things getting worse? If they are, don’t wait three months for your next appointment. Contact your healthcare provider and ask to be seen. Ask about getting a repeat bone marrow biopsy to establish where the current disease status is because that can open up doors possibly to more treatments.”
The future of MPN care has an additional approach to address. Dr. Amanam shared his perspective and how patients can help advocate for improved treatments. “I think in the next three to five years, we’re going to have drugs that are going to actually be able to treat the underlying disease before it gets to a point where you may need more aggressive therapy…And so it’s exciting where we’re going, and I think the questions that as a patient that I would ask are, because of the fact that we only have few FDA-approved therapies, are there any clinical trials that are able to target the underlying disease as opposed to just treating the symptoms? I think that’s very important for the patients to ask, especially in this space now.”
Rates for stem cell transplant approvals must improve for lower income groups and for African American and Hispanic groups to provide better health outcomes for blood cancers like MPNs. Dr. Amanam explained what’s involved with transplants and how others can help as donors. “You can donate your bone marrow, or you can donate your stem cells that are not inside of your bone marrow. And typically as a donor, your experience of actually donating is about a day. And the recovery time after you donate your bone marrow or stem cells, it’s typically within about one to three days. So the benefit of donating your stem cells or bone marrow outweighs the inconvenience of a day or a couple of days of your schedule being altered. So I think that’s really important to understand. And I think if we can get more people to be aware of this, I think we can definitely get more donors.”
![[ACT]IVATED Program Logo](https://powerfulpatients.org/wp-content/uploads/Screenshot-2023-08-24-at-3.03.57-PM-1030x586.png)
[ACT]IVATED MPN Program Resources
The [ACT]IVATED MPN program series takes a three-part approach to inform, empower, and engage both the overall MPN community and patient groups who experience health disparities. The series includes the following resources:
- Myeloproliferative Neoplasm Basics for Newly Diagnosed Patients
- Are MPN Risks and Outcomes Impacted by Race or Ethnicity?
- What Does the Future of Myeloproliferative Neoplasm Care Look Like?
- Are There Any MPN Disparities in Subtypes and Genetics?
- Have MPN Disparities Been Addressed by Institutions?
- MPN-Related Complications | Are BIPOC Patients at Higher Risk?
- How Can MPN Clinical Trials Be Diversified?
- Understanding MPN Treatment Goals and Shared Decision-Making
- Are There Disparities in Stem Cell Transplant Outcomes?
- Bone Marrow Registries | What Myeloproliferative Neoplasm Patients Should Know
- Graft-Versus-Host Disease Risk for BIPOC Patients
- Emerging MPN Therapies in the Research Pipeline
- How Can Myeloproliferative Neoplasm Care Barriers Be Overcome?
- Myeloproliferative Neoplasm Financial and Care Resources
- How Can Underrepresented MPN Communities Access Support?
- [ACT]IVATED MPN Resource Guide
- [ACT]IVATED MPN Resource Guide en español
- [ACT]IVATED MPN Patient Vignettes
- [ACT]IVATED MPN Activity Guides
Though there are myeloproliferative neoplasm disparities, patients and care partners can take action to empower themselves to help ensure optimal care. We hope you can take advantage of these valuable resources to aid in your MPN care for yourself or for your loved one.
[ACT]IVATED MPN Resource Guide en español
[ACT]IVATED MPN Resource Guide
How Have Advances in Testing Impacted AML Care?
How Have Advances in Testing Impacted AML Care? from Patient Empowerment Network on Vimeo.
Recent testing advances have dramatically improved care for AML patients. Dr. Ann-Kathrin Eisfeld discusses these improvements and why every AML patient should undergo in-depth molecular testing before making a treatment choice.
Dr. Ann-Kathrin Eisfeld is Director of the Clara D. Bloomfield Center for Leukemia Outcomes Research at The Ohio State University and a member of the Leukemia Research Program at the OSUCCC – James. Learn more about Dr. Eisfeld.
Related Resources:

|

|

|
Transcript:
Katherine Banwell:
Dr. Eisfeld, the landscape of AML has changed significantly in recent years. How have advances in testing improved patient care?
Dr. Eisfeld:
It is a different world, Katherine, honestly. I mean, I started practicing in hematology in taking care of AML patients back in Germany actually in the year 2007.
Back then, there was no other testing that was available. All we were guiding and all that we had available was morphology and cytogenetics
And very often, it was very inaccurate. And we also only had two treatment kinds available. One was intensive chemotherapy, and one was something that was just a little bit better than best supportive care. So, many patients could not receive treatment. And the increase in knowledge that we have on a molecular level in AML really did two things at once. On one, we understood we had a more finetuned understanding on which patients would respond. And the second thing is that this knowledge about the molecular landscape enabled us to have new treatments available that are sometimes in pill form that can target specific mutations in patients who carry these genetic changes.
Katherine Banwell:
Should all AML patients undergo in-depth testing like biomarker testing or cytogenetics?
Dr. Eisfeld:
Yes. Every patient should do that. It can make the difference between life and death. And it can make the difference between receiving – having a hospital stay of four weeks with intensive chemotherapy versus taking the pill at home. This is very rare that this is possible. But it is possible. And of course, you – one would not want to miss this chance if it would be possible.
Katherine:
I’d like to get your thoughts on where we stand with progress in the field of AML. What would you like to leave the audience with? Are you hopeful?
Dr. Eisfeld:
I am incredibly hopeful. I hope – when I started working in hematology, as I said at that time, it was just about when imatinib (Gleevec) came out. Which is this CML pill that really revolutionized care. And so, at that time, I would be – all patients on that bone marrow transplant service had chronic myeloid leukemia. And because they all had to undergo bone marrow transplant. Then Gleevec came, and today, there are no such patients who are see or very rarely that require such intensive care.
So, I am very hopeful that in my practice time, which hopefully –and even earlier on – that there will be a time where we find targeted therapies for almost all patients.
Developing Research and New Myeloma Treatment Options
Developing Research and New Myeloma Treatment Options from Patient Empowerment Network on Vimeo.
What are the new developments in myeloma treatment and research? Dr. Brandon Blue discusses how the landscape of myeloma care has changed in recent years and treatment options for high-risk myeloma, and he shares developing research that patients should know about.
Dr. Brandon Blue is Assistant Member and Clinical Instructor in the Department of Malignant Hematology at Moffitt Cancer Center in Tampa, FL. Learn more about Dr. Brandon Blue.
Related Resources:

What Myeloma Patients Need to Know About Bispecific Antibodies |

Myeloma CAR T-Cell Therapy: How Does It Work and What Are the Risks? |

|
Transcript:
Katherine Banwell:
Dr. Blue, the landscape of myeloma care has changed significantly in recent years. Are there new factors to consider when working with a patient to choose a treatment approach?
Dr. Brandon Blue:
Yeah. The good thing about myeloma is it’s literally always changing, and that’s a great thing. Compared to some of the other cancers, or really even other diseases, sometimes we’ve been using the same things since the ‘90s. But luckily for myeloma every couple years we get something that’s bigger, and typically better. So, right now some of the new things that are available for patients are all the way from newly diagnosed, all the way to people who have relapsed disease. So, we have a lot of different options that we can potentially go into.
Katherine Banwell:
Dr. Blue, what treatment options are available for myeloma that’s considered high-risk?
Dr. Brandon Blue:
Yeah. So, unfortunately, there’s some people who have multiple myeloma whose disease does not follow the standard pattern. Unfortunately, what happens is that there are certain mutations that actually happen in the biology of those cancer cells that actually cause them to survive when they should be dying. And unfortunately, that means that sometimes the chemotherapy and the medicines that we give them becomes a little bit more resident.
A lot of times when we give people treatment the one question they ask is, “How long will it last?” But, unfortunately, there’s some people who have those high-risk features that unfortunately, despite whatever numbers we tell them of how long it may last, theirs actually may last a little bit shorter, and the disease may come back a little bit quicker. So, what we have to do as the doctors, and as the team, taking care of these patients is maybe do things a little bit more outside of the box, and do things that might tend to be a little bit more aggressive.
Because sometimes we have to match the aggressiveness of the disease. If the cancer itself is starting to be high-risk or aggressive, sometimes we may have to do some nontraditional things to kind of make sure that they have a good outcome and a good result.
Katherine Banwell:
Dr. Blue, is there developing research that myeloma patients should know about? And what are you hopeful about?
Dr. Brandon Blue:
Yeah. One of the things that happens right now is that we have CAR T that’s available for patients got approved by the FDA. However, the CAR T product that we currently have available only have one target, which is called the BCMA, or B-cell maturating antigen.
Which is part of the plasma cells, however, there are so many other targets on the plasma cells that potentially can be targets for new medications. And the good thing is that there are actually new CAR T and medications that are being developed that actually target other things other than the BCMA.
So then, it may come to the point where people get more than one CAR T down the road, and I think those are exciting clinical trials. Because if there’s multiple targets, and there’s multiple CAR T, maybe we can sequence them in a way that maybe we find a cure for the disease one day.
Katherine Banwell:
That’s exciting.
Dr. Brandon Blue:
It is.
Katherine Banwell:
Dr. Blue, thank you so much for joining us. Do you have anything else you’d like to mention?
Dr. Brandon Blue:
I just want people to know that it’s okay to get a second opinion. I think that regardless of what’s happening in your care, sometimes it’s always good just to have someone, especially someone who’s what they call a myeloma specialist, to review your case, and just make sure that you’re on the right road, and that things are going well for you. So, it’s something that I would recommend for anyone to do.
How Is Bispecific Antibody Therapy Changing Myeloma Care?
How Is Bispecific Antibody Therapy Changing Myeloma Care? from Patient Empowerment Network on Vimeo.
How does bispecific antibody therapy work? Dr. Brandon Blue explains the benefits of bispecific antibody therapy and how this treatment may be quicker to access for patients.
Dr. Brandon Blue is Assistant Member and Clinical Instructor in the Department of Malignant Hematology at Moffitt Cancer Center in Tampa, FL. Learn more about Dr. Brandon Blue.
Related Resources:

What Myeloma Patients Need to Know About Bispecific Antibodies |

|

Questions and Considerations When Making Myeloma Treatment Decisions |
Transcript:
Katherine Banwell:
Dr. Blue, can you tell us about bispecific antibody therapy for myeloma?
Dr. Brandon Blue:
Yeah. So, bispecific is basically similar to CAR T in a way that it uses the body’s immune system. But the big difference with bispecific therapy is that not only does it attack the plasma cell, which is the typical cancer cell in multiple myeloma, but it also brings the cancer cell to the actual immune system.
So, it’s one thing to kind of go after the cancer cell, it’s another thing to say, “Hey, here’s the immune system, here’s the cancer cell. Let me figure out a way to marry the two of them together so that the fighting really takes place in real time.” And luckily, we’ve seen some really fantastic results.
Katherine Banwell:
So, how is this therapy changing myeloma care?
Dr. Brandon Blue:
The big thing about bispecifics is that they’re a much quicker process than CAR T.
Right now, one of the things that is slowing up the CAR T process is something called manufacturing time. And so, even if someone wanted CAR T today, they may not be able to get it for six to eight weeks due to that manufacturing time. However, these bispecific are typically readily available so that if you need them today, probably by tomorrow, the next day, they can be infused. And so, that’s a much quicker time, and that allows patients to get the treatment that they need.
Because, again, these are patients who, unfortunately, disease has not responded to a lot of the more traditional therapies. So, they need help, and sometimes they need help quickly.
Accessing Myeloma CAR T-Cell Therapy Clinical Trials
Accessing Myeloma CAR T-Cell Therapy Clinical Trials from Patient Empowerment Network on Vimeo.
How has CAR T-cell therapy changed the landscape of myeloma care? Dr. Brandon Blue shares how this therapy has been a “game changer” in myeloma care, and how clinical trials for newer CAR T-cell therapies are advancing care and access for patients.
Dr. Brandon Blue is Assistant Member and Clinical Instructor in the Department of Malignant Hematology at Moffitt Cancer Center in Tampa, FL. Learn more about Dr. Brandon Blue.
Related Resources:

|

Questions and Considerations When Making Myeloma Treatment Decisions |
Transcript:
Katherine Banwell:
Dr. Blue, we know that the approved CAR T-cell therapies are for patients who have already undergone several lines of treatment. How has this therapy revolutionized care for myeloma patients?
Dr. Brandon Blue:
Yeah. So, CAR T is really a game changer when it comes to multiple myeloma. I’ll tell you that previously people have seen a lot of the best medicines that we have, and unfortunately for a good percentage of people the disease just becomes what we call refractory.
And unfortunately, despite us giving them the best medicines, the disease still likes to survive. So, we had to think of something of what can still kill cancer, but may not be the traditional chemotherapy that people may think of? So, we say, “Well, let’s come up with CAR T because it’s a way to actually use the body’s own immune system to fight off those cancer cells.” And for myeloma it really has shown a lot of progress. And one of the things that we know now is that not only do we have one, but we have two products, and maybe even a third coming down the pipeline because there’s more and more of this CAR T becoming available.
And that’s better, and better for patients.
Katherine Banwell:
Absolutely. That’s great news. For patients who are recently diagnosed, Dr. Blue, is there any chance of accessing this treatment sooner? Maybe through clinical trials.
Dr. Brandon Blue:
Yeah. One of the biggest clinical trials that I think that people are excited about is trying to challenge something that we’ve been doing since the 1980s, which is stem cell transplant.
So, typically, when a person get diagnosed with multiple myeloma, especially newly diagnosed, stem cell transplant is typically part of the treatment plan. But now there’s clinical trials that are coming out where we challenge instead of maybe a patient going to stem cell transplant, maybe they might do CAR T instead. And we’re trying to figure out can something that we’ve been doing since the ‘80s be un-throned as the best standard practice? And so, I think that’s something that people are really excited about, that’s something I’m excited about.
And it gives people who are newly diagnosed a chance to get some of this novel therapy.
Katherine Banwell:
I have a follow-up question about the clinical trials, you mentioned that there is one going on. Where is it taking place?
Dr. Brandon Blue:
Yeah. So, it’s actually a multi-center study. And so, hopefully, we hope to have Moffit Cancer Center involved in that clinical trial, but it’s multiple different sites really all over the world because I think this is a question that everybody’s really excited about. Again, like I said, transplant has been happening since 1980s, and so for some treatment to come along to potentially challenge that, I think people are excited about a new contender. And we’ve already seen the progress that CAR T has already made.
And so, the big question is how well will it work when someone is newly diagnosed before their body has really seen all the extra treatments that are there? Will it work even better?
We’re very hopeful, and we’re very optimistic.
Katherine Banwell:
Where can people find out about this particular clinical trial and other clinical trials?
Dr. Brandon Blue:
Yeah. So, I tell people there’s so many different websites and resources. One of the main ones that is very readily accessible is clinicaltrials.gov, is very kind of easy, and intuitive. Typically, what you can do at clinicaltrials.gov is you can literally kind of just type in your disease process, and then they’ll tell you if it’s newly diagnosed, or relapsed. There’s also a place called SparkCures. SparkCures is fantastic organization that really tries to focus people, and get them matched with clinical trials, which is fantastic.
There’s also HealthTree. HealthTree not only helps people from a clinical trial standpoint, but they also have patient support programs because nobody wants to be in the fight for cancer by themselves. The American Cancer Society does a fantastic job, as well as Leukemia & Lymphoma Society.
The International Myeloma Foundation, or the IMF, and then the MMRF, the Multiple Myeloma Research Foundation. And there’s many more, but those are some of the top ones that we readily use that have a lot of information. And some of them have not only information for the patient, but also information for the family, and the caregivers. Because again, when someone gets diagnosed with cancer it doesn’t just affect the person, it affects the whole family.
How Are Myeloma Patients in Remission Monitored?
How Are Myeloma Patients in Remission Monitored? from Patient Empowerment Network on Vimeo.
How often should testing be administered when myeloma is in remission? Dr. Brandon Blue discusses how patients in remission are monitored and when a bone marrow biopsy may be required.
Dr. Brandon Blue is Assistant Member and Clinical Instructor in the Department of Malignant Hematology at Moffitt Cancer Center in Tampa, FL. Learn more about Dr. Brandon Blue.
Related Programs:
|

Should You Push for a Stronger Myeloma Treatment at Relapse? |

Questions and Considerations When Making Myeloma Treatment Decisions |
Transcript:
Katherine Banwell:
Dr. Blue, how often should bone marrow biopsy be performed in the years following a stem cell transplant?
Dr. Brandon Blue:
So, typically following stem cell transplant patients are kind of switched to what we call maintenance therapy.
Meaning that the disease is typically under control after transplant, and our job right now is to kind of put the lid on the disease and keep that lid on so that the disease doesn’t kind of bubble over. And likely, people are on that maintenance therapy for three, four, sometimes even five years, or more. And so, sometimes when the disease is very stagnant or very stable, and people are on maintenance therapy, there may not be a need for multiple repeated bone marrow biopsies.
Because the disease may just be in a kind of dormant or remission stage. However, at the first sign that we see that things are changing, we see that unfortunately the disease may be starting to relapse, or maybe even there’s a new pain, or things happening that just need further investigation, I think a bone marrow biopsy would be very warranted at that time.
Katherine Banwell:
Okay. So, when patients are in a kind of remission stage you just monitor them. Do you continue to do bloodwork, and test their urine, and so on?
Dr. Brandon Blue:
Blood, urine, imaging. Blood, urine imaging.
Katherine Banwell:
Yeah. Blood, urine, imaging.
Dr. Brandon Blue:
Yup. Those would be the best ways to follow it. Of course, the gold standard would be a bone marrow biopsy, but typically what happens is that the blood, the urine, and the imaging typically reflect what’s happening in the bone marrow. It’d be sometimes very unlikely for a patient’s bloodwork to be normal, but then the bone marrow to be ridden with cancer. Typically, it doesn’t work that way. There are some unique circumstances where bone marrow biopsies are needed in people who have something called non-secretory myeloma, but that’s a very small percentage.



