Everyone living with cancer understands the dangers of their disease. But did you know that infections cause, or are involved in, about 60% of all deaths for cancer patients? This is because many cancers, and many cancer therapies, can weaken your immune system. As you enter each phase of treatment, your doctors will prepare you for what to expect, but here are 7 things every patient with cancer — and those around them — need to know about infections.
1. Know if you’re at risk, and when.
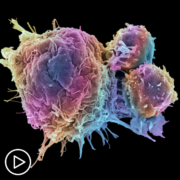
Almost 20 million people are diagnosed with cancer each year, and nearly all cancer patients are likely to be immunocompromised at some point (or points) of their disease course. Hematologic cancers like leukemia, lymphoma, or multiple myeloma can weaken the immune system themselves, and certain solid cancers are related to diseases that weaken the immune system, like AIDS.
But even if your disease doesn’t impact your immune system, the treatment might. Most patients undergo treatments with chemotherapies, which attack the fast-dividing cells of the cancer, but also bone marrow that manufactures immune cells. Similarly, common treatments for blood cancers involve destroying and replacing bone marrow to reboot the immune system. Your doctor will inform you if you enter a treatment phase that requires extra caution and vigilance.
2. Understand the dangers of infections for the immunocompromised.
Patients with cancer may have unique challenges from infections that people with fully functioning immune systems may not. The most obvious issue is your body can’t mount its usual defense, leaving you unable to fight off what would be otherwise routine illnesses. Also, you are susceptible to certain types of pathogens, like certain fungal infections and hospital-acquired infections, that a healthy immune system would block early.
Importantly, your body’s common tools against infection — fever, inflammation, increases in certain easily-detected immune cells — are often the telltale signs of an infection. If they don’t occur normally, it’s easier to miss red flags of early disease, when treatment is often easier.
3. Protect yourself to avoid infection.
The best defense against infection is to not get one. Living through the pandemic has likely made you familiar with some common tools and strategies to minimize exposure to infectious diseases: wear the right mask, wash your hands frequently, and avoid contact with sick people and crowds. Vaccines can be important armor against infections, especially if you are not yet immunocompromised — but may become so later in treatment. (Your doctor can guide you on which vaccines to update.)
If you are already immunocompromised, it’s important for those around you with healthy immune systems to get vaccinated. They become your first line of defense.
If your white blood cell counts are low, you are considered neutropenic. Neutropenic patients should avoid hiking, where you risk exposure to molds growing in natural environment that might be dangerous. Similarly, avoid construction sites, which tend to aerosolize dirt — increasing the spread of dangerous pathogens.
4. Know the signs of infection.
Sometimes getting sick may be unavoidable. Infections may present differently in immunocompromised patients, depending on the type of infection, immune status, and how far a disease has progressed. But there are signs to watch for:
Fever.
This is the number one red flag, though it can be hard to interpret. When patients with low white blood cell counts have a fever it’s called febrile neutropenia. Because of the danger in developing a blood infection that escalates to life-threatening sepsis, patients will often be placed on broad-spectrum antibiotics immediately when presenting with a fever, though more accurate treatment. Fever, however, can also be a sign of cancer progression.
Respiratory symptoms.
Things like shortness of breath or difficulty breathing can be signs of lung infection and pneumonia.
Acute pain.
As with many symptoms, pain in the chest or abdomen are not necessarily signs of infection, but need to be investigated in immunocompromised patients
Weight loss.
Weight loss is associated with serious infections like tuberculosis, which may be slow to show symptoms in patients with compromised immune systems.
Fatigue.
Another symptom that can have many causes.
5. Have a plan.
Don’t let the signs of infection catch you off-guard. The point at which you’ll be most at risk of infection is often predictable — for example, when white blood cell counts have dropped just after chemotherapy. This can help you prepare and stay vigilant.
Typically, doctors will advise blood cancer patients with signs of infection not to go to an emergency room — mixing with a general population of acutely ill patients could expose you to other dangerous pathogens.
But that doesn’t mean to ignore symptoms or avoid care — if you wait until you experience drops in blood pressure or spiking fever, the outcomes could be worse. Instead, many oncologists recommend you call your cancer clinic, where your potential infection can be addressed by your doctors in a controlled setting. It’s understandable that patients will not want to be admitted too early, but early treatment tends to give better results. Make a plan with your specialists before you wind up in harm’s way. Speak with your family members so they know how to help you if you are in need. And know where you need to go.
6. Stay safe in the hospital.
The most common infections for immunocompromised patients are from opportunistic pathogens. This can include hospital-acquired infections, which is why most specialists will help you try to avoid the hospital if possible.
But sometimes it’s unavoidable. In these cases, you will most likely be transferred in from your cancer center or — after a phone call to your specialist — directly from home, avoiding the ER. Often, this means you will be in a dedicated cancer ward, intensive care, or otherwise segregated from people with normal immune systems. In any event, health care providers will be wearing masks and other protective gear to prevent exposing you to new pathogens. Hospitals also have additional safety protection like HEPA air filters and rigorous protocols to prevent contamination.
7. Be ready for the fight.
Clinicians will often use empiric antimicrobial therapy for cancer patients showing signs of infection. Under this approach, doctors begin the process of testing for the specific pathogen, but simultaneously start the patient on a broad-spectrum antimicrobial therapy while waiting for the results of testing. If testing can identify a specific cause, the doctors can switch to a more directed therapy that is appropriate for the specific illness.
If they can’t, there is still a chance the signs of infection will resolve, sometimes without ever finding a specific diagnosis. Those patients may have endured additional suffering, remained at elevated risk for new infections in a hospital setting, or encouraged antimicrobial resistance by treating a pathogen with an inappropriate treatment course. In the worst-case scenario, failure to identify the right pathogen may lead to worse outcomes for the patients.
The good news is that diagnostic testing is improving, and there are novel, highly accurate tools to help doctors get their patients on the most appropriate therapeutic course faster. This means directed treatment for more patients, earlier in the course of disease, for better outcomes with less antimicrobial resistance.
Sarah Park, MD, is a pediatric infectious diseases physician at Kapi’olani Medical Center for Women & Children in Hawaii. She is also an assistant clinical professor in the department of pediatrics at the University of Hawaii John A. Burns School of Medicine, and Medical Director of Medical Affairs at Karius Inc.