How Can Lung Cancer Disparities Be Addressed? from Patient Empowerment Network on Vimeo.
Lung cancer disparities work against care for some patients, but how can they be addressed? Expert Dr. Christian Rolfo from Mount Sinai explains some disparities in patient populations and how care can be improved for these underrepresented patients.
See More from Best Lung Cancer Care
Related Resource:
Transcript:
Dr. Nicole Rochester:
So I’d love for you to talk a little bit, Dr. Rolfo, about some of the challenges related to appropriate access to lung cancer care as it relates to different socio-demographic populations, and then how can we begin to address those disparities.
Dr. Christian Rolfo:
Yeah, this is a topic that is really in my heart because I was coming with you before we start the communication, the recording of this. I was working in Europe before coming to the United States. I was shocked by the disparities that we see in some healthcare situations, so in my position before in Europe, we have a healthcare system that discovering for patients and we have, obviously, difficulties, but here I saw in some communities really under-served in terms of access to different service and healthcare is one of them.
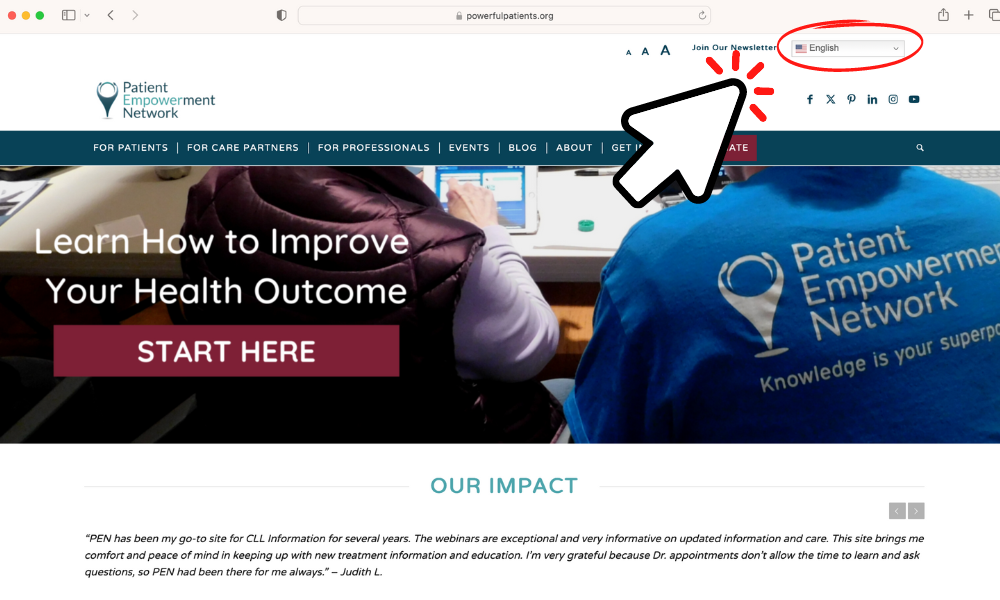
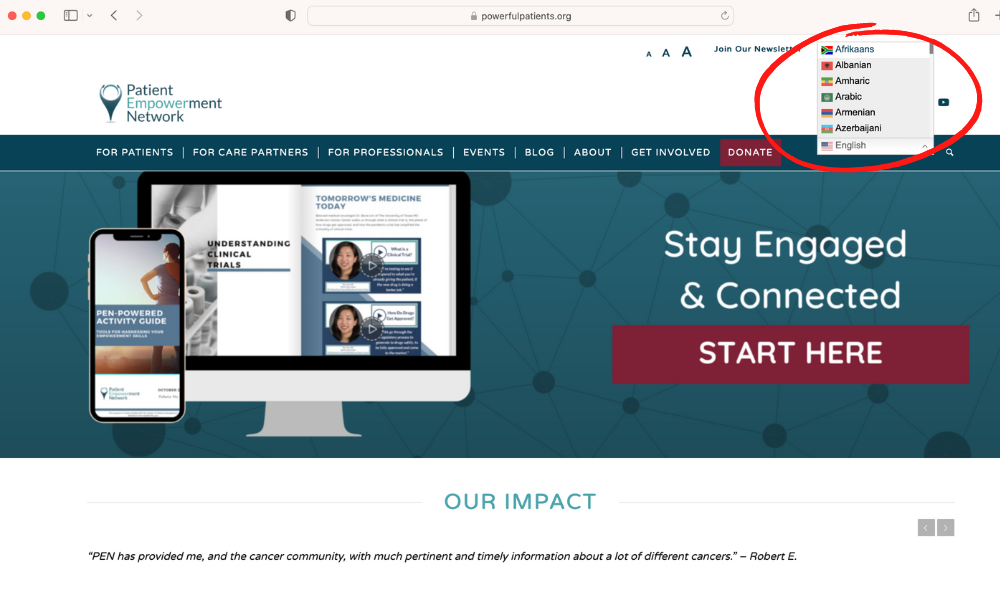
So we need to be conscious about that when we have patients that are struggling to get transportation, we have patients that are struggling to get approval for some drugs. So, there are a lot of areas that need to be addressed, disparity also in terms of language, we have also patients that are not understanding the doctors, we have patients that are having difficulty when to get to the app information when we are saying, Oh, you can see your report in your app, so it’s not easy for some of them, we have generational gaps as well, these are disparities as well. So taking or being conscious of all these factors is making us take action and how we can take actions in our institutions, and in several institutions in the country, we have the support of an experienced team that is addressing that, and teams are specific that are working for disparities. Some of them are social workers, some of them are advocate patients, so we have a big team of institutions that are helping to the patients to go for different scenarios, and even we have patients that are homeless, so how we treat patients in these conditions when we know that the patient is in a shelter, so if you have toxicity, what will we be doing. So all these things are taken into consideration, believe me, because it is like New York, you have a big disparity of or a big diversity, and we say of populations in one consultation morning, you can see all of them in your waiting room, so we need to try to address all this, and there are politics that are coming from us as a healthcare system, but there are also politics that they need to come from governmental politics, so try to use these…all the tools that we have at our disposal are important, and also we have a very good support of advocacy groups.
And this is something that I want to really profit their patient to say thanks because we have several, several advocacy groups that are doing a terrific job from testing to helping patients to go through this journey. So it’s really an important job, and obviously families, families are helping to these disparities and patients, so patients themself. So what I say always to the patient, raise your voice, empower yourself. Try to ask for your rights if you don’t understand your doctor… Ask again, if you want to have a second opinion, talk to your doctor, that is the most important thing. We are very open to help the patients, and that is our mission. So if I say to my patients, If you want to have a second opinion, please let me know, and I try to direct you to somebody who is an expert in the field and can help us to learn better your disease or your treatment, but I think it’s a situation that everyone is winning, especially the patient, but also ask for future patients understanding better every case.