“Tell me a fact and I’ll learn. Tell me a truth and I’ll believe. But tell me a story and it will live in my heart forever.” North American Indian proverb
As a patient or caregiver you may be asked to share your personal story with others. Your story serves as a powerful tool for raising awareness and offering valuable insight into the patient experience. Stories can be a bridge between the technical, rational world of scientific practice and the experiential world of patients. Stories also create a shared sense of meaning and community in our lives, lessening the isolation many of us feel when faced with a chronic illness.
The Power of Story
Stories have existed in our culture from the beginning of time. We use stories to derive meaning from experience and to pass along knowledge and wisdom. Recent breakthroughs in neuroscience reveal that your brain is in fact hardwired to respond to story. Your brain on story is different from your brain when it is receiving any other form of information, including straight facts and data. While facts and figures engage a small area of the brain, stories engage multiple brain regions that work together to build rich emotional responses.
In 2010, a group of neuroscientists at Princeton University used an fMRI machine to monitor what was going on inside the brains of both story-tellers and listeners simultaneously. They discovered that whilst the speaker was communicating to the listener, both their brains showed very similar activity across widespread areas. Their brains were effectively ‘in sync’ with one another suggesting a deep connection between storyteller and listener.” [1]
Tapping the Power of Patient Stories
Humans have an innate desire to feel connected with others who live life through similar lenses. When I first started telling my own story on my blog Journeying Beyond Breast Cancer, I did so in the hope that others on the same path might find some resonance and the knowledge that they are not alone. Chronic illness can be an isolating experience but the very act of sharing our stories with others counteracts the isolation we so often feel. It carries within it the seeds of community and connection which makes us feel less alone in our journey. Diabetes patient advocate and blogger Renza Scibilia captures this feeling when she writes: “There are billions of stories in the world and when we find people we connect with, we reach out and want to hold on. I know that’s how I feel about the Diabetes Online Community – I hear familiar stories and want to grab onto them and the people who wrote them because they help make sense of my diabetes life.”
Patient advocate and author, Jackie Barreau, believes the importance of sharing her personal story lies in “the ability to connect, empower and help others. It is also uplifting and inspiring to hear of people’s hardships whether through illness or unfortunate life events and the positivity & optimism they convey”. Not only can sharing your story lessen feelings of isolation and open up new avenues of support, it can also offer vital diagnostic clues when others are searching for answers. Jackie explains, “through my volunteer work with for example, the Unicorn Foundation, as an admin for an online patient support group I see first-hand patients joining our group due to lack of knowledge and misinformation provided by their general practitioners and also physicians.”
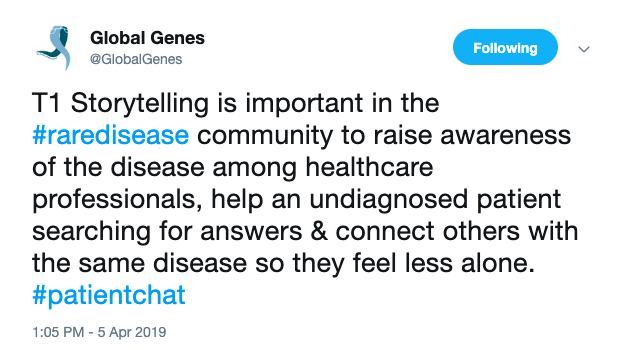
The National Gaucher Foundation of Canada has coproduced an excellent storytelling toolkit with rare disease patient advocacy organization, Global Genes. It states that “medical terminology and data, though undeniably important, can obscure what it means to live with a disease and make it difficult for most people to relate. Personal stories, though, frame our individual experiences in a way that lets others connect and find diagnostic clues that may have been missing.” Isabel Jordan, the mother of a son with a rare disease, credits reading a patient’s blog to help her finally see the pattern in symptoms in her own son’s life, which set them on a new diagnostic path. “As a parent of a child with a rare disease I’m constantly looking for patterns, for clues, for ideas of what could be next in our diagnostic journey,” she writes, “I look for researchers, doctors, other connected parents to see what they are posting. It was through reading someone else’s blog that I could finally see the pattern in symptoms in my own son’s life. Connecting the dots by seeing them in someone else let me provide valuable clues to our own clinician researchers and now we’re heading down a new diagnostic path.”
How To Tell Your Story
Whether you tell your story through public speaking, print or online social media, take some time to plan ahead for what you will share and how you will share it. Speak from the heart; be accurate, honest and persuasive. The following questions will help you to develop your story in order for it to have maximum impact.
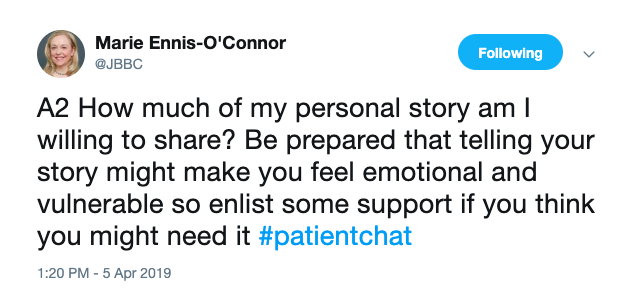
- How much of my personal story am I willing to share? Be prepared that telling your story might make you feel emotional and vulnerable so enlist some support if you think you might need it.
- What is too private to share? Let the audience know your boundaries.
- How comfortable is my family with me talking about my story (or theirs)?
- What supporting material will make my story stronger? Can you use pictures, research data, and statistics to support your story? Create an experience in images that evokes an emotional response.
- What is the main take-home message you wish to leave your audience with? Focus on two or three main points for clarity.
- What do I want my listener to do when I am done? Do you want your listeners to take action after hearing your story? Outline clearly the next steps they can take to do so.
Taking the decision to share your story is a personal one. Emma Rooney, a rare disease patient advocate has this to say:
“I’ve been telling stories since I was a child but my health story always seemed like something to keep private. Despite living with a rare disease my entire life, it wasn’t until becoming a young adult that I decide to share my journey with Gaucher disease. Openness to sharing has led me to other patients who have similar health experiences, and also connected me with stories that are very different from my own. This diversity helps me to better understand my condition and to connect the dots with new information. Storytelling has provided a type of healing that drugs alone can’t offer. My health is an evolving story, and continuing to be a storyteller is part of my wellness strategy and my way to contribute to the global community of patient advocates.”
Each of us has a compelling story to tell; a story with the power to build connection, increase understanding, and move others to take action. Developing our skills as storytellers is a powerful tool in our patient advocacy toolkit. Your story is a precious resource; use it wisely and well.
[1] PNAS.org: Speaker–listener neural coupling underlies successful communication by Greg J. Stephens, Lauren J. Silbert and Uri Hasson.
A Stanford Medicine X e-Patient scholar, Marie Ennis O’Connor is an internationally recognized keynote speaker, writer, and consultant on global trends in patient engagement, digital health and participatory medicine. Marie’s work is informed by her passion for embedding the patient voice at the heart of healthcare values. She writes about the experience of transitioning from breast cancer patient to advocate on her award-winning blog Journeying Beyond Breast Cancer.