How could cancer and cancer treatment impact a woman’s fertility? Oncofertility expert Dr. Terri Woodard explains cancer’s impact on a woman’s reproductive health — and the preservation options available. Dr. Woodard discusses emerging research, explores fertility planning, and shares advice for collaborating with your healthcare team.
Dr. Terri Woodard is a reproductive endocrinologist at Texas Children’s Pavilion for Women. Dr. Woodard holds a joint appointment as an Assistant Professor in the Division of Reproductive Endocrinology and Infertility at Baylor College of Medicine and the Department of Gynecologic Oncology and Reproductive Medicine at MD Anderson Cancer Center. Learn more about Dr. Terri Woodard.
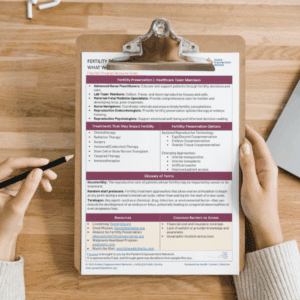
Related Resources
Transcript
Jamie Forward:
Hi, I’m Jamie Forward, your host for today’s webinar. Today we’re kicking off PEN’s new series, Flourish. Flourish is focused on helping women living with cancer to understand the impact of the disease on their reproductive health, including their fertility, hormones, and sexual well-being.
Today’s program is going to focus on fertility. So, to help us understand this complex issue, we have an expert joining us to explain how a woman’s reproductive health may be impacted. Now, before we meet our guests, here’s a few important reminders. The email you received about this webinar contains a link to a program resource guide.
If you haven’t already, click that link to follow along during the webinar. At the end of this program, you’ll receive a link to a program survey. Please take a moment to share feedback about your experience today in order to help us plan future webinars. And finally, before we get into the discussion, please remember that this program is not a substitute for seeking medical advice.
Please refer to your healthcare team about what might be best for you. Okay. Let’s meet our guest today. Joining us is Dr. Terri Woodard. Dr. Woodard, welcome. Can you please introduce yourself?
Dr. Terri Woodard:
Thank you, and it’s such a pleasure to be here. My name is Terri Woodard. I’m a professor in the Department of Gynecologic Oncology at Reproductive Medicine at MD Anderson Cancer Center.
And I also hold a joint appointment in the Division of Reproductive Endocrinology and Infertility at Baylor College of Medicine and Texas Children’s Hospital.
Jamie Forward:
Wonderful. Thank you so much for being here today. So, Dr. Woodard, you established the oncofertility program at MD Anderson Cancer Center. So, for those that aren’t familiar with this term, can you explain what oncofertility means?
Dr. Terri Woodard:
So oncofertility, this term was coined a couple of decades ago, actually, and it really refers to the reproductive care of patients whose fertility may be impacted by cancer or its treatment.
Jamie Forward:
Okay. Thank you for that explanation. So, let’s learn more about how cancer and cancer treatment can impact women. So, how is reproductive health affected? Is it the cancer, or is it the treatment, or is it both?
Dr. Terri Woodard:
It can be both.
So, one thing is that women are at risk for developing gynecologic cancers that can directly affect the reproductive organs. So, we’re talking about ovarian cancer, cervical cancer, endometrial cancer. So, all of those can directly affect fertility in itself.
So, in addition to cancer directly affecting the reproductive organs, there are other cancers where the treatment can actually impact infertility. So, we’re talking about things like chemotherapy or other systemic therapies, radiation, surgeries that can also impact reproductive function, as well.
Jamie Forward:
Okay. So, as far as, are there any sort of treatment? It sounds like also the treatments that could – or cancer-related therapies, I should say. So, therapies that are treating side effects, etc., of medicine, can that also have an impact on it?
Dr. Terri Woodard:
Absolutely, yes. And then, sometimes these modalities are combined, so it’s not uncommon to see someone who’s getting both chemotherapy as well as something like radiation.
Jamie Forward:
Okay. And what about hormonal therapies?
I know there’s these that are often used in breast cancer. How might they affect a woman’s reproductive health?
Dr. Terri Woodard:
So, the interesting thing about hormonal therapy is that they’re not directly gonadotoxic themselves. So, giving tamoxifen (Nolvadex), or an aromatase inhibitor, or a GnRH agonist doesn’t necessarily cause the ovary to fail. But usually, women have to be on these agents for five to 10 years, and they are not compatible with becoming pregnant. Actually, many of them will shut down the ovaries. The ones that don’t are actually teratogenic, meaning it can cause birth defects. So, the concern that we have with these agents is that while the woman’s on them for five to 10 years, she is aging, and with age, fertility declines.
But there are also other systemic therapies that are newer, like targeted agents, immunotherapy, where we don’t have a lot of data about fertility risks. So, making sure patients understand that. And the other thing about some of these agents is that they’re on them for long periods of time, so they may not be able to come off of them to get pregnant. So, those are all conversations that we should be having up front with patients before they start them.
Jamie Forward:
Sure. And what about like bone marrow transplant and stem cell, maybe CAR T-cell therapy, things like that? Or do those come into play as well?
Dr. Terri Woodard:
So, they do, and honestly, it’s ideal. So, usually by the time someone gets to bone marrow transplant, stem cell transplant, they were diagnosed some time ago. Usually, you don’t go straight there. So, the important thing is getting to those patients early before they get to that point.
And the fact is, their initial time of diagnosis, maybe the risk wasn’t thought to be that high, but now they’re needing more therapy. By the time we’re getting to stem cell transplant, it’s a little bit harder to offer fertility preservation services. Sometimes we can freeze ovarian tissue, but typically, these patients have recently had chemo, so egg freezing and things like that are not really that useful, or helpful, or effective. So, but I still think even if the patient didn’t have a conversation before having that conversation before a transplant, is very important because those are women that are at very, very high risk for ovarian failure and infertility.
So, not only the fertility piece, but also talking about what it means for needing hormone replacement therapy and things like that in the future.
Jamie Forward:
Sure. Okay. So, that really brings up the most, what we really should get to here is timing, right? So, with all of this, the timing of the discussion about fertility is very important.
And, of course, a cancer diagnosis can be a really overwhelming time. So, it’s really important that they advocate for themselves, which I’m sure you would corroborate that.
Dr. Terri Woodard:
Yes.
Jamie Forward:
So, should patients begin this conversation with their healthcare team, and should they start with their oncologist?
Dr. Terri Woodard:
They should start as soon as possible with any healthcare provider that they’re talking to. ASCO developed guidelines back in 2006. ASCO is the American Society for Clinical Oncology. And these guidelines basically state that as healthcare providers, all of us should be invested in making sure that patients are educated about their potential risk of infertility as a result of cancer or its treatment. So, as soon as a woman knows that she is diagnosed, it is appropriate to start asking those questions and ask for a referral to a reproductive medicine specialist.
Jamie Forward:
Okay. And so, what sort of patients should they – or excuse me, what sort of questions should women be asking their healthcare team about this like, where should they start?
Dr. Terri Woodard:
So, the first question is, will the treatment for my cancer significantly impact my fertility? Because there are treatments out there that really, we don’t worry about that should not impact fertility, at all. So, first question is risk assessment. What is my risk? The next question is, well, if I am at risk, are there any things that I can actually do to preserve my fertility? And then, the question following that really should be like, “Well, will I have enough time to do those things to preserve my fertility, and do you think it’s safe or not?”
Jamie Forward:
Sure. And what role should a partner play in this discussion?
Dr. Terri Woodard:
So, it really depends on the patient. So, I find that when talking to a lot of couples, the partner or the spouse kind of defers to the woman because, the partner’s like, “Hey, I just want them to be okay and be comfortable with everything.
I am their support system and whatever they decide, I’m okay with it.” Other couples are much more collaborative, but I think in all cases, it’s wonderful to have the partner involved just as another set of ears. This woman is newly diagnosed, there’s lots of information being thrown at her, and to have someone else hearing it is so important. And someone to kind of bounce their thoughts and ideas off of is very, very useful in decision-making.
Jamie Forward:
Yeah, it’s a really important role, and people don’t often consider it. They’re really a part of the healthcare team. So, what would you say to someone who is hesitant to speak up about family planning? It’s an overwhelming time. Sometimes they’re not even a point where they’re ready to have children, but why is it so important to say something, and speak up, and not be shy about it?
Dr. Terri Woodard:
Yeah, it’s very important because this may be your shot. And I think sometimes patients feel like, “Okay, I’m dealing with this cancer. That’s all I can deal with right now.”
Or maybe they feel like it’s inappropriate to ask their provider, like, “Oh, you know, they’re trying to save me, but yet, I’m talking about fertility.” The point is that this is all part of comprehensive cancer care. And really, we don’t want patients to lose the opportunity to potentially have a family, in the event that they become infertile because of their treatment.
Jamie Forward:
Sure. And, of course, every physician or patient-doctor relationship can be a bit different. So, if a patient’s not feeling supported by their healthcare team in that discussion, what sort of advice do you have for them? Should they consider a second opinion?
Dr. Terri Woodard:
I think it’s always wise to seek a second opinion if you’re not comfortable with who you’re seeing. And even, if I have a complex or difficult case and the patient doesn’t seem comfortable, I encourage a second opinion to get some other eyes and ears on the situation.
And then, I also want to point out that we work in healthcare teams, and we all have different roles. And I would say that a lot of times, people look at the oncologist as the busy one making diagnosis and treatment plans, but often, there are other people that are part of those teams, such as nurses or advanced practitioners. A lot of programs have navigators now. Those are people that a woman might feel more comfortable talking to to help them figure this out.
Jamie Forward:
Yeah, and I think even sending an email through the patient portal saying, “Is there somebody I can talk to?” if you’re nervous about speaking up. If that’s the way you can get it out, I say, early and often. Right?
Dr. Terri Woodard:
Yes.
Jamie Forward:
Okay, great. So, let’s talk a little bit about preserving fertility. So, now that we understand more about the issues that may occur, what are the potential approaches for fertility preservation?
Dr. Terri Woodard:
So, there are a lot of different approaches.
And some of it really depends on the type of cancer diagnosis. So, as I was talking about before, there are women that are diagnosed with gynecologic cancers, for instance. And historically, the way that we’ve treated those cancers is to remove reproductive organs, which obviously is not compatible with fertility. But over the years, we’ve learned that especially if someone has early-stage disease, we can be more conservative in our surgical methods. Or sometimes, instead of doing surgery, treat people hormonally, like in the instance of endometrial cancer, and still give that patient an opportunity to try to conceive after cancer treatment.
For other things, like if a patient is getting radiation to the pelvis, there are ways to surgically move the ovaries as well as the uterus now, up higher into the abdominal cavity, so that the radiation doesn’t have as strong as an effect.
Really, the standard of care, especially here in the United States, has been to utilize assisted reproductive technology. So, that’s referring to things like IVF, which would include embryo freezing, or the first part of it would be egg freezing. And then finally, for our young, young patients who may not have gone through puberty yet, or who may not have the time to do ART, we can sometimes offer ovarian tissue freezing.
Jamie Forward:
Okay, great. So, what is the ovarian tissue preservation? What is that exactly?
Dr. Terri Woodard:
So, essentially the idea of ovarian tissue freezing is that we can remove a portion of the ovary or an entire ovary and basically freeze it. And that tissue contains lots of immature follicles in it. Sometimes, they actually contain some mature follicles, and we can get those eggs when we remove that tissue.
But the idea is that we can freeze this tissue, and if the woman develops ovarian failure, this tissue can then be transplanted back into the body after cancer and start to work again. And there have been hundreds of births using this technique. I will say it’s not widely available in the United States. There are specialized centers who are doing this. But essentially, this tissue can work, and patients can conceive naturally or via IVF.
Jamie Forward:
Fascinating. So, related to egg freezing, as you were talking about earlier, so imagine the timing of that can potentially affect, how does that – you work that in if you’re thinking about treatment in the future? How do you go about coordinating that?
Dr. Terri Woodard:
Yeah. So, to do egg freezing or embryo freezing, you do need the services of a reproductive endocrinologist. And so, one important thing is being able to find a reproductive endocrinologist. We certainly encourage oncologists to establish those relationships so that they can quickly refer a patient for fertility preservation if need be.
But typically, it takes about two weeks for a patient to freeze her eggs or get the eggs to freeze embryos. And there have been some misconceptions on the length of time it takes and how much it might delay the start of therapy. But now, we have something called random start protocols that make this process a lot quicker than it used to be historically. Historically, we always had to wait for her to start her period. So, if she just had her period, then you’re waiting a whole other month before you can do a cycle. But these days, she can come in at whatever part of her cycle, and we can get her started right away.
Jamie Forward:
That’s great information. I was under the assumption that it would take much longer than that. So, thank you for clarifying. So, you’ve mentioned ways to protect the ovaries, egg freezing, tissue preservation.
So, how do you determine which approach is best for which patient type?
Dr. Terri Woodard:
So, all of these are going to be highly individualized. And I think that’s why it’s so important to have that initial fertility consultation because part of that consultation is going to be discussing the risk. So, if the risk is relatively low, we probably don’t want to go and remove someone’s entire ovary if chances are she’s most likely going to be okay, but she might want to freeze eggs. I think the other part of this is what aligns with the patient. So, sometimes people have ethical, or moral, or religious reasons that they might not want to do one versus the other, so sometimes that plays a role.
And, unfortunately, the other thing that often dictates what people choose to do is finances. Most of this is not covered by insurance. So, that often limits people’s choices.
Jamie Forward:
Sure. And that leads me to my next question.
So, outside of financial resources, what are other common barriers to accessing fertility preservation?
Dr. Terri Woodard:
I think one thing is just the knowledge gap, both on the side of patients as well as providers. I think as providers, we’re not always prone to talk about things that we don’t know a lot about, so we might skip over it if we don’t feel comfortable talking about it. And I think specifically, providers who aren’t taking care of young women routinely might not even think about it. And then, on the other hand, as a young cancer patient, say you’re 22 years old and in college, doing all you can not to get pregnant, and then we’re throwing this infertility thing at you, you don’t even really know or it’s not on your radar to even ask about it.
Certainly, there are other barriers in terms of geographic access, so people who live far from cities with fertility clinics. I see patients where the nearest fertility clinic may be a couple hours away.
So, that’s another barrier. And then, of course, yes, financial is probably the biggest barrier of them all.
Jamie Forward:
Sure. And are there any support organizations to help with the financial side of it? Do you know of any nonprofit, advocacy groups, for example?
Dr. Terri Woodard:
Actually, yes. So, there are several that I can think of off the top of my head. Livestrong has had a fertility assistance program for many years now. There’s also a wonderful group that works with several states throughout the United States called Chick Mission, who will pay the cost of egg freezing for women with cancer. There’s also another great resource from the Alliance for Fertility Preservation. And their main goal is actually to help pass legislation that will cover fertility preservation for patients with cancer. But they also have resources on their website that patients can utilize to try to get additional assistance.
And then finally, for medications, some of the drug companies actually offer assistance. So, Walgreens Heartbeat Program will cover a lot of the medications if there is a cancer diagnosis.
Jamie Forward:
That’s great information. Thanks for sharing those resources. I should also mention that our program partner, Worth the Wait, provides financial support and educational resources for fertility for cancer survivors. Scan the QR code on your screen to learn more.
Dr. Terri Woodard:
Yeah, Worth the Wait is awesome. And they also help with gestational carriers, post-treatment for survivors who may not have had this opportunity.
Jamie Forward:
Wonderful. That’s great to know. So, let’s talk a little bit about the emotional side. I know that you’re involved in the psychosocial aspect of fertility preservation. So, can you share a little bit about this? What are the common issues?
Dr. Terri Woodard:
So, I think the first thing is that patients are just overwhelmed.
They’re overwhelmed by the information about their cancer diagnosis. And then, you add infertility or the threat of infertility on top of it, it’s hard for people to manage. I think one thing that really struck me when I started doing this work is that sometimes patients want you to tell them what they should do. And this is really a values-based decision. So, our job is to provide information. It’s to give them context for their own decision-making and their values, but we can’t really tell them what to do. But we’ve tried to develop some ways to make it easier for them.
Occasionally, I’ll run into patients that are really distressed about this, and that’s when I will often refer them to reproductive psychologists or counselors that can help them delve into this a little deeper than what I can do in the clinic.
But I do want to stress to patients that there are resources, and this is not an easy decision to make. And sometimes you don’t even have much of a decision, you’re really sick and we have to start treatment right away. Fertility preservation might not be an option. But I think it’s important to remember that we can always circle back to this. There are so many ways to build families these days. So, you know, don’t give up.
Jamie Forward:
Sure. And can you tell us a little bit about your research in this area?
Dr. Terri Woodard:
Yes. So, because I was running into this issue of women saying, “Well, just tell me what to do,” I learned about a whole field of science called Decision Science. And what we did was develop a decision aid for women who have been newly diagnosed with cancer and who have to make these decisions. And the wonderful thing about this decision aid is that it was really designed by patients for patients. So, they told us what they wanted.
They wanted to see testimonials from other women who had to make various decisions. They wanted to know about the processes, the effectiveness rates, the cost, all of that. And in this decision made, we also embedded some values-based exercises because, like we were talking about earlier, many of these women might not have even thought about having children. So, there’s a list of questions about, what’s really important to them or what they think they might want in the future.
Jamie Forward:
Sure. And so, how can someone access this decision aid?
Dr. Terri Woodard:
So right now, we’re just working on getting it dispersed throughout MD Anderson, but we’re hoping in the next year or so, it will be available to everyone. And that was always the intent. For instance, we said that one of the big barriers might be geography. Well, in this decision aid, there’s actually a find a clinic link. So, someone can put in their ZIP code and figure out what the nearest clinic is or where it is with regard to where they live.
Jamie Forward:
Okay. And just to circle back to your oncofertility team that we were talking about earlier. So, who’s on that team? What does that healthcare team look like for a patient?
Dr. Terri Woodard:
So, my immediate team is actually pretty small. There are two of us who are reproductive endocrinologists. We also have an advanced nurse practitioner. We also have nurse navigators that work throughout the institution with different departments that refer to us or contact us when patients have questions or need some additional navigation or guidance. Of course, we have our fertility lab teams that do all the cool stuff in the back with the eggs, and the sperm, and the embryos.
And then, we have some ancillary people that we work with, for instance, our reproductive psychologists, who not all of our patients have to see, but some of them do.
And the other important people that we often will work with, and this is more post-treatment, are our maternal fetal medicine specialists. So, when a patient comes back and says, “You know what? I’ve beat cancer. I’m this many years out and I think I want to become pregnant,” I send them to maternal fetal medicine for preconceptual counseling so that we can optimize their health prior to becoming pregnant and make sure that we’re not missing anything so that both baby and mom will have a safe birth.
Jamie Forward:
That’s a really important point that you bring up to circle back after, to have a team in place for when you’re ready to have a child or plan a family. So, let’s talk a little bit about what happens if the conversation about reproductive health doesn’t take place prior to treatment. Are there steps post-treatment that patients can take?
Dr. Terri Woodard:
Yes. And when I came to MD Anderson about 13 years ago now, I guess I had a very naïve sense of what I would be doing.
I thought, “Okay, I’m going to freeze eggs. I’m going to freeze sperm. It’s fertility preservation. Fertility preservation.” But what I quickly realized is about 30 percent of the patients I see are survivors of cancer who may not have known about this opportunity or may not have been able to take advantage of the opportunity. So, the question is, what can I do now? So, we will do a thorough fertility investigation to see what their reproductive status is, and from there, develop potential treatment plans that can help them build their families.
And in some cases, patients have to kind of re-envision how they thought they would build their families because we do have a considerable number of people who are in fertile post-treatment and might need to consider third-party reproductive options such as donor eggs, donor embryos, donor sperm. So, again, that’s why I think it’s so important, even at that initial consultation.
To state that even if you can’t do anything, or you don’t have the time, you don’t have the money, or you just choose not to, we can always circle back and find some other options if they’re acceptable to you.
Jamie Forward:
Okay. And you know, we’ve really been talking about sort of women’s based GYN type cancers, ovarian, cervical, etc. But it seems like this may apply across the board for blood cancers such as leukemia and other things. This really applies to every cancer type. Would you agree with that?
Dr. Terri Woodard:
Yes, absolutely. Absolutely.
Jamie Forward:
And so, as a physician, how do you empower patients to be proactive about fertility preservation? What is your sort of – what do you sort of lead with?
Dr. Terri Woodard:
So, I really feel like the most important thing that I do as a physician is the education. When people know things, that is so empowering.
It gives so much agency. So, just letting patients know that, “Hey, this may be a risk. These are the things that you can potentially do,” is the most important thing that we, as reproductive endocrinologists, can do. And I will say that the angriest patients that I see are the ones that come and say, “No one told me that this could happen to me,” and “I didn’t get the chance or the opportunity.” So, honestly, the baby pictures on my wall, I love them because they’re awesome. But in terms of, I think the most important work, it is the education.
Jamie Forward:
Okay. That’s great advice. So, Dr. Woodward, as we close out this program, what would you like to leave the audience with? Are you hopeful about the future of fertility for cancer survivors?
Dr. Terri Woodard:
I am hopeful. So many really cool things are happening in the world of reproductive medicine.
I alluded to it earlier, but now people are doing uterine transposition, so actually moving the uterus out of the pelvic cavity. People are doing uterine transplants, which have not been done in women with cancer yet, but it’s probably on the horizon. People are developing artificial ovaries. So, I think there’s going to be a lot of other options that are available to women in the future that are not available now. And I’m also hopeful that access will improve, as well.
I’ve been involved with the Alliance for Fertility Preservation. They helped us get some legislation passed in the state of Texas that provides some coverage for patients with cancer. But every year, when I look at their map of who’s developed legislation to provide access to patients, it gets larger. So, I’m hopeful that eventually we’ll get to a point where every person who wants fertility preservation can get it and that the finances aren’t the issue.
Jamie Forward:
That’s a very hopeful outlook, Dr. Woodard. Thank you so much for joining us today.
Dr. Terri Woodard:
Of course, it’s my pleasure.
Jamie Forward:
And thank you to all of our collaborators. If you’d like to watch this webinar again, there will be a replay available soon. You’ll receive an email when it’s ready. And don’t forget to take the survey immediately following this webinar. It will help us as we plan future programs.
To learn more about cancer and fertility, and to access tools to help you become a proactive patient, visit powerfulpatients.org. I’m Jamie Forward. Thanks for joining us.