Understanding Common Clinical Trial Terminology
Katherine Banwell:
Dr. Funchain, are there common clinical trial terms that patients should know?
Dr. Pauline Funchain:
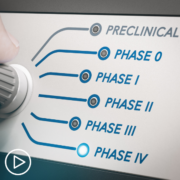
Yeah, there are trial terms that people hear all the time, and probably should know a little bit about. But I think the most common thing people will hear with trials are the type of trial it is, so Phase I, Phase II, Phase III. The important things to know about that are essentially, Phase I is it’s a brand-new drug, and all we’re trying to do is look for toxicity. Although we’ll always on the side be looking for efficacy for whether that drug actually works, we’re really looking to see if the drug is safe.
A Phase II trial is a trial where we’re starting to look at efficacy to some degree, and we are still looking at toxicity. And then in Phase III is, we totally understand the toxicity, and we are seeing promise, and what we really want to do is see if this should become a new standard. So, that would be the Phase I, II, and III.
Another couple of terms that people hear a lot about are eligibility criteria, or inclusion criteria. So, those are usually some set of 10 to 30 things that people can and can’t be. So, usually trials only allow certain types of cancer, and so that would be an inclusion criteria, but it will exclude other types of cancers. Most trials, unfortunately, exclude pregnant women. That would be an exclusion criteria.
So, these are things that, at the very beginning of a trial, will allow someone to enter, or say, “You’re not in the safe category, we should not put you on a trial.” Many trials are randomized, so people will hear this a lot. Randomization.
So, a lot of times, there is already a standard of care. When there’s already a standard of care, and you want to see if this drug is at least the same or better, then on that trial, there will be two different arms; a standard of care arm and experimental arm.
And then in order to be fair, a randomized trial is a flip of a coin. Based on a electronic flip of a coin – nobody gets to choose; not the doc, not the patient. On that type of trial, you’ll either get what you would normally get, standard of care, or something new. So, that’s a randomized trial. Not all trials are randomized, but some are. And those are the things that people will run into often.