What Are Common Head and Neck Cancer Symptoms and Treatment Side Effects?
What Are Common Head and Neck Cancer Symptoms and Treatment Side Effects? from Patient Empowerment Network on Vimeo.
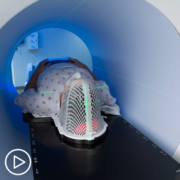
What symptoms and side effects can head and neck cancer patients experience? Expert Dr. Ari Rosenberg discusses common symptoms and treatment side effects and explains why it’s important to share your symptoms and side effects with your doctor.
Dr. Ari Rosenberg is a medical oncologist and Assistant Professor of Medicine at the University of Chicago Medicine. Learn more about Dr. Rosenberg.
See More From The Pro-Active Head and Neck Cancer Patient Toolkit
Related Programs:

|

What Factors Impact Head and Neck Cancer Treatment Decisions? |

Expert Advice for Newly Diagnosed Head and Neck Cancer Patients |
Transcript:
Katherine:
What about symptoms and side effects? What should people be worried about?
Dr. Rosenberg:
Yeah. So, oftentimes when patients come to us with a new diagnosis of head and neck cancer, when looking back, they’ve had, sometimes, symptoms for a while, whether it’s a nagging ulcer on their tongue, or some difficulty with speech, or a new hoarseness, or a lump in the neck that turns out to be a cancerous lymph node.
And so, even before we get into the diagnosis of head and neck cancer, I do think it’s important for people to know that, in particular, if some of these symptoms – particularly if they’re lasting for a while and not going away with more conservative measures like antibiotics – really need to be evaluated by an ENT and a doctor team to make the diagnosis of head and neck cancer, so it can be treated.
The side effects of treatment very much depend on the treatment modality that’s used. So, for example, when chemotherapy and radiation, and chemoradiation is utilized, oftentimes, the treatment itself could be associated with a lot of side effects from treatment. Things like a sore throat, things like skin changes, things like fatigue, challenges with nutrition, and a plethora of other things that, depending on some of the specifics, can be associated. Which is one of the reasons why we’re trying to figure out if there are some patients that we can deintensify the radiation, or do more precise radiation, rather than standard, regular dose radiation for everyone. But that’s of course in the context of some of the clinical trials that are being evaluated for improving outcomes for head and neck cancer patients.