What Are the Beginning Stages of Multiple Myeloma (MM)?
What Are the Beginning Stages of Multiple Myeloma (MM)? from Patient Empowerment Network on Vimeo.
What happens in early stages of multiple myeloma? Watch as early multiple myeloma is explained as expert Dr. Rafael Fonseca details what occurs in the body, and patient Lisa Hatfield shares the symptoms that she experienced early in her myeloma journey.
See More from START HERE Myeloma
Related Resources:

|

|
|
Transcript:
Dr. Rafael Fonseca:
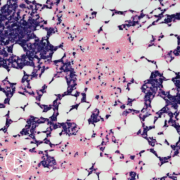
These cells live predominantly inside the bones in the space we call the bone marrow. They can do a number of things that actually lead to the symptoms and to the clinical presentation. As they grow in the bone marrow, they take some of that real estate. A person may experience fatigue and that is because they have anemia. The myeloma cells are also very characteristic because they can erode into the structure of bones, so destruction of bone is another feature that we see in patients with myeloma. That can be either seen on X-rays or sometimes people will present with symptoms related to bone pain or discomfort with movement or weight bearing. Those are signs that we look for.
Lisa Hatfield:
For me, early on with myeloma, I really had none of the classic symptoms. All of my blood work was coming back normal. I would see my regular primary care physician every two years. My lab work was coming back normal. Nothing really stood out. I wasn’t anemic. My kidney function was okay. What did stand out over the course of two years was I was experiencing progressively worsening pain in my hip. It felt like kind of a pinched kink pain in my hip to the point where it progressed to the point where I could barely walk was when I finally talked to my primary care doctor. And requested very strongly to have a scan done, and that’s when I was diagnosed with myeloma.
So the primary reason I went in was for the pain to begin with, and my doctor did look at the pain. He tried to assess it several times over the course of two years. But it wasn’t until I had the MRI that showed a large plasmacytoma on my spine when I realized that something was wrong. A couple other signs that I did have looking back now that I complained about to my doctor and I thought were rather curious, I shrunk a little bit. I shrunk in height. My daughters were laughing, and they’re like “Mom, we’re just growing.” But I did shrink in height by about 2-1/2 inches from the compression fractures in my spine and the plasmacytoma that had eaten away at my spine. And then another thing that a lot of people don’t talk about is sometimes people will have foamy urine. We don’t like to talk about body functions.
But it’s important to know that if you experience that, there are proteins that they can find that are called Bence Jones proteins that are a sign of multiple myeloma. So if you notice anything unique like that – foamy urine, extreme fatigue, anemia in your blood tests, it’s definitely worth asking your doctor about. And also relentless, persistent pain in your hips, in your back, in your ribs, any of those areas, it’s worth talking to your doctor about just to assess those thoroughly to make sure there’s not something more significant going on.
If myeloma goes undiagnosed and untreated, the cancer cells can make a patient experience:
- Lowered immune function due to white cells being crowded out, resulting in frequent infections
- High levels of protein in the urine and blood, which may cause kidney damage
- Build-up of cancer cells in the bones, which can cause bone weakening, bone pain, and bone fractures









