How Does An Empowered Patient Approach Care Coordination? #patientchat Highlights
Last week, we hosted an Empowered #patientchat on leveraging social media for patient advocacy. The #patientchat community came together for an engaging discussion and shared their best advice and tips.
Top Tweets and Advice
Care Coordination Means Everyone Is Working Together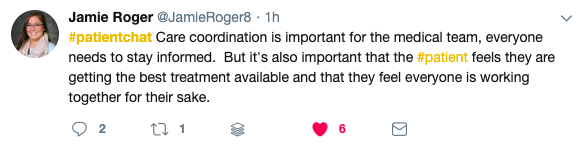
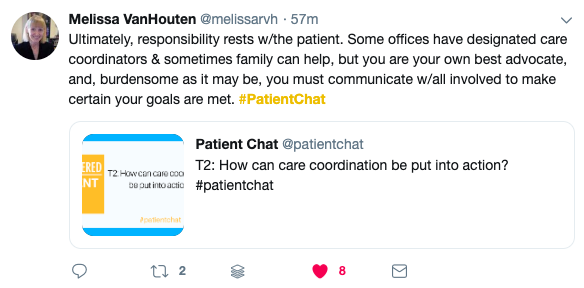
You Are Your Own Best Advocate
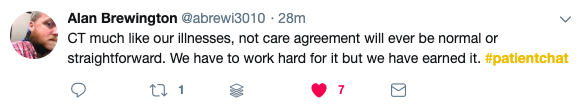
Work For What You Deserve