What Is Minimal Residual Testing in Multiple Myeloma?
What is Minimal Residual Testing in Multiple Myeloma? from Patient Empowerment Network on Vimeo.
How is minimal residual testing (MRD) used for multiple myeloma patients? Watch as expert Dr. Nina Shah explains the use of MRD testing, and myeloma patient and Empowerment Lead Lisa Hatfield shares her knowledge of MRD testing and how specialists use it in treatment and care.
See More from START HERE Myeloma
Related Resources:

|

|

|
Transcript:
Dr. Nina Shah:
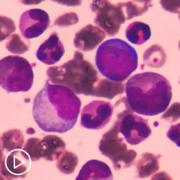
Minimal residual disease is exactly what it sounds like. It’s the disease that you can’t see under the microscope, but it’s still there. And I sort of equate it to the little deep food particles that are in a pot after you clean it and really, really scrub it, but still, something is in there. And that’s what it is for myeloma.
Minimal residual disease testing, or MRD testing, is performed to locate any small number of cancer cells that remain in the cancer patient’s bone marrow during or following treatment. The presence of any remaining cancer cells is the most common cause of relapse in blood cancers, so MRD testing is used to gauge treatment success, to compare different treatments, to detect myeloma recurrence, to monitor patient remission, and to help choose optimal treatments.
Lisa Hatfield:
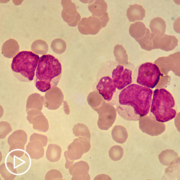
So when I was first diagnosed, MRD testing, or minimal residual disease testing, sometimes called measurable residual disease testing, was just, they were looking at having it approved by the FDA for clinical trials only. Still it was only approved for clinical trials as an end point. However, a lot of myeloma specialists are using this MRD testing to help guide decisions. It’s not approved for that yet but to help guide decisions for patients who have a really great response to their induction chemo and stem cell transplant that they may have after induction chemo and after some years of maintenance to see if they can possibly go off of their maintenance therapy. It is occasionally being used, MRD testing, is being used to help guide providers and patients on where to go with treatment. So MRD testing requires a bone marrow biopsy. The most sensitive MRD testing is called clonoSEQ testing, it is NGS testing. It does require the original bone marrow sample, and then they can track that over time each year or however often you have bone marrow biopsies to see if the cloned cells are still there.
So MRD testing right now requires the bone marrow biopsy. I’m hoping that someday it can be done with a blood test, but it’s really important for tracking purposes to see if you’re responding to therapy, to see if you’re staying in remission during maintenance therapy. And it’s even worthwhile too if you’re having toxicities from maintenance therapy to consider going off of that therapy. You can test to see, right now the MRD testing is testing to see if they can find one myeloma cell out of one million cells. So it’s called 10-6 MRD testing. That’s the most sensitive test that’s out there to date and really important if you’re considering possibly going off of maintenance therapy or are having significant toxicities during your treatment.