How Can You Access the Latest CLL Treatment Options? from Patient Empowerment Network on Vimeo.
Could a new or emerging chronic lymphocytic leukemia (CLL) treatment be right for you? In this 30-minute webinar, Dr. Anthony Mato will review current and emerging CLL treatment approaches, important decision-making considerations, and the ins and outs of clinical trials.
See More From The Pro-Active CLL Patient Toolkit
Download Program Resource Guide
Related Resources
Transcript:
Katherine:
Hello, and welcome to the webinar. I’m Katherine Banwell, your host for today’s program.
Today we’re going to explore promising CLL research and what I could mean for you. Joining me is Dr. Anthony Mato. Welcome, Dr. Mato.
Would you please introduce yourselves?
Dr. Mato:
Hi, I’m Anthony Mato, Director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Katherine:
Great. Before we get into the discussion, please remember that this program is not a substitute for seeking medical advice. Please refer to your healthcare team. Well, Dr. Mato, when it comes to CLL treatment there seems to be an abundance of new and developing options which, of course, is a great problem to have. To help patients understand more about the types of treatment currently available, let’s review the treatment classes and discuss how they work to fight CLL.
Well, and let’s start with chemo. Some patients are probably familiar with the term FCR. What does that stand for, and how does work?
Dr. Mato:
Sure. FCR is a name for three chemotherapies that are combined together.
So, this is fludarabine, cyclophosphamide which are two cytotoxic chemotherapies combined with the monoclonal anti-CD20 antibody rituximab, so two traditional chemos plus an immunotherapy called rituximab that have worked together synergistically and have been quite effective over a prolonged people of time for treating patients with CLL. FCR was originally developed at MD Anderson.
But a very important CLL trial called CLL8 confirmed that FC plus rituximab was better than FC by itself, so a trial that demonstrated improvement in progression-free survival but also in overall survival advantage. And so, this became the standard of care more than a decade, and it has been a very common chemotherapy combination for patients.
Katherine:
What about monoclonal antibodies? How do these treat CLL?
Dr. Mato:
Great question. So, right now, we have several monoclonal antibodies that are approved in CLL.
They all target the same cell surface marker called CD20. And so, the way antibodies work in general in these patients, in our patients is that we identify a cell surface marker. In this case, it’s the protein CD20, and these antibodies are able to target that specific cell surface marker, bind to it, and in a way act as a flag for the immune system to destroy these cells.
So, an antibody like rituximab may be able to destroy a cell directly, or it may flag the cell to be destroyed within the immune system within the spleen, for example. So, different mechanisms of action but it’s a targeted therapy because it focuses on a specific protein that’s largely expressed on the cancer cells relative to other cells within the body.
Katherine:
There are also a variety of inhibitor treatments. What are they, and what exactly are they inhibiting?
Dr. Mato:
Yeah, so the kinase inhibitors are probably some of the most important drugs developed for CLL to date.
And we have different classes. One group would be BTK inhibitors which stands for Bruton tyrosine kinase, another would be PI3K inhibitors. Another class would be a BCL-2 inhibitor which is a little bit different. Essentially, the way to think about inhibitors are that they identify key molecules within a cell that are very important for either cell survival or cell signaling. These are the molecules that tell cells to either migrate or to hone in on a particular area or to amplify signaling to allow them to survive.
So, a drug like ibrutinib or acalabrutinib which are BTK inhibitors block this BTK signal and interrupts a very important survival signal in the cell, kinda causes it to go haywire in many ways, and then allows those cells to slowly die over time. PI3K inhibitors like idelalisib or duvelisib do the same. They block a very important and parallel signaling pathway to BTK that cause a very similar effect.
And then venetoclax which is a BCL-2 inhibitor works a little bit differently. So, CLL cells are very primed to actually die except that there are signals in place that block that process called apoptosis, and so venetoclax blocks the blocker of that signal, sort of inhibits the inhibitor to cell death and allows that natural process of cell death to occur in CLL cells.
And so, they’re kinda targeting different pathways, but they’re able to stop the cell in a way. This is very different than cytotoxic chemotherapy like the FC which targets all dividing cells. Here we’re targeting cells where those particular enzymes are most important.
Katherine:
Do inhibitors need to be taken indefinitely?
Dr. Mato:
That’s a great question, and that’s something that we’re still working out. Right now, BTK inhibitors and PI3K inhibitors are all given as continuous therapies. That’s not to say that they couldn’t be stopped, but they haven’t been studied in a way that allows us to stop them. So, there’s not a lot of evidence to support that.
BCL-2 inhibitors, venetoclax, were studied as either as continuous therapies or as what we call a time-limited therapy, either 12 months in the frontline or 24 months in the relapsed/refractory setting. And so, they can be given for a fixed-duration period and then stopped.
Katherine:
Are there combination approaches that are effective?
Dr. Mato:
Depends on what you mean as a combination, so right now, BTK inhibitors, ibrutinib, for example, is approved either to be given by itself or with CD20 antibodies, either rituximab or obinutuzumab, another antibody that’s like rituximab in the frontline setting. So, that is a combination of drug plus antibody.
Acalabrutinib is either approved to be given by itself or with the CD20 antibody obinutuzumab. In either case, whether the antibody is present or not, the drug is given continuously. Venetoclax is given either by itself or with a CD20 antibody either obinutuzumab in the frontline setting or rituximab in the relapsed/refractory setting.
There are no approved combinations of kinase inhibitor and kinase inhibitor together or inhibitor/inhibitor. So, there are studies that are exciting about ibrutinib plus venetoclax for example, but there is no one who should be receiving those combinations as a standard of care at this time.
Katherine:
Are there any other approaches that we haven’t discussed?
Dr. Mato:
Yeah, well, there are other exciting approaches from the spectrum of very experimental to closer-to-market for patients. So, there are other PI3K inhibitors that are in development which may or may not have better toxicity profiles from the current ones. There are noncovalent BTK inhibitors. These are drugs that work like ibrutinib or acalabrutinib, but they may actually overcome resistance to those molecules. So, you’re on ibrutinib; you’re progressing. You develop a resistance mutation. There are drugs that are being studied that might be able to overcome that and recapture the response.
And then there are drugs like CAR-T cells or cellular therapies, using your immune system, actually, genetically engineering your own immune system outside the body to be focused on killing CLL and then putting it back inside the body through a transfusion to allow it to fight cancer more effectively. So, those are some of the more up-and-coming strategies that are closer to being available for patients at this time.
Katherine:
All right, and we’ll discuss more about that later on. So, with all of these options, how do you then decide which class might be right for an individual patient?
Dr. Mato:
Well, you think about the patient. You think about their medical history, their comorbidities, their preferences, and then you try to focus on their disease biology, their genetic factors, their molecular factors, and also what therapies they’ve had. So, if I had a patient who had ibrutinib previously, I’m not going to give them acalabrutinib if they were resistant, for example. So, it’s not just one thing. It’s multiple things that have to be taken into account in order to make a decision.
And of course, for me as an oncologist, the hardest part is that there have not been many trials comparing the newest therapies to one another. So, I can’t tell you what’s better ibrutinib or acalabrutinib by a head-to-head comparison. I can’t tell you whether you should start with ibrutinib before venetoclax or venetoclax before ibrutinib not because we’re not very interested in having those studies performed. But they have not been performed at this point in time.
The only thing I can tell you based on prospective data from a head-to-head comparison is that we do have direct data comparing acalabrutinib which is a BTK inhibitor to idelalisib in the relapsed/refractory setting. And by all measures, acalabrutinib was better tolerated and more effective. So, we have some very early head-to-head data but not as much as we need in order to make these decisions for patients.
Katherine:
How are side effects taken into consideration?
Dr. Mato:
Well, all of these drugs although they are targeted, and they’re oral, and they’re relatively easy compared to chemotherapy are not without side effects. And so, each of these classes have their own unique side effects. BTK inhibitors can be associated with increased bleeding risk or atrial fibrillation or infection. PI3K inhibitors can be associated with lung or liver or colon damage. BCL-2 inhibitors might be associated with lowering of the blood counts and infection risk or something called tumor lysis syndrome.
So, we try to, if you had a side effect to one, not pick a drug with the exact same side effect profile, for example. And we also think about medical history for patients. So, if I had a patient who was on blood thinners and has poorly-controlled atrial arrhythmia like AFib, I might not start them on a BTK inhibitor. If I patient who has active Crohn’s disease or ulcerative colitis that’s poorly controlled, I might not start them on a PI3K inhibitor. And if I have a patient who’s near dialysis because of chronic kidney disease, and I’m worried about further tumor lysis syndrome, I might not start them on a BCL-2 inhibitor.
So, you kinda weigh a patient’s medical history, their prior therapies, and their response and toxicities, and then make a decision on what’s the best fit for patients.
Katherine:
Well, what kind of testing is involved to make sure you have the best approach?
Dr. Mato:
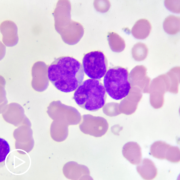
Well, there’s several tests that we think about using or we do use, and they’re mostly genetic and prognostic tests. And so, what we like to do is look at the CLL cells beyond looking at them under a microscope to try to identify the genetic markers that drive the biology of CLL. So, for example, if I have a patient who has deletion 17p which is one of the more feared chromosome abnormalities, I know right off the bat chemotherapy’s not a good fit for that patient. But I can do quite well with a BTK inhibitor like ibrutinib.
So, we’re starting to use the molecular features of the disease in order to pick therapies that are the best fit for patients. So, we have a board panel at our center that we use. At this point, some of the information isn’t helpful yet.
But some of the information is quite helpful in to make a decision about the best therapy for patients. So, this is truly what we call targeted therapies for individual patients or personalized or individualized approaches based on the disease itself.
Katherine:
Dr. Mato, we have some questions from the audience. Let’s start with this one. How high does the white blood count have to be in order to start treatment, and which are the best treatments available at this time?
Dr. Mato:
That’s a great question, and it’s a common question we hear in the clinic. So, there is no white blood cell count that defines the need to start therapy. Some patients are treated with relatively low white blood cell count. Some are treated with very high white blood cell counts.
What defines the need for treatment or therapy for CLL are the symptoms of the disease, extreme fatigue, soaking night sweats, fevers that are unexplained by infection, the need for transfusion, bleeding, bruising, growing lymph nodes, growing spleen causing symptoms, frequent infections.
Those are the things that define the need for therapy. A rising white blood cell count by itself or a cutoff at some arbitrary number should never be a reason to start treatment without some of those other factors.
Katherine:
Here’s another question for you. How do you monitor to see if a treatment is working, and what if the patient doesn’t respond to any of the treatments?
Dr. Mato:
Yeah, so, we response criteria, and so, they’re largely very simple measures. We perform a physical examination before and after treatment to see if the lymph nodes and spleen are decreasing in size. We measure the white blood cell count to verify that it’s going down. We look for normal parameters of normal functioning bone marrow like improvement in the hemoglobin or the platelet count.
So, those are some of the measures we use, and we put them together. And of course, just asking a patient how do they feel, do they feel better, are the symptoms that were associated with the CLL improving, and if the answer is yes, that would be considered responding disease. We also sometimes do measures like CAT scans to measure internal masses or internal lymph nodes and a bone marrow biopsy to verify that all the CLL cells are gone.
So, that’s the basics of a response assessment, and we also venture now into a new territory called MRD or minimal residual disease where we’ll be able to look beyond the traditional response assessment. Sometimes, it measures at a measurement of one in a million cells to verify that there’s no evidence of CLL present. If a therapy’s not working, fortunately – well, first I’ll say that with the modern therapies that we’ve already mentioned, response rates exceeded 90%.
So, it very, very infrequent that we have a patient where we pick the appropriate therapy where it doesn’t work for them. But if one is not working, then we do have measurements of resistance, and we can try to tell why a therapy maybe not working and switch them to an alternate class. And oftentimes, that will solve the problem.
Katherine:
Dr. Mato, you mentioned the term MRD. What does that mean?
Dr. Mato:
It stands for minimal residual disease. That’s using technology like flow cytometry or PCR or sequencing to take a deep look in the bone marrow and the blood for the presence or absence of CLL.
So, when I perform a bone marrow biopsy, a pathologist with their eyes might count one hundred cells. With MRD testing we could look at 10,000 or 100,000 or 1,000,000 cells to see if there’s any CLL present, much more than the human eye or the human brain could process.
Katherine:
Well, this leads us to our next topic, Dr. Mato, and that is emerging treatments for CLL. For people who don’t understand how treatment approvals work, which would you give us an overview of the stages of clinical trials?
Dr. Mato:
Sure. I’m very involved in clinical trials at my center. There are different phases of clinical trials. And so, the way that I think about them would be – let’s focus on phase one thru three because those are probably the most relevant ones for patients. The purpose of a Phase One trial is really to define the dose of the drug and confirm that it’s safe or not. We get very, very preliminary data about activity of the drug, but the major question that’s being asked is, “Is this drug safe?”
Phase Two is – and I should also add that Phase One trials are relatively small. So, it’s a small number of patients where we’re trying to find the right dose. By the time we get to Phase Two, we know the drug is likely safe. We have a lot of information about its side effect profile. We might have a hint that it’s active. And so, the purpose of a Phase Two trial is to expand the size of the trial, have more patients recruited, get more information about safety but then get more information about activity.
Of course, there’s no comparator generally in a Phase Two trial. So, it’s not like I’m asking this drug versus another drug. And the end of a Phase Two trial, we know the drug is active, we know it’s safe. And if it appears to be active, we’re feeling confident that it may be better than a standard of care which leads to Phase Three where the drug is compared directly in oftentimes what we call a randomized study to a standard of care.
So, the trial that I mentioned earlier, FCR versus FC would be a great example of a randomized, controlled trial where a new therapy would, in that case, the FCR, was compared to the old therapy, the FC.
In the more modern era, there have been several trials. I example I might mention is the RESONATE trial where ibrutinib was compared head-to-head to an antibody called ofatumumab. Patients who were enrolled were either randomized by a coin flip through a computer to one arm or the other. And then those arms are compared directly to help define a standard of care.
So, that’s kinda the basics of clinical trials, and at our center and many centers around the country, we participate in Phase One, Two, and Three trials trying to ask different questions that are important to our patients.
Katherine:
Well, speaking of patients, they’re very often fearful of participating in a clinical trial. What do you say to them to make them feel more comfortable with the idea?
Dr. Mato:
I mean, I think the most important thing to highlight is all of the standards of care that we’re using today, ibrutinib, acalabrutinib, idelalisib, duvelisib, venetoclax, these were all just drugs a few years ago that were studied in the context of clinical trials.
And so, our current standards of care are very new on the scene from clinical research. It’s very important to have a conversation with your doctor about the intent of a particular clinical trial. I think most patients are fearful of placebos or blinding where they don’t know what they’re getting, or it’s possible that they’re not getting any treatment at all.
In oncology and particularly CLL, the chances of a clinical trial having a placebo or blinding are very low. We very rarely ever participate in such studies. And so, that should provide reassurance to the patient that they know what they’re getting, they know their dose, their oncologist knows what they’re getting, and oftentimes, many clinical trials have mechanisms called crossover built into them. Meaning, that if you’re getting A versus B, and you get B, and it doesn’t work, you often have opportunity to crossover to A.
Clinical trials in CLL are the reason why there’s been so much innovation over the last several years, the reason why we can talk about six and seven approvals of drugs within half a decade.
And many of the drugs that we have at our centers will likely become standard of care in the near future. So, it gives us access to important drugs a little bit in advance of when they might be available for patients through FDA approval. So, it a lot of hope; it’s a lot of innovation. And the major message I would say to patients is don’t think of a clinical trial is for when all options have run out, but oftentimes there are great trial options that are aiming to improve the current standard of care in the frontline and also the relapsed/refractory settings.
Katherine:
What’s involved in patient participation in clinical trials?
Dr. Mato:
Well, the process is called informed consent, and so, if you’re interested in a clinical trial, you have a conversation with your oncologist to review the study, the schedule, the screening procedures. If you’re interested, you sign an informed consent and then begin a process of doing some testing, oftentimes scan, blood work, EKGs, bone marrow biopsy, to try to identify whether or not you’re a good candidate for the study.
Clinical trials are often more rigid than standard of care meaning you have to follow a strict schedule. You have to report everything, side effects, or successes related to the clinical trial. And oftentimes, a clinical trial is performed at the particular center that you signed the consent. And so, if you came to our center at MSK, odds are you would have to have treatment at our center in order to participate in that trial.
Once you’re enrolled on the trial, you’re on a strict schedule. You work with the physician and a research team, often a nurse directly who specializes in clinical trials to help ensure that you’re monitored appropriately and that the trial is successful for the patient.
Katherine:
Now that we understand how trials work, let’s get into developing research. Let’s get into developing research and what it can mean for patients. What new approaches are showing promise?
Dr. Mato:
Wow, that’s a loaded question because there’s so many possible answers. There are new versions of the current standards of care, different classes like BTK inhibitors or PI3K inhibitors which have the potential to be very active but better tolerated
So, that’s one big group of new agents in development. There are several agents in development that appear to be effective in the setting of resistance to the current standards of care. There are classes of immunotherapies that allow us in different ways to use the immune system of the patient to fight cancer directly, so not necessarily targeting the cancer cell but targeting the immune system to make it do its job to filter out the cancer.
There are new antibodies in development. And that’s just a little slice of what’s in development for CLL and new combinations of course of the current standards of care which when put together could be even more effective. So, –
Katherine:
What about – oh, go –
Dr. Mato:
Sorry. I was just gonna add that so many different possibilities available that not every center can participate in all of these types of research, but it’s amazing for patients to know how many different new options are in development that maybe even better than the current approaches.
Katherine:
Right. What kind of side effects might be involved with the emerging treatments? What might people expect?
Dr. Mato:
That’s a hard question to answer because the purpose of the clinical research is to help define the side effects associated with these newer drugs. And so, while we have a hint from early data or from Phase One data what a side effect profile might look like for a new drug, part of the consenting process is to help gather information not only about a drug’s activity but also about its side effect profile.
So, when we consent a patient, there is a little bit of an unknown about side effects, and we have sometimes very limited information that we can share about the activity. So, it’s not easy to just group these together and say these are the newest side effects to worry about. That’s really the purpose of the studies that I’m mentioning and the general idea of clinical research.
Katherine:
And that makes sense. How is research into the genetics of CLL providing a better understanding of how a patient’s individual disease may behave?
Dr. Mato:
Well, just a few years ago, the basic genetic studies for CLL included just a few chromosomal markers that we could easily or sometimes not so easily test. At our center for example, and it’s not unique, we’ll be able to look at the over 400 different mutations associated with hematologic malignancies. The more information we get, the more we realize that although under the microscope a CLL cell may look like another CLL cell, biologically, they’re very different.
They’re driven by different genetic mutations, and knowledge of those pathways that are important for an individual CLL will oftentimes, will hopefully in the future guide how therapy is selected for patients.
Katherine:
It sounds like there is a lot of very interesting research going on as more is being learned from the molecular – as more is being learned from molecular or genetic testing in CLL. And that leads us to our next topic. Why is it important to stay informed as new treatments become available?
Dr. Mato:
Well, the field is moving at such a rapid, and I would say up until very recently, every six to eight months we’ve had a new drug approved for CLL for a long period of time. So, it’s important to stay informed because in a good way, the standard of care and the pace of research is very quick and that maybe not all oncologists are as up-to-date about what’s going on in the field.
And so, through patient organizations and through webinars like this and through working closely with patient and professional societies and also with CLL experts, it’s very important to stay up-to-date not only about new therapies but about prognostic markers and about emerging clinical trials which be a benefit to an individual patient.
Katherine:
What are some of the credible sources that can help patients stay informed and up-to-date?
Dr. Mato:
I think there are several societies which I just kind of at the top of my mind I can think of which there’s credible information.
I hate to create and list and say it’s exhaustive because I’m sure I’m forgetting somebody, but Lymphoma Research Foundation has great information, Leukemia & Lymphoma Society, the CLL Society, Patient Power, there’re just many organizations that are patient-focused that have educational materials, support groups, webinars, access to CLL experts, and interviews available that are very useful, and there are several that I’m omitting.
Katherine:
That’s fine. We’ll go into that with our slides probably.
Dr. Mato:
Not intentionally by the way, just because I can’t remember every single organization, but there’s a lot of resources available for patients. I guess the one thing I would advise against is getting too mired into chat rooms or conversations that are a little bit unfiltered because it’s very hard to translate one patient’s experience to another. And I think sometimes that a chat room without a moderator or a patient support group that doesn’t have a filter in it somehow to try to understand where the questions are or concerns are coming from can sometimes lead to a lot of anxiety for patients.
Katherine:
Yeah. That’s really good advice. If a patient’s physician doesn’t seem really knowledgeable about research and the latest treatments, do you recommend a patient consider a second opinion or even ultimately consult a specialist?
Dr. Mato:
Yeah, I think even for my own patients as a CLL expert, I never discourage a second opinion. There’s always something that can be learned for the patient and the physician from that experience. Anybody who has a physician who is very resistant to allow them to get a second opinion, I think that that’s probably a tell-tale sign that they’re not the best fit for the patient.
So, I don’t like to say that every patient has to have a CLL expert. But if a patient has questions that aren’t being answered, they certainly should seek advice. There are many community oncologists who are wonderful doctors. They’re very caring. They’re very good at taking care of patients. And a CLL expert is not always needed. But if you do have a community oncologist, and they come to see me for example, we work very happily with the local doctor to partner together.
And I view it as the need – I view it as a partnership where we can work with the doctor, and it doesn’t have to be a choice. And so, if a patient ever feels they’re put in a situation where they have to choose one doctor over another, there’s probably too many egos involved, and they should think long and hard about finding new help.
Katherine:
Yeah. Let’s take one last audience question, Dr. Mato. I am IGHV mutated, young, and healthy, and I wanna participate in a clinical trial. How do I find one that’s right for me?
Dr. Mato:
That’s a great question. So, IGHV mutational status is a prognostic factor that largely defines prognosis in the setting in the need for chemotherapy. So, IGHV mutated patients typically do better when they receive chemotherapy versus IGHV unmutated patients. In the modern area where we’re talking about BTK inhibitors and some of the other drugs, for example, the outcomes are quite similar whether you’re mutated or unmutated.
I think the search for a clinical trial probably should not be based on the IGHV mutational status, but the fact that you’re a young patient and you’re looking for a clinical trial that may have a little bit of a different focus intent in terms of depth of remission or ability to stop therapy rather than just a specific focus on the IGHV status driving that decision.
What I would advise for a young person is that it’s probably very reasonable to be seen in a major academic center where there are more patients who are younger and therefore clinical trials which may have a focus on a younger patient population. And in the world of CLL where the average age is 70 or 71 at diagnosis, younger maybe 60 or 65 or 55. I’m not necessarily talking about a 25-year-old when I say younger. I don’t know this particular patient’s age.
Katherine:
Right. I’m not sure either. Many of these newer therapies are pills or oral therapies.
How do you ensure that the patient is taking the medicine as prescribed, and with COVID now in our lives on a daily basis, how has this been affected by COVID?
Dr. Mato:
So, how do we ensure patients are taking their medicines? That’s a good question. It’s not an exact science. So, part of it is we rely on the patient to tell us that they’re taking the medications. We can guestimate that they’re taking patients based on their requests for refills. So, if we give a 30-day supply and they request a refill in 60 days, they’re probably not taking it appropriately.
Sometimes, patient diaries are used. We have a whole team who sees our patients including a nurse, a nurse practitioner, a clinical pharmacist who can help gauge whether or not a patient is adherent to a schedule. And then if you’re on a clinical trial, then you often have to keep a pill diary, and a research nurse will do drug accountability assessments with patients when they’re seen in the office, so lots of different ways to answer the same question.
Has COVID affected things? A little bit during the height of the pandemic in the New York area. There might’ve been some slight delays to starting CLL-based therapy because of concerns for risk of infection, sort of risk/benefit. Currently, based on my region at least, we are treating patients. We’re not withholding therapy or delaying therapy based on the theoretical risk for COVID infection, but we’re making decisions that we think are in the best interest of the patients based on their CLL and their need for therapy.
That may be different in other areas of the country right now. We always have to weigh the risk/benefit of infection and other circumstances versus the need for CLL-directed therapy.
Katherine:
Before we close, Dr. Mato, how do you feel about the future of CLL treatment? Are you hopeful?
Dr. Mato:
I’m extremely hopeful and optimistic. I think for me, I trained as an oncologist with the hope of being able to take care of patients with CLL.
I always liked taking care of patients with CLL. It’s a passion to provide great care to help provide development or to participate in research that changes the standard of care, and every day I’m amazed with some of the molecules we work with and how much or how they’ll be able to help patients in the future and of course, taking care of patients and seeing this is in the clinic is really the best and most gratifying experience for anybody who’s involved in CLL research to see our patients who are very sick become well and go back to work or resume their normal life is really the most rewarding part of being part of the specialty.
Katherine:
Dr. Mato, thank you so much for taking the time to join us today.
Dr. Mato:
Thank you for having me, and I’m really, really thankful for participating in this program.
Katherine:
And thank you to all of our partners. To learn more about CLL and to access tools to help you become a proactive patient, visit powerfulpatients.org. I’m Katherine Banwell.
Thanks for joining us today, and please make sure to fill out the survey that you receive after the program. It helps us as we develop more webinars like this one.