Understanding High-Risk DLBCL
Understanding High-Risk DLBCL from Patient Empowerment Network on Vimeo.
What is high-risk diffuse large B-cell lymphoma (DLBCL) exactly? Dr. Jane Winter explains progression of the disease, DLBCL subgroups, and treatment approaches that may bring high-risk DLBCL under control.
Dr. Jane Winter is a hematologist and medical oncologist at Robert H. Lurie Comprehensive Cancer Center at Northwestern University. More information on Dr. Winter here.
See More From The Pro-Active DLBCL Patient Toolkit
Related Programs:
Understanding Diffuse Large B-cell Lymphoma (DLBCL) and Its Subtypes |

|
|
Transcript:
Laura Beth:
Dr. Winter, what is high-risk DLBCL?
Dr. Winter:
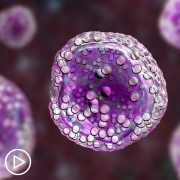
There are certain aggressive lymphomas that are more high-grade. And in recent years, we’ve identified a subset that has genetic changes in certain genes that lead to a very aggressive type of lymphoma that grows rapidly and is more difficult to cure with standard therapy. And what’s most important about identifying that subset is that it requires that at least most of our evidence is that the standard strategy that I just spoke about briefly in terms of what we use for transformed follicular lymphoma, the standard therapy we use for diffuse large B-cell lymphoma called R-CHOP where the “R” is standing for rituximab.
Again, that antibody that targets a particular marker on the lymphoma cells, CD20 immunotherapy plus chemotherapy, CHOP chemotherapy which has been around for probably 50 years, this very standard backbone of treatment for diffuse large B-cell lymphoma is not sufficient. We don’t have head-to-head randomized phase three trials showing definitely that the more aggressive strategy is so much better, but most of the evidence is that standard R-CHOP just doesn’t do as well in curing these highly aggressive, and what we call high grade or double hit lymphomas.
These are lymphomas that have these genetic changes, rearrangements in particular genes MYC and BCL2, and I like to think of it as MYC takes the brakes off of growth. So, it’s sort of the rapidly growing disease, and the BCL2 prevents the cells from dying. So, between that, you have a rapidly growing lymphoma that doesn’t stop. And so, that’s a special subgroup of diffuse large B-cell lymphoma. There are some other subcategories.
Primary mediastinal, which tends to be a type of aggressive lymphoma that presents generally as a big mediastinal mass in the middle of the chest, usually younger patients, more often women than men, but still many, many men as well. So, high-risk generally for me means that it has a double hit. There’s MYC, M-Y-C, and BCL2 genetic changes. There are some other types, but that’s basically what I think of in terms of high-risk. When we think of garden-variety diffuse large B-cell lymphomas, there are some ways of categorizing patients into four different subcategories in terms of “risk.”
The first of these was what we call the international prognostic index that was developed in the 70s based on patients who were enrolled on clinical trials. In those days, the diagnoses were probably not exactly what they are today in terms of how we categorize patients, but that is a set of clinical features that there’s a little app online and you can calculate whether a patient is high-risk, intermediate, low, low-intermediate risk. In this system remains fairly helpful, predictive. But, we have refined it significantly in modern times.
And I have to say, not to toot my own horn, but one of my fellows, Dr. Zhao and I, a number of years ago using a database from the National Comprehensive Cancer Network, and patients who all treated with modern therapy and were diagnosed with modern techniques, we used that data to develop a new, improved international prognostic index. And this helps us better discriminate the four different categories, and it places greater weight on patient age, which is an important predictor, as well as the particular blood test result, the LDH, which is an enzyme that’s helpful in aggressive lymphomas and diffuse large B-cell lymphoma.
And, this particular, what we call the NCCN-IPI, you can just put your age and LDH level and so on into this app and you just find it online, NCCN–IPI, and it will put patients into four different subgroups. And this predict outcomes and survival over a five-year period for these patients. It’s not hard and fast, like anything else, within every category. So, if you look at every patient in the low-risk group by the NCCN–IPI, there still are a few patients who will fail therapy, but the majority of patients will do very well.
And, if you happen to be someone who is 80 years old with a high LDH and you fall into the high-risk patient group, the outcomes are not going to be as good, but that doesn’t mean every patient in that category fails treatment. So, there’s still gonna be some good outcomes. So, it’s helpful. These are guides, and they do help to identify patients who are, what we call, high-risk or high intermediate risk. So, this is another way of looking at predicting outcome apart from looking at whether a patient is what we call a “double hit” lymphoma. So, the double hit, I just want to make one point is that when a pathologist makes a diagnosis of diffuse large B-cell lymphoma, it is absolutely critical that that biopsy, the pathology be sent for a procedure called FISH.
That stands for fluorescent in situ hybridization, and it’s a technique the pathologist can use, or special labs will use, to pull out, to identify those patients who have this very high-risk subset of lymphoma called the double hit with both a MYC and a BCL2 rearrangement. Whether a MYC and a BCL6 rearrangement falls into this same risk group, we’re deemphasizing that and really, it’s the double MYC and BLC2 group that’s the highest risk.