Head and Neck Cancers
This was originally posted by the National Cancer Institute here.
What are cancers of the head and neck?
Cancers that are known collectively as head and neck cancers usually begin in the squamous cells that line the moist, mucosal surfaces inside the head and neck (for example, inside the mouth, the nose, and the throat). These squamous cell cancers are often referred to as squamous cell carcinomas of the head and neck. Head and neck cancers can also begin in the salivary glands, but salivary gland cancers are relatively uncommon. Salivary glands contain many different types of cells that can become cancerous, so there are many different types of salivary gland cancer.
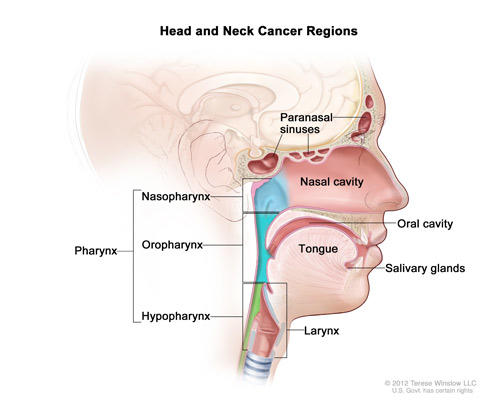
Cancers of the head and neck are further categorized by the area of the head or neck in which they begin. These areas are described below and labeled in the image of head and neck cancer regions.
Oral cavity: Includes the lips, the front two-thirds of the tongue, the gums, the lining inside the cheeks and lips, the floor (bottom) of the mouth under the tongue, the hard palate (bony top of the mouth), and the small area of the gum behind the wisdom teeth.
Pharynx: The pharynx (throat) is a hollow tube about 5 inches long that starts behind the nose and leads to the esophagus. It has three parts: the nasopharynx (the upper part of the pharynx, behind the nose); the oropharynx (the middle part of the pharynx, including the soft palate [the back of the mouth], the base of the tongue, and the tonsils); the hypopharynx (the lower part of the pharynx).
Larynx: The larynx, also called the voicebox, is a short passageway formed by cartilage just below the pharynx in the neck. The larynx contains the vocal cords. It also has a small piece of tissue, called the epiglottis, which moves to cover the larynx to prevent food from entering the air passages.
Paranasal sinuses and nasal cavity: The paranasal sinuses are small hollow spaces in the bones of the head surrounding the nose. The nasal cavity is the hollow space inside the nose.
Salivary glands: The major salivary glands are in the floor of the mouth and near the jawbone. The salivary glands produce saliva.
Cancers of the brain, the eye, the esophagus, and the thyroid gland, as well as those of the scalp, skin, muscles, and bones of the head and neck, are not usually classified as head and neck cancers.
Sometimes, cancerous squamous cells can be found in the lymph nodes of the upper neck when there is no evidence of cancer in other parts of the head and neck (1). When this happens, the cancer is called metastatic squamous neck cancer with unknown (occult) primary. More information about this cancer type can be found in Metastatic Squamous Neck Cancer with Occult Primary (PDQ®).
What causes cancers of the head and neck?
Alcohol and tobacco use (including smokeless tobacco, sometimes called “chewing tobacco” or “snuff”) are the two most important risk factors for head and neck cancers, especially cancers of the oral cavity, oropharynx, hypopharynx, and larynx (2–5). At least 75% of head and neck cancers are caused by tobacco and alcohol use (6). People who use both tobacco and alcohol are at greater risk of developing these cancers than people who use either tobacco or alcohol alone (6–8). Tobacco and alcohol use are not risk factors for salivary gland cancers.
Infection with cancer-causing types of human papillomavirus (HPV), especially HPV type 16, is a risk factor for some types of head and neck cancers, particularly oropharyngeal cancers that involve the tonsils or the base of the tongue (9–11). In the United States, the incidence of oropharyngeal cancers caused by HPV infection is increasing, while the incidence of oropharyngeal cancers related to other causes is falling (9). More information is available at the HPV and Cancer page.
Other risk factors for cancers of the head and neck include the following:
Paan (betel quid). Immigrants from Southeast Asia who use paan (betel quid) in the mouth should be aware that this habit has been strongly associated with an increased risk of oral cancer (12, 13).
Preserved or salted foods. Consumption of certain preserved or salted foods during childhood is a risk factor for nasopharyngeal cancer (14, 15).
Oral health. Poor oral hygiene and missing teeth may be weak risk factors for cancers of the oral cavity (16, 17). Use of mouthwash that has a high alcohol content is a possible, but not proven, risk factor for cancers of the oral cavity (16, 17).
Occupational exposure. Occupational exposure to wood dust is a risk factor for nasopharyngeal cancer (14, 15). Certain industrial exposures, including exposures to asbestos and synthetic fibers, have been associated with cancer of the larynx, but the increase in risk remains controversial (18). People working in certain jobs in the construction, metal, textile, ceramic, logging, and food industries may have an increased risk of cancer of the larynx (19). Industrial exposure to wood or nickel dust or formaldehyde is a risk factor for cancers of the paranasal sinuses and nasal cavity (20–22).
Radiation exposure. Radiation to the head and neck, for noncancerous conditions or cancer, is a risk factor for cancer of the salivary glands (16, 23, 24).
Epstein-Barr virus infection. Infection with the Epstein-Barr virus is a risk factor for nasopharyngeal cancer (25) and cancer of the salivary glands (26, 27).
Ancestry. Asian ancestry, particularly Chinese ancestry, is a risk factor for nasopharyngeal cancer (14, 15).
The symptoms of head and neck cancers may include a lump or a sore that does not heal, a sore throat that does not go away, difficulty in swallowing, and a change or hoarseness in the voice. These symptoms may also be caused by other, less serious conditions. It is important to check with a doctor or dentist about any of these symptoms. Symptoms that may affect specific areas of the head and neck include the following:
Oral cavity. A white or red patch on the gums, the tongue, or the lining of the mouth; a swelling of the jaw that causes dentures to fit poorly or become uncomfortable; and unusual bleeding or pain in the mouth.
Pharynx. Trouble breathing or speaking; pain when swallowing; pain in the neck or the throat that does not go away; frequent headaches, pain, or ringing in the ears; or trouble hearing.
Larynx. Pain when swallowing or ear pain.
Paranasal sinuses and nasal cavity. Sinuses that are blocked and do not clear; chronic sinus infections that do not respond to treatment with antibiotics; bleeding through the nose; frequent headaches, swelling or other trouble with the eyes; pain in the upper teeth; or problems with dentures.
Salivary glands. Swelling under the chin or around the jawbone, numbness or paralysis of the muscles in the face, or pain in the face, the chin, or the neck that does not go away.
How common are head and neck cancers?
Head and neck cancers account for approximately 4% of all cancers in the United States (28). These cancers are more than twice as common among men as they are among women (29). Head and neck cancers are also diagnosed more often among people over age 50 than they are among younger people.
Researchers estimated that more than 65,000 men and women in this country would be diagnosed with head and neck cancers in 2017 (29).
How can I reduce my risk of developing head and neck cancers?
People who are at risk of head and neck cancers―particularly those who use tobacco―should talk with their doctor about ways that they may be able to reduce their risk. They should also discuss with their doctor how often to have checkups. In addition, ongoing clinical trials are testing the effectiveness of various medications in preventing head and neck cancers in people who have a high risk of developing these diseases. Descriptions of these clinical trials can be accessed by searching NCI’s list of cancer clinical trials. NCI’s list of cancer clinical trials includes all NCI-supported clinical trials that are taking place across the United States and Canada, including the NIH Clinical Center in Bethesda, MD. For information about other ways to search the list, see Help Finding NCI-Supported Clinical Trials.
Information specialists from NCI’s Cancer Information Service (CIS) can also help people find clinical trials for the prevention of head and neck cancers. The CIS can be reached at 1–800–4–CANCER (1–800–422–6237) or by chatting with a cancer information specialist online through LiveHelp.
Avoiding oral HPV infection may reduce the risk of HPV-associated head and neck cancers. However, it is not yet known whether the Food and Drug Administration-approved HPV vaccines Gardasil®, Gardasil 9®, and Cervarix® prevent HPV infection of the oral cavity, and none of these vaccines has yet been approved for the prevention of oropharyngeal cancer. More information about these vaccines is in the NCI fact sheet Human Papillomavirus (HPV) Vaccines.
How are head and neck cancers diagnosed?
To find the cause of the signs or symptoms of a problem in the head and neck area, a doctor evaluates a person’s medical history, performs a physical examination, and orders diagnostic tests. The exams and tests may vary depending on the symptoms. Examination of a sample of tissue under a microscope is always necessary to confirm a diagnosis of cancer.
If the diagnosis is cancer, the doctor will want to learn the stage (or extent) of disease. Staging is a careful attempt to find out whether the cancer has spread and, if so, to which parts of the body. Staging may involve an examination under anesthesia (in an operating room), x-rays and other imaging procedures, and laboratory tests. Knowing the stage of the disease helps the doctor plan treatment.
How are head and neck cancers treated?
The treatment plan for an individual patient depends on a number of factors, including the exact location of the tumor, the stage of the cancer, and the person’s age and general health. Treatment for head and neck cancer can include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of treatments.
People who are diagnosed with HPV-positive oropharyngeal cancer may be treated differently than people with oropharyngeal cancers that are HPV-negative. Recent research has shown that patients with HPV-positive oropharyngeal tumors have a better prognosis and may do just as well on less intense treatment. An ongoing clinical trial is investigating this question.
More information about treatment for specific types of head and neck cancers is in the following PDQ® cancer treatment summaries, which are available in patient and health professional versions, as well as in Spanish (the links below go to the patient versions in English):
- Hypopharyngeal Cancer
- Laryngeal Cancer
- Lip and Oral Cavity Cancer
- Metastatic Squamous Neck Cancer with Occult Primary
- Nasopharyngeal Cancer
- Oropharyngeal Cancer
- Paranasal Sinus and Nasal Cavity Cancer
- Salivary Gland Cancer
The patient and the doctor should consider treatment options carefully. They should discuss each type of treatment and how it might change the way the patient looks, talks, eats, or breathes.
What are the side effects of treatment?
Surgery for head and neck cancers often changes the patient’s ability to chew, swallow, or talk. The patient may look different after surgery, and the face and neck may be swollen. The swelling usually goes away within a few weeks. However, if lymph nodes are removed, the flow of lymph in the area where they were removed may be slower and lymph could collect in the tissues, causing additional swelling; this swelling may last for a long time.
After a laryngectomy (surgery to remove the larynx) or other surgery in the neck, parts of the neck and throat may feel numb because nerves have been cut. If lymph nodes in the neck were removed, the shoulder and neck may become weak and stiff.
Patients who receive radiation to the head and neck may experience redness, irritation, and sores in the mouth; a dry mouth or thickened saliva; difficulty in swallowing; changes in taste; or nausea. Other problems that may occur during treatment are loss of taste, which may decrease appetite and affect nutrition, and earaches (caused by the hardening of ear wax). Patients may also notice some swelling or drooping of the skin under the chin and changes in the texture of the skin. The jaw may feel stiff, and patients may not be able to open their mouth as wide as before treatment.
Patients should report any side effects to their doctor or nurse, and discuss how to deal with them.
Where can I find more information about clinical trials for patients with head and neck cancers?
People interested in taking part in a clinical trial should talk with their doctor. Information about clinical trials is available in the NCI publication Taking Part in Cancer Treatment Research Studies. This resource describes how research studies are carried out and explains their possible benefits and risks.
What rehabilitation or support options are available for patients with head and neck cancers?
The goal of treatment for head and neck cancers is to control the disease, but doctors are also concerned about preserving the function of the affected areas as much as they can and helping the patient return to normal activities as soon as possible after treatment. Rehabilitation is a very important part of this process. The goals of rehabilitation depend on the extent of the disease and the treatment that a patient has received.
Depending on the location of the cancer and the type of treatment, rehabilitation may include physical therapy, dietary counseling, speech therapy, and/or learning how to care for a stoma. A stoma is an opening into the windpipe through which a patient breathes after a laryngectomy, which is surgery to remove the larynx. The National Library of Medicine has more information about laryngectomy in MedlinePlus.
Sometimes, especially with cancer of the oral cavity, a patient may need reconstructive and plastic surgery to rebuild bones or tissues. However, reconstructive surgery may not always be possible because of damage to the remaining tissue from the original surgery or from radiation therapy. If reconstructive surgery is not possible, a prosthodontist may be able to make a prosthesis (an artificial dental and/or facial part) to restore satisfactory swallowing, speech, and appearance. Patients will receive special training on how to use the device.
Patients who have trouble speaking after treatment may need speech therapy. Often, a speech-language pathologist will visit the patient in the hospital to plan therapy and teach speech exercises or alternative methods of speaking. Speech therapy usually continues after the patient returns home.
Eating may be difficult after treatment for head and neck cancer. Some patients receive nutrients directly into a vein after surgery or need a feeding tube until they can eat on their own. A feeding tube is a flexible plastic tube that is passed into the stomach through the nose or an incision in the abdomen. A nurse or speech-language pathologist can help patients learn how to swallow again after surgery. The NCI booklet Eating Hints: Before, During, and After Cancer Treatment contains many useful suggestions and recipes.
Is follow-up care necessary? What does it involve?
Regular follow-up care is very important after treatment for head and neck cancer to make sure that the cancer has not returned, or that a second primary (new) cancer has not developed. Depending on the type of cancer, medical checkups could include exams of the stoma, if one has been created, and of the mouth, neck, and throat. Regular dental exams may also be necessary.
From time to time, the doctor may perform a complete physical exam, blood tests, x-rays, and computed tomography (CT), positron emission tomography (PET), or magnetic resonance imaging (MRI) scans. The doctor may monitor thyroid and pituitary gland function, especially if the head or neck was treated with radiation. Also, the doctor is likely to counsel patients to stop smoking. Research has shown that continued smoking by a patient with head and neck cancer may reduce the effectiveness of treatment and increase the chance of a second primary cancer.
Additional information can be found at NCI’s Follow-Up Medical Care page.
How can people who have had head and neck cancers reduce their risk of developing a second primary (new) cancer?
People who have been treated for head and neck cancers have an increased chance of developing a new cancer, usually in the head, neck, esophagus, or lungs (30–32). The chance of a second primary cancer varies depending on the site of the original cancer, but it is higher for people who use tobacco and drink alcohol (30).
Especially because patients who smoke have a higher risk of a second primary cancer, doctors encourage patients who use tobacco to quit. Information about tobacco cessation is available from NCI’s Cancer Information Service at 1–800–4–CANCER (1–800–422–6237) and in the NCI fact sheet Where To Get Help When You Decide To Quit Smoking. The federal government’s main resource to help people quit using tobacco is BeTobaccoFree.gov.The government also sponsors Smokefree Women, a website to help women quit using tobacco, and Smokefree Teen, which is designed to help teens understand the decisions they make and how those decisions fit into their lives. The toll-free number 1–800–QUIT–NOW (1–800–784–8669) also serves as a single point of access to state-based telephone quitlines.
Tests for Head and Neck Cancers
This was originally published by the Cancer Council here.
In this section we look at the different tests you may have to see if you have a head and neck cancer.
Learn more about these tests for head and neck cancers:
- Physical examination
- Nasendoscopy
- Laryngoscopy
- Biopsy
- Imaging tests
Physical examination
Depending on your symptoms, the doctor will examine your mouth, throat, nose, neck, ears and/or eyes. They may use a thin wooden tongue depressor to see inside the mouth more clearly. The doctor may also insert a gloved finger into your mouth to feel areas that are difficult to see, and gently feel both sides of your neck to check your lymph nodes.
The doctor may use equipment to see some areas of the head and neck, such as the nasopharynx, tongue base and pharynx.
Nasendoscopy
In this procedure, your doctor examines the nose and throat area using a thin flexible tube with a light and camera on the end. This device is called a nasendoscope. Before the nasendoscope is inserted, a local anaesthetic is sprayed into the nostril to numb the nose and throat.
You may find that the spray tastes bitter. The doctor will gently pass the nasendoscope into one of your nostrils and down your throat to look at your nasal cavity, nasopharynx, oropharynx, hypopharynx and larynx. Images from the nasendoscope may be projected onto a screen. This test may feel uncomfortable, but should not hurt.
You will be asked to breathe lightly through your nose and mouth, and to swallow and make sounds. The doctor may also take tissue samples (biopsy). A nasendoscopy usually takes a few minutes. If you need a biopsy, the test may take longer. You will be advised to not have any hot drinks for about 30 minutes after the procedure, but you can go home straightaway.
Laryngoscopy
This procedure allows the doctor to look at your throat and voice box, and take a tissue sample (biopsy). The doctor inserts a tube with a light and camera on the end (laryngoscope) into your mouth and throat. The camera projects images onto a screen. The procedure is done under a general anaesthetic and takes 10–40 minutes. You can go home when you’ve recovered from the anaesthetic. You may have a sore throat for a couple of days.
| A bronchoscope is similar to a laryngoscope, but it allows doctors to examine the airways to see if cancer is present in the lungs. The tube (bronchoscope) is inserted into the lungs via the mouth and throat. This may be done under a local or general anaesthetic. |
Head & Neck Cancer Screening Guidelines
This resources was original published by Memorial Sloan Kettering Cancer Center here.
The term “head and neck cancer” encompasses a wide range of tumors that occur in several areas of the head and neck region, including the nasal passages, sinuses, mouth, throat, larynx (voice box), swallowing passages, salivary glands, and the thyroid gland. The two major known risk factors for head and neck cancer are exposure to tobacco and heavy use of alcohol. A type of cancer of the head and neck known as head and neck squamous cell carcinoma (HNSCC) is a relatively uncommon disease, with 40,000 new cases and 10,000 deaths estimated in 2008 in the United States. Twenty-five percent of HNSCCs harbor human papillomavirus (HPV), a commonly occurring virus that may play a role in the development of head and neck cancer. Non-squamous cancers of the head and neck — which include tumors of the thyroid, skin adnexa, salivary glands, sarcomas, and lymphomas — are even more uncommon.
Head and Neck Cancer Risk – High-Risk Groups
Heavy exposure to tobacco and heavy use of alcohol are well documented as major risk factors for head and neck cancer. In addition, patients cured of HNSCC have an approximately 10 percent risk of developing second primary cancers of the head and neck at five years after treatment. Individuals with a premalignant lesion in the mouth known as dysplastic oral leukoplakia have an almost 30 percent risk of oral cancer at ten years after treatment. Individuals with the following diseases and syndromes are at increased risk for head and neck cancer: Fanconi anemia, a rare, inherited disease in which the bone marrow fails to function properly; Li-Fraumeni syndrome, a rare, inherited disorder that greatly increases the risk of developing several types of cancer; and Plummer-Vinson syndrome, a disorder characterized by long-term iron deficiency anemia, which causes swallowing difficulty.
Head and Neck Cancer Screening Tests
Currently, there are no screening methods that have been proven to increase survival rates for HNSCC. A screening physical examination of the neck, oropharynx (the middle section of the throat that includes the soft palate, the base of the tongue, and the tonsils), and the mouth has been widely adopted as part of a routine dental examination. However, there is no evidence that this intervention reduces mortality from oral cancer. It is likely that in the coming decades this routine screening will allow earlier identification of oral cancer, when it is in a less advanced form, but this has yet to be proven in clinical studies.
At Memorial Sloan Kettering Cancer Center, we offer yearly free head and neck screenings in the spring to anyone in the community. These screenings provide an opportunity to educate interested patients on awareness of oral cancer and its risk factors.
There are no HNSCC screening guidelines from the American Cancer Society, the National Comprehensive Cancer Network (NCCN), or the National Cancer Institute. And, at present, there are no known tests of blood or saliva proven to be effective for detection of HNSCC.
Our Head and Neck Screening Guidelines
Our doctors advise that all individuals have a yearly physical examination of the head and neck and oropharynx (the middle section of the throat that includes the soft palate, the base of the tongue, and the tonsils) conducted by their primary care physician, as well as a yearly routine dental evaluation to include examination of the neck and inspection of the oropharynx and the mouth.
Our Screening Guidelines for High-Risk Patients
For high-risk patients cured of HNSCC, our doctors use the NCCN’s follow-up guidelines outlined below to look for both recurrence of the initial cancer and second primary cancer formation.
Physical exam
- Year One: every one to three months
- Year Two: every two to four months
- Years Three to Five: every four to six months
- Year Five and Beyond: every six to 12 months
Chest x-ray annually
If an individual has received radiation treatment of the thyroid, then a TSH thyroid function test should be performed annually.
For high-risk patients with surgically unremovable or recurrent dysplastic oral leukoplakia, our doctors recommend observation on the same schedule as above and biopsies for suspicious changes in the lesions. These patients are also sometimes eligible to be enrolled in prospective clinical trials in head and neck cancer prevention at Memorial Sloan Kettering.