Lamar’s Story | Renal Medullary Carcinoma from Patient Empowerment Network on Vimeo.
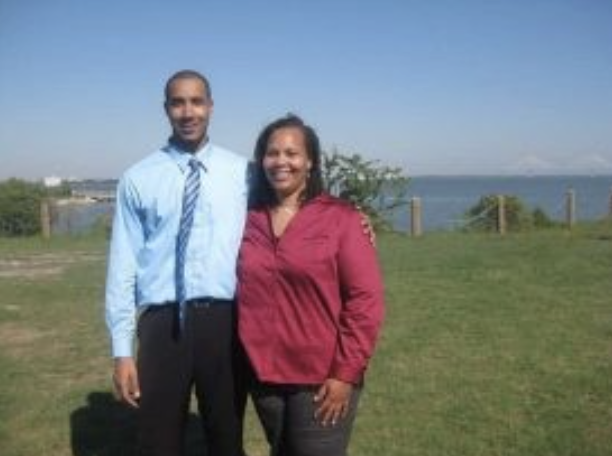
Renal medullary carcinoma patient and active-duty U.S. Air Force member Lamar Valentina shares important pieces of his RMC journey. Watch as he discusses the symptoms that led to his RMC diagnosis, his treatment journey, things he found helpful for support, and his hopes for how to educate others about sickle cell trait and RMC for better health outcomes.
Transcript:
Lamar Valentina:
I’m Lamar Valentina, I was diagnosed September 25th, 2019. What prompted me to be checked was I had a lump that was literally right here, it kind of protruded out, and I had some really bad abdominal pain as well as flank pain on my left side, it was really unbearable, so those three things combined — I got really concerned and decided to go to the hospital.
I’m in the military, active-duty military, so working out and kind of taking breaks, it’s common for me to get lower back pain, but it was definitely a different lower back pain, and then with the added lump that was between here, it was literally right here. And this kind of has actually gone down, so that’s a sign from my oncologist that says that the cancer is shrinking based off treatment. So diagnosed on September 25th, 2019. I started chemotherapy on October 11th of 2019. There were a few options. I had some friends that work in cancer centers, and my ex-wife actually works with foundation on medicine, and they had connections at Dana Farber in Boston, and that’s where she lives with my son who’s 12, who will be 13 in March. Starting chemo on October 11th, the first cycle that I was on was Carboplatin-Taxol, I did that for about six cycles, and there was shrinkage, but due to COVID, we took a break to give my body a break, ’cause chemotherapy did a big number on my body, I lost a lot of weight, obviously my hair and my eyebrows, my hair is still gone, my eyebrows are still gone, and it just…
With my body adjusting to chemotherapy was pretty rough, but I handled it well, so actually that break… During that time, I said about three months, two months through my break, I want to say we did that until about February, and then we started back up in April, so about three months and that was more so because of COVID and creating delays in between. But once we got a scan and we saw that there was a little bit of growth, it wasn’t alarming growth, but there was some growth, but it still hadn’t gone to where it was when I first was diagnosed, so that was the good thing that it wasn’t as aggressive as it’s known to be.
Throughout this whole ordeal, it’s been family, friends. Throughout the beginning, you know you have a lot more support and it kind of balances out, which is fine, ’cause I’m a pretty introverted person anyway, but I have a great immediate circle that’s there to share positive affirmations and positive vibes and positive energy. And that’s honestly what helps me through that, along with music and staying productive, I’m still actively in school and still in the Air Force, active duty, I make 14 years, and next month in March, and my hope is that through this campaign and through everything else, we just continue to raise as much awareness as possible. I was always told growing up that sickle cell trait really was nothing to worry about, unless if I had a child with someone else that had the sickle cell trait, and then our child would be fully diagnosed with sickle cell, so I’ve never really even thought to be concerned about having a trait of sickle cell, so my hope is that through this campaign and through other everything else, we’re able to raise as much awareness as possible to grab the right people’s attention that are going to continue to put forth the proper research to help save more lives and of course, to live my life as long as possible, for as long as I’m here, and if I can hopefully inspire and motivate others along that through my hardships, hopefully that’ll help them to create a survival guide for their own lives moving forward. Whatever it is they may go through, but especially with RMC.
For anyone who’s recently diagnosed, my best advice is lean on your support team, your support circle, it’s going to be very, very hard, don’t be so quick to Google everything, but do try to make sure that you’re as informed as possible about your diagnosis about RMC, and then finding a community that fits. That’s exactly what I did as soon as I was diagnosed, of course. I did what I’m telling people not to do by Googling and everything, because once you Google everything, you’re going to get everything negative under the sun, but it is very important to be informed properly based off what you’re going to be going through, you’re down for the moment, but you’re not out, you just got a dig deep and make sure the people around you are sharing that positive energy and those positive vibes to continue to provide you with the motivation and then at a strength and the courage to fight, and it’s also okay to deal with the emotions that you may be going through. Some people feel that, “Oh, you got to be strong.” Being strong doesn’t mean not crying or not feeling sad, you’re going to feel every emotion imaginable once you are diagnosed.
So, it’s okay, the best thing is to do is to process that and hopefully have an outlet or somebody that you can share that with, and you can kind of unload it ’cause you don’t want to compartmentalize those feelings and those emotions because it doesn’t go anywhere, it just kind of festers, it’s like sweeping it under the rug, it’s going to pile up and just really, really become a lot.
So really, really lean on your support system, and if you don’t have a support system, I guarantee if you research it like I did. Reaching out to Cora Connor has been amazing, ’cause they put me in touch with other people that were going through what I’m going through, and talking with people who are going through, who can relate to what you’re going through is way different than talking to people who don’t really have an idea of what it is that you’re going through, not saying that they can’t help and they can’t be there for you, but it’s just, it’s a different type of comfort that comes from knowing someone that is literally sharing the same symptoms or going through the same treatment, or may have gone through the same treatment or the same procedures that you may be up against, and you can ask some questions and get a realistic answer from somebody with experience as opposed to getting assumptions or things from other people, but I would say stay positive. Stay as positive as possible. Don’t give up hope. Don’t give up hope.
It doesn’t have to be a significant other for other people that are going through if you’re single, it could just be your best friend, it could be a friend. Motivation and inspiration comes from the most strangest of places, and I’ll be witnessed. I’ll be the first to admit to that on the top of having someone, but there’s times when you often feel alone and you kind of think about how this impacts and affects them, those closest to you as well. So, I think taking that into consideration is something that people who are really diagnosed as well to guess we are the center of it, were the ones who actually are going through it, but the people that love and care about you, they’re going through it in a way as well too, they’re definitely affected and impacted by this too.