How Can You Access Personalized Prostate Cancer Treatment? from Patient Empowerment Network on Vimeo.
How could genetic testing results affect your prostate cancer treatment plan? In this INSIST! Prostate Cancer webinar, Dr. Sumit Subudhi will discuss key prostate cancer tests, the latest targeted therapies and tools to help you advocate for a personalized treatment approach and insist on better care.
Dr. Sumit Subudhi is a Medical Oncologist at The University of Texas MD Anderson Cancer Center.
Download Program Resource Guide
Related Resources
Transcript:
Katherine:
Welcome to Insist Prostate Cancer, a program focused on empowering patients to insist on better care. Today we’ll discuss the latest advances in prostate cancer, including the role of genetic testing and how this may affect treatment options.
I’m Katherine Banwell, your host for today’s program. And joining me is Dr. Sumit Subudhi. Welcome, Dr. Subudhi. Would you please introduce yourself?
Dr. Subudhi:
Hi, I’m Sumit Subudhi. I’m a medical oncologist at MD Anderson Cancer Center, and I specifically focus on prostate cancer.
Katherine:
Excellent, thank you. Before we start, a reminder that this program is not a substitute for seeking medical advice. Please refer to your own healthcare team. Well, Dr. Subudhi, I’d like you to begin with a brief explanation of the stages of prostate cancer.
Dr. Subudhi:
Yeah, that’s a great question. So, we use stages, and there’s four – Stage I, II, III, and IV. And we use it to help us determine what treatments the patients need for their prostate cancer. In general, Stage I is localized prostate cancer, and it’s localized only to the prostate. And when we do a digital rectal exam, we cannot feel or palpate the prostate.
And the treatment for Stage I prostate cancer is either active surveillance, where you’re not trying to cure the cancer, you’re just actively watching it, and you’re using a PSA imaging studies, prostate biopsies, and digital rectal exams at regular intervals to follow the patients. But other patients with Stage I prostate cancer can actually get definitive treatment for curative intent with radiation therapy or surgery. Stage 2 prostate cancer is also localized, but on physical exam, we can actually palpate or feel the prostate cancer. And this also can receive definitive treatment for the prostate to cure it, and that, also, you can use radiation therapy and surgery.
Stage III is what I consider locally advance. This is where the prostate cancer is now starting to leave the prostate. And it still can be cured by radiation and surgery, but most likely needs a multidisciplinary approach, where you might need both or maybe even in addition of a systemic therapy. Stage IV is the last stage that I’ll talk about, and it has distant metastases. And here we’re not looking for a curative approach; we’re actually looking for palliation, which means that we’re trying to treat the prostate cancer as a chronic disease.
Katherine:
I understand that there are many types of prostate cancer that have been identified. How can patients advocate for a precise diagnosis?
Dr. Subudhi:
Yes, you’re absolutely right. There are many types. So, we have historically used histological classification. And when I say histological, that means when we look at the cancer under the microscope, we can look at the different structures within the prostate cancer and classify them.
And there are multiple types such as adenocarcinoma, neuroendocrine, small-cell, mucinous, etc. But more recently, with the advances in genetic and molecular testing, we now can look at the genes inside the prostate cancer, and that has also helped us better classify the cancer. Now many of these types of approaches are best done at major cancer centers, where they have experienced pathologists who actually evaluate both histologically and molecularly the cancer.
So, I recommend to my patients, or family and friends, that have been diagnosed with prostate cancer that they don’t necessarily have to go to the major cancer centers. They can have their local doctor send the tissue from the biopsy to the advanced cancer centers to get a second opinion.
Katherine:
But this would be an initial visit to a doctor. Is that right?
Dr. Subudhi:
Good question. So, I’m presuming that the patient is actually being seen at a local center where they have a local doctor, and so they don’t have to come, for example, to MD Anderson Cancer Center to see me. They could actually have their tissue sent to our pathologists and get it reviewed, and they can still be at home. And especially in this era of COVID, that’s important.
Katherine:
What is the role of genetic testing in prostate cancer?
Dr. Subudhi:
That’s a great question, because this is something that wasn’t really available when I was training and understanding prostate cancer. But over the last few years, this has actually hit the mainstream, and it’s very important. And I see it having three roles. The first role is whether or not you can receive a certain type of targeted therapy or systemic therapy known as PARP inhibitors. So, if your genetic test is positive for certain markers – that I think we’ll cover later – then it can help give you more treatment options. The second is that generate testing can give you also risk of other cancers besides prostate cancer. For example, if you have the BRCA mutation, you’re 15% to 20% more likely to get breast cancer in men.
The third is that because the genetic testing is looking for inheritable mutations in your genes, that means you can pass it along to your kids. And this could have a tremendous impact on the screening strategies your children want to use in the future.
Katherine:
Would you mind going into that a little bit?
Dr. Subudhi:
Yeah.
Katherine:
For instance, my ex-husband had early prostate cancer. My 22-year-old son is worried now about also getting prostate cancer. His grandfather had prostate cancer.
Dr. Subudhi:
Yeah, great question. So, it’s not just about prostate cancer. So, prostate cancer, genetically, is linked to other cancers, as well.
So, in your case, you’re turning by your son. But if you have daughters or any female members in the family, consideration needs to be given to breast and ovarian cancer. And for both men and women, we also have to think about melanoma and pancreatic cancer. So, it’s not just prostate cancer that we’re thinking about when you have these genetic risks. And that’s very important, because each of these different cancers can have different screening modalities.
Katherine:
Oh. Well, how is the testing administered then?
Dr. Subudhi:
The testing is actually a blood test, so very simple.
Katherine:
Have there been any major advances in testing?
Dr. Subudhi:
Yeah, so when we’re talking about the inheritable testing, that’s just a simple blood test. And the reason why it can be done simply through the blood is because every cell in your body has it. So, when they collect the blood, they can just take any cell from there and do genetic analysis. And if that gene is mutated or missing, it will be captured.
Now, there’s another type of testing where they test your tumor tissue itself – so, your cancer tissue – whether you got it by biopsy or surgically removed. And so, that’s a different type of testing. That’s looking for what we call somatic mutations. These are not inherited mutations. These are mutations that are specific for your prostate cancer. Again, in contrast, the inheritable mutations are in every cell in your body – not just your prostate cancer cells, but every cell in your body. And the somatic, it’s just in your prostate tissue itself.
And so, sometimes with prostate cancer, it’s difficult to get the tissue. And what’s happened more recently – and to answer your question – is that the advances have been in what we call liquid biopsies, where they are able to use your blood and get the DNA from the tumors and actually genetically test the cancers that way. And so, that’s where the future is going.
Katherine:
Oh, that’s amazing. Are there specific tests that patients should ask their doctor for following the diagnosis?
Dr. Subudhi:
Yeah. So, if inpatients with high risk or metastatic prostate cancer, they should definitely be considering tests to see if they have mutations in what we call the DNA damage repair pathway or homologous recombination DNA pathway. And I know they’re fancy terms. What these genes are, they’re genes that help the body repair their DNA, and DNA is very important. And so, when there’s defects in the DNA repair pathway, then mutations occur. And these mutations can actually help the cancer grow.
Now what’s happening is that what they’re looking for in these genetic tests – whether it’s the inheritable test or the somatic mutation test that’s looking just within the tumor itself – they’re looking to see if there’s any DNA damage machinery that’s defective. And if it is, then you’re more likely to benefit from PARP inhibitors, which are oral drugs that specifically target the DNA repair pathway.
Katherine:
All right. Dr. Subudhi, what is the link between inherited mutations and prostate cancer?
Dr. Subudhi:
Yeah, so in approximately 10% to 15% of patients with prostate cancer, they have an inheritable cause for their cancer. And so, this predisposes them to not just having prostate cancer, but potentially to other cancers, but also their family members.
Katherine:
Would you give us an overview of common mutations in prostate cancer?
Dr. Subudhi:
Yeah. So, in regards to the inheritable causes, the BRCA mutations – BRCA2 and BRCA1 – are very common. In fact, BRCA2 is more common than prostate cancer than BRCA1. In addition, there’s CHEK2 and ATM which are common inheritable mutations. And the other ones are the mismatch repair genes. Again, all these play an important role in repairing DNA. So, if you’re mutated in these genes, then your ability to repair DNA has been significantly diminished, and you’re more likely to gain more mutations.
Katherine:
How do these mutations affect disease progression?
Dr. Subudhi:
Yeah. So, what they can do is they can lead to mutations that make the cancer grow more. And there’s two ways to do it. You can have a mutation in what we call an oncogene, a gene that when it’s active, it’s going to just promote the cancer.
And then we have other genes called tumor suppressor genes. Their normal function is to prevent the cancer from growing. But if the tumor suppressor gene gets mutated so it’s no longer functional, then the cancer can then take off, because it’s no longer suppressed. So, those are how these genes can actually affect the prostate cancer.
Katherine:
What about treatment options, what’s available?
Dr. Subudhi:
Yeah. So, if you have either an inheritable mutation in these genes or a somatic mutation, then there’s a chance that the PARP inhibitors could actually work for you. And the PARP inhibitors, they actually target cancers where there’s a defect in the DNA repair pathway.
Now, there’s one thing that I want to point out that a lot of people sort of are missing, and it’s not a subtle point. Not all inheritable mutations are made the same – or even somatic mutations. Meaning, what we’re learning is the PARP inhibitors seem to be more active with the “Braca,” or BRCA, mutations and the ATM mutations. Whereas, they’re less active with other types of DNA repair mutations. So, the point is not all mutations are made the same.
Katherine:
Let’s turn to targeted therapies. How exactly do they work?
Dr. Subudhi:
Yeah. So, this is a form of personalized medicine. So, what you’re doing is you’re looking at the patient’s cancer, either their inheritable cause of genetic causes or the somatic. And then you’re saying, oh, wait, they have a genetic defect in a DNA machine. So, let’s use the PARP inhibitor, which also targets the DNA machinery.
And these are the cancer cells that are most likely to be susceptible to PARP inhibition. And actually, the cancer cells will die from it. Whereas if a patient has a normal DNA machinery, the PARP inhibitors will actually not have any effect on the cancer.
Katherine:
Oh, I see. Just as a follow-up, how are these targeted therapies administered?
Dr. Subudhi:
They’re given, actually, orally twice a day. The two drugs are rucaparib and Olaparib that have been FDA approved for this indication.
Katherine:
How do these newer treatments differ from traditional chemotherapy?
Dr. Subudhi:
That’s a great question. So, with chemotherapies, at least in prostate cancer, they’re given intravenously every three weeks. And the goal of the chemotherapies, they are actually designed to kill any actively dividing cell in the body.
And the problem is it’s not just cancer cells that are actively dividing in our body. For example, with the chemotherapy such as docetaxel or cabazitaxel, that’s used in prostate cancer – their brand names are Taxotere and Jevtana – these chemotherapies will also affect hair loss. Why? Because hair grows really fast. And in fact, I need a haircut every three to four weeks, which my wife has been helping me with.
So, the chemotherapies are targeting all actively dividing cells, and that’s why you also get nausea vomiting, because the cells of our GI tract are also affected by that. So, chemotherapies are not personalized. They’re there to kill actively dividing cells. Luckily prostate cancer divides a lot more quickly than any other cell in our body, and that’s why they’re susceptible to chemotherapy.
Katherine:
And as far as the targeted therapies, Dr. Subudhi, are there side effects with those?
Dr. Subudhi:
Yeah, there are. One of the most predominant side effect is actually anemia. And so, that’s when the red blood cells in our body are lower than usual. And so, that’s one of the major side effects for PARP inhibitors. But in addition, you can have nausea, vomiting, and diarrhea as other side effects with the PARP inhibitors.
Katherine:
What are you excited about in prostate cancer research right now?
Dr. Subudhi:
So, to me, it’s the combination of treatments. So, not just treating with one PARP inhibitor or just one hormonal therapy, it’s combining these approaches, and especially with immunotherapies, so that we can potentially cure what’s considered incurable cancer. To me, that’s the most exciting.
Katherine:
What would you say to patients who are nervous about participating in a clinical trial?
Dr. Subudhi:
Yeah. This is a common question that I deal with in clinic, because we tend to have a lot of trials at MD Anderson. And the first thing, for me, is to understand why they’re nervous, because there’s different reasons why people are nervous.
Some people have heard of placebo trials, where the experimental drug that they’re hoping to get is only given to a portion of the patients and not all. And so, patients are worried what if they get on the placebo arm. And so, what I tell patients in that case is that please note that you’re going to be monitored very closely – more than usual, and so I’ll be seeing you in clinic more often. And if there’s any signs of progression, I will take you off the study. But I also always have a back-up plan. So, I tell them this is the next drug I’m going to give you if you progress, so don’t worry, I’ve got a plan for you. So, that’s one thing.
The other thing that people get concerned about are experimental drugs – just the fact that they are experimental. And I have to remind them that all these standard therapies that we have for prostate cancer were all experimental at one point. And it was the courage of the other patients that went through clinical trials that helped bring it as standard of care. And then sometimes some people have issues with travel, and those are more logistical issues. And especially now with the COVID era, we have to think about that. And so, we’re also trying to find and use networks to see if there’s other trials that are more amenable for patients so they don’t have to travel far.
Katherine:
How can patients find out about clinical trials that may be right for them?
Dr. Subudhi:
Yeah. So, one way is using clinicaltrials.gov. And that’s a website that allows you to search for specific trials either by drug name or by disease type – so, for example, prostate cancer. So, that’s one resource. And the others are cancer societies like the American Cancer Society or ASCO or Prostate Cancer Foundation. They also have links to clinical trials that are exciting.
Katherine:
Do you recommend having patients see a specialist?
Dr. Subudhi:
Absolutely. I think that if you have a metastatic disease, you need to have a medical oncologist on board that can still work with your urologist, who’s more surgically trained.
Katherine:
Right. Well, we’ve talked about COVID a couple of times, and I’d be remiss if we didn’t touch upon it now. What should prostate cancer patients be considering at this time, especially those with advanced disease?
Dr. Subudhi:
Yeah, so what I don’t want are people to say, oh, I can wait a little bit longer to contact my physician, whether it’s primary care or a prostate cancer doctor, because of COVID. I think it’s very important that the medical team is up to date on a patient’s symptoms and what’s going on medically, whether it’s related to prostate cancer or not. And so, that’s one of the messages we’ve been trying to pass on to our patients.
And with every single patient, we try our best to see if we can provide medical care as well as expertise without having physically see them through telehealth, whether it’s through video or whether it’s just through a simple phone call. So, we’re trying to look at that with each individual patient. Now, sometimes when there’s treatment decisions that have to be made – especially like do we start chemotherapy? – it’s harder to do that over the phone. But sometimes what I’ll do for my patients that are in areas where COVID is really worrisome, I’ll work with the local medical oncologist and talk to them and basically see if we can develop a plan together so that the patient can be served best.
Katherine:
Is there a time when telemedicine is more appropriate than others?
Dr. Subudhi:
I think that has to be a case-by-case basis. And that’s how we do it in clinic.
Every week, a week before hand, I go through my entire clinic list – I go through each patient’s case – and I say, okay, this is a patient that would be better served with telemedicine, this is a case that I really need to see the patient to get a better sense of what to do next.
Katherine:
If a patient has to go into clinic, what safety measures are in place for them?
Dr. Subudhi:
Yeah, so I can only speak for our hospital and how we’re doing it. But there’s actually like a thermal scan where when you walk in the building, they actually measure your temperature without you even knowing it. But they delete it, so it’s not something that’s kept. And this is still kept private, so you don’t have to worry about public disclosure of your temperature. And so, they’re monitoring both the staff and the patients – their temperatures. The staff themselves have to go through screening questions that they have to answer every time, and they’re actually handed a mask that’s required to be used at all times.
As far as patients go, they are also getting their temperature measured. But in addition, they are asking questions about their exposures, whether it’s family members that are asymptomatic, or not symptomatic. And in addition, the new patients will get a COVID test done prior to seeing the medical team. And for the follow-up patients, they’re not required to get a COVID test unless there’s concerns of symptoms.
Katherine:
Unless they’ve been exposed to somebody?
Dr. Subudhi:
Correct, that’s right. Thanks for pointing that out. In addition, all patients are asked to wear their masks at all times, especially if they’re going to be within 6 feet of a healthcare provider or a patient or anyone else. And so, these are the measures that we’re taking to keep our patients safe.
Katherine:
Oh, good. Dr. Subudhi, what advice do you have for patients who may be hesitant to speak up an advocate for themselves when it comes to their own care and treatment?
Dr. Subudhi:
Yeah, I’d say that it’s interesting because we all do this ourselves. And when it comes to our car – let’s say a car breaks down, or if we’re trying to buy furniture – we’ll get three, four different opinions. But for ourselves, for our own body, we don’t do that. And when you watch – we were talking earlier about Major League Baseball – and these players, when they get injured, they get the three best specialists in the world to evaluate them. And they’re seeing the best of the best.
And so, we owe it to ourselves and the patients owe it to themselves to actually get second opinions. I encourage it. I encourage my patients to get second opinions, even if I’m the first doctor they see, because I want them to feel comfortable with their decision.
And it’s important to understand that just because you’re seeing a doctor doesn’t mean that it’s a one-size-fits-all. You will get different opinions from different doctors, and you have to go with the one that makes you feel most comfortable.
Katherine:
We have a question from the audience, Dr. Subudhi. Amy is saying she’s the daughter of a prostate cancer patient. And she’s curious to know how she goes about getting genetic testing, and if her children should be tested, as well.
Dr. Subudhi:
Yeah. So, one of the things is that family history is very important in determining who should get genetically tested. So, if you’re a prostate cancer patient and you have metastatic disease, you should get genetically tested. And the reason for that is because we have a new set of drugs, the PARP inhibitors. But if you’re a family member that’s wanting to know whether you have a loved one has inheritable cancer that you may end up inheriting, that requires more understanding of the family history.
For example, did the grandfather have prostate cancer? Did the uncle have prostate cancer? And as I mentioned earlier, it’s not just prostate cancer. Is there a family member with breast cancer or ovarian cancer? These things play out in the decision-making of who should be genetically tested.
Katherine:
Absolutely. As a researcher in the field doctor, Dr. Subudhi, what would you like to leave patients with? Are you hopeful?
Dr. Subudhi:
Yeah, I’m very hopeful. It’s a really interesting time, because with the technological advances and scientific advances – Traditionally, prostate cancer has always been treated just with hormonal therapies from the 1930s all the way to early 2000. Then in 2004, chemotherapy became the next thing. And then after chemotherapy, we’ve now got a dendritic cell vaccine; we’ve also got a radiopharmaceutical agent. And so, what the point is now we have a lot more different FDA-approved agents. And now, experimentally, the PARP inhibitors have now become a standard of care for those patients with mutations in the BRCA1, BRCA2, or ATM.
And then, in addition, we have many other types of technologies, such as BiTE and CAR T cells, that are coming out that are showing in early studies to be exciting. And so, I feel like that these therapies in combination may actually lead us to cure the cancer.
Katherine:
ASCO happened in June. Was there any news that patients should know about?
Dr. Subudhi:
Yeah, so the PARP inhibitors got a lot of press during ASCO, as they should, because this is a new class of drugs that is the first personalized version of medicine that we have in prostate cancer. Now, personalized medicine has been around for a long time in cancers such as breast and lung cancer. But for first time, we actually have it in prostate cancer.
Katherine:
Dr. Subudhi, I want to thank you so much for joining us today.
Dr. Subudhi:
Thank you for your time. I really appreciate it.
Katherine:
And thank you to all of our partners. To learn more about prostate cancer and to access tools to help you become a more proactive patient, visit powerfulpatients.org. I’m Katherine Banwell.







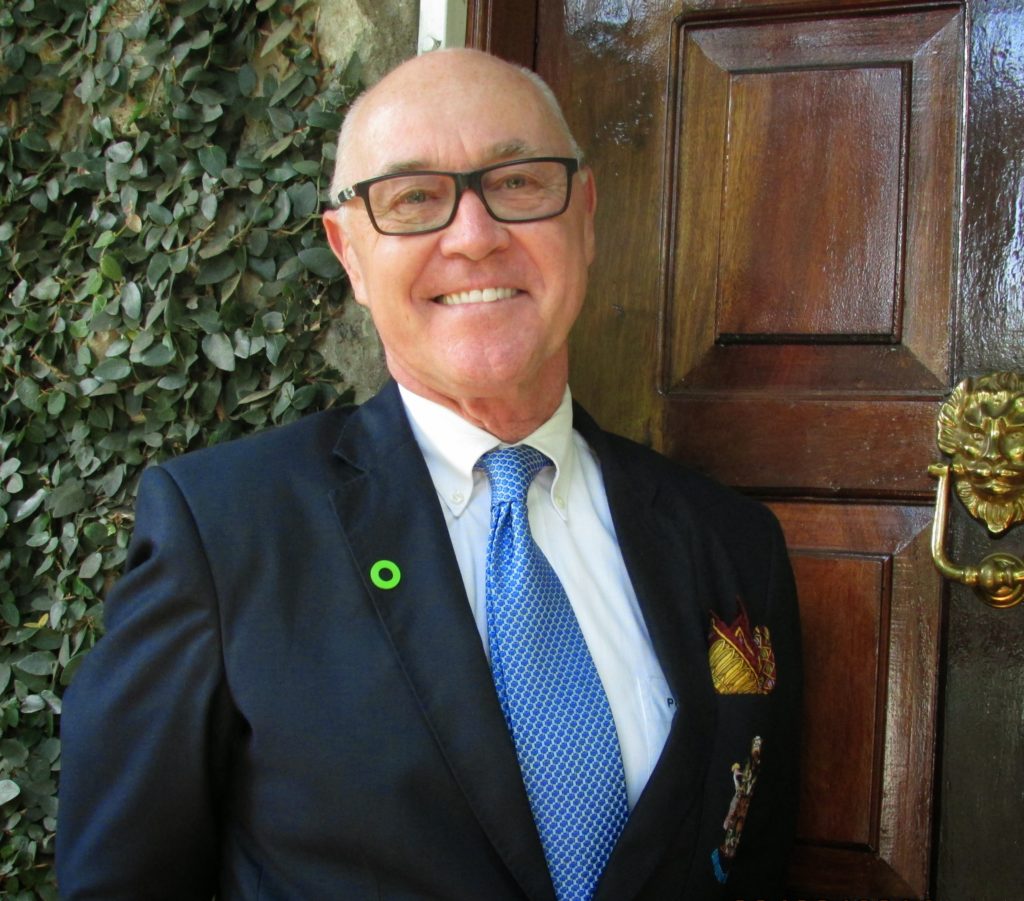 Peter Blaze Corcoran concedes that there is never a good time to get a stage four cancer diagnosis, but he says his diagnosis came at a time in his life when he felt secure in managing it. It was 2015 and he was a university professor nearing retirement. He had insurance, a supportive employer, and access to excellent medical care. “It came at a time when I was mature enough, secure enough, and knowledgeable enough,” says Peter. “I felt quite stable in dealing with it.” It was
Peter Blaze Corcoran concedes that there is never a good time to get a stage four cancer diagnosis, but he says his diagnosis came at a time in his life when he felt secure in managing it. It was 2015 and he was a university professor nearing retirement. He had insurance, a supportive employer, and access to excellent medical care. “It came at a time when I was mature enough, secure enough, and knowledgeable enough,” says Peter. “I felt quite stable in dealing with it.” It was 

