FLT3 Inhibitors for AML Update
Introduction
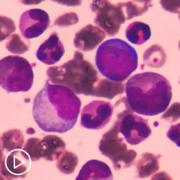
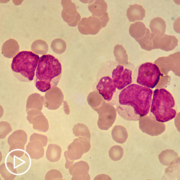
Mutations in the FLT3 (fms-like tyrosine kinase 3) gene are the most common mutations seen in Acute Myeloid Leukemia (AML) patients. FLT3 mutations are seen in about 30% of AML patients. There are 2 different FLT3 mutations, FLT3-ITD (internal tandem duplication) mutation and tyrosine kinase domain mutations (TKD) mutation. Here I report some newer results of treatments with FLT3 inhibitors, that I have come across in the last several months.
There are quite a few drugs that target the FLT3 gene, including:
First generation drugs:
- Sorafenib (Nexavar)
- Midostaurin (Rydapt)
- Lestaurtinib clinical development of lestaurtinib has been discontinued as it did not provide significant clinical benefit.
Second generation drugs, which tend to have fewer and less severe side effects and are more effective include:
- Gilteritinib (Xospata)
- Quizartinib (Vanflyta) – Only for ITD mutations.
- Crenolanib – Not FDA approved.
FLT3 inhibitors are effective treatments for AML with a FLT3 mutation. However, there are still a number of open questions. How should FLT3 inhibitors be used, with induction chemo, with consolidation chemo and/or for maintenance after a stem cell transplant (SCT) or chemo? Can they be used as a single agent for treating patients who are not good candidates for chemotherapy? Do they work well with newer treatments, specifically with azacitidine and ventoclax regimens? There have not been a lot of comparison between the different drugs. Finally, there is the question of why all these drugs have names that are barely pronounceable!
Gilterinib
There is a new study looking at the use of gilterinib as maintenance after SCT. This was a multi-national randomized study, comparing maintenance with gIlterinib against placebo. The result was overall the patients who received gilterinib had better relapse-free survival (RFS) compared to patients who received placebo. However, this difference was not considered statically significant. However, the trial had a pre-specified secondary objective to look at the subgroup of patients who had measurable residual disease (MRD), that is they were MRD+.
About half of the patients were MRD+ either before SCT or after (or both). In this group, the RFS survival in the patients receiving gilterinib was significantly greater than the placebo group. Unfortunately, there were more side effects in the gilterinib group. It is likely that, because of this study, patients who are FLT3+ and undergoing a transplant will get gilterinib as maintenance if they are MRD+ and not if they are MRD-. The use of gilterinib or other FLT3 inhibitors as maintenance therapy will continue to be a subject of active research.
Quizartinib
I wrote a post on quizartiinb: Quizartinib in FLT3-ITD-Positive AML that was an overview of a trial of this drug along with induction and consolidation chemo and as maintenance after chemotherapy. In July, 2023, Quizartinib was approved for treatment of FLT3-ITD AML in the United States by the FDA.
Crenolanib
Crenolanib is a second-generation FLT3 agent that works for both FLT3-ITD and FLT3-TKD mutations. In Crenolanib and Intensive Chemotherapy for Adults With Newly Diagnosed FLT3-Mutated AML, crenolanib was given with “7+3:” induction and then with consolidation chemotherapy and as maintenance therapy after consolidation chemo and after a SCT. About 2/3 of patients were younger than 60, but patients as old as 75 were included. Although this was not a randomized trial and was fairly small (44 patients), it seemed that Crenolanib added to chemotherapy and as maintenance improved survival compared to midostaurin (the first drug approved for FLT3 AML) and quizartiinb (described above).
Sorafenib
While sorafenib is an FLT3 inhibitor, this first study is on its use in AML patients even if they did have a FLT3 mutation. Previous studies had shown sorafenib improved survival when given with standard “7+3” induction for AML. This study (Sorafenib Plus Cladribine, High-Dose Cytarabine, G-CSF, and Mitoxantrone for Untreated AML) looked at sorafenib with cladribine, high-dose cytarabine, granulocyte colony–stimulating factor, and mitoxantrone (CLAG-M). The first part of the study (Phase I) tried increasing doses of sorafenib and mitoxantrone. The Phase II part of the study used the recommended phase 2 dose (RP2D) to treat more patients. When compared with historical controls who received CLAG-M without sorafenib, the patients who received the RP2D had improved survival.
Finally, there is a report on the long term follow-up of a trial looking at using sorafenib as maintenance therapy after a transplant (Sorafenib Maintenance After Allogeneic HSCT in Patients With AML With FLT3 Internal Tandem Duplications). The use of sorafenib as maintenance reduced relapse which improved survival in patients with FLT3-ITD AML. The non-relapse mortality and the incidence of chronic Graft-Versus-Host Disease (GVHD) in those who had a transplant was similar in patients who received sorafenib and those who did not. This result was sustained long-term (with a median follow-up of about 5 years).
Conclusion
The best way to use FLT3 inhibitors in patients with FLT3 mutation is still an area of active research. Newer agents promise better results – fewer side effects and better survival.
Further Reading
FLT3 Tyrosine Kinase Inhibitors for the Treatment of Fit and Unfit Patients with FLT3-Mutated AML: A Systematic Review, Int J Mol Sci. 2021 Jun; 22(11): 5873.
Molecular Mechanisms of Resistance to FLT3 Inhibitors in Acute Myeloid Leukemia: Ongoing Challenges and Future Treatments, Cells 2020, 9(11), 2493.
Gilteritinib as Posttransplant Maintenance for AML With Internal Tandem Duplication Mutation of FLT3, Practice Update (registration required, free), March 26, 2024.
Gilteritinib as Post-Transplant Maintenance for Acute Myeloid Leukemia With Internal Tandem Duplication Mutation of FLT3, Medscape, June 21, 2023.
Gilteritinib as Post-Transplant Maintenance for Acute Myeloid Leukemia With Internal Tandem Duplication Mutation of FLT3, Journal of Cinical Oncology. March 12, 2024..
Quizartinib Approval Adds New Treatment Option for AML, Including in Older Patients , National Cancer Institute, Cancer Currents Blog , August 15, 2023.
Crenolanib and Intensive Chemotherapy for Adults With Newly Diagnosed FLT3-Mutated AML, Practice Update (registration required, free), March 4, 2024.
Crenolanib and Intensive Chemotherapy in Adults With Newly Diagnosed FLT3-Mutated AML (JCO article) Journal of Clinical Oncology February 07, 2024.
Sorafenib Plus Cladribine, High-Dose Cytarabine, G-CSF, and Mitoxantrone for Untreated AML Practice Update (registration required, free), July 25, 2023.
Phase 1/2 study of sorafenib added to cladribine, high-dose cytarabine, G-CSF, and mitoxantrone in untreated AML, Blood Adv (2023) 7 (17): 4950–4961.
Sorafenib Maintenance After Allogeneic HSCT in Patients With AML With FLT3 Internal Tandem Duplications, Practice Update (registration required, free), July 25, 2023.
Sorafenib maintenance after allogeneic haemopoietic stem-cell transplantation in patients with FLT3-ITD acute myeloid leukaemia: long-term follow-up of an open-label, multicentre, randomised, phase 3 trial, The Lancet, Volume 10, ISSUE 8, e600-e611, August 2023

AML Network Manager
Art Flatau lives in Austin, Texas with his wife Gretchen. They have 2 grown children. He was diagnosed with Acute Myeloid Leukemia (AML) in 1992 at the age of 31, while still in graduate school at the University of Texas. Gretchen and Art’s kids were 2 and 4 at the time. He received chemotherapy (both induction chemotherapy and then consolidation). After graduating with a Ph.D. in computer science in December 1992. He relapsed in early 1993 and then had a bone marrow transplant (BMT), his brother was a perfect match.