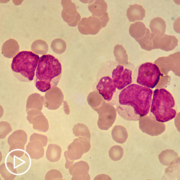
Patient Empowerment Network (PEN) is committed to helping educate and empower patients and care partners in the acute myeloid leukemia (AML) community. AML is shown to impact younger patients compared to other types of blood cancer. In addition, there are some marginalized communities of Black and Latinx AML patients that experience disparities in health outcomes. Recent studies in AML have shown higher mortality rates and higher rates of AML recurrence in Black and Latinx patient groups. PEN aims to help empower patients in their care. With this goal in mind, we kicked off the [ACT]IVATED AML program, which aims to inform, empower, and engage patients to stay abreast of the latest in AML care.
Disparities in AML Treatment and Health Outcomes
AML research studies show that Black and Latinx patients experience disparities in AML treatment and health outcomes. Some of the study findings include:
A recent study in Blood Advances showed that Black adolescent and young adult (AYA) patients with AML have higher mortality rates and higher rates of AML recurrence in comparison to white patients. The study compared clinical outcomes between 1983 and 2016 for AYA patients between the ages of 18 and 29. The early mortality rate of Black AYA patients was 16 percent compared to 3 percent for white AYA patients. When examining complete AML remission rates, 66 percent of Black AYA patients experienced complete remission compared to 83 percent of white AYA patients. The authors of the study looked at the research data and determined that delayed diagnosis and treatment in the Black AYA patients as well as genetic differences of AML likely led to the higher mortality rate for this group. In comparison, Black and white patients between the ages of 30 and 39 showed no significant differences in their survival rates.
Lead study author Dr. Karilyn Larkin, a hematologist at the OSUCCC – James, shared, “To our knowledge, this is the first study to examine how molecular genetic alterations contribute to outcomes in young Black people with AML compared with their white counterparts.” Study of genetics is extremely vital in developing new and refined AML treatments, and this is why it’s more important than ever for more Black AYA patients to join clinical trials to create a larger pool of participants to learn from.
Another recent study in Blood showed that Hispanic/Latinx and Black AML patients have higher mortality rates in comparison to white AML patients. The study analyzed several factors in the disparities including health care access, tumor biology, treatment patterns, ICU admission during induction chemotherapy, comorbidities, and structural racism. Neighborhood measures of structural racism were found to be a major predictor of AML mortality rates. The neighborhood measures that were tracked in the study included census tract disadvantage, segregation, and affluence. The study authors concluded that more research must be done to learn the ways that structural racism relates with different AML treatment and predictive factors to impact health outcomes. Then more actions can be taken to help decrease the health disparities for these patient groups.
[ACT]IVATED AML Patient and Expert Tips
Black and Latinx patients who more frequently experience AML disparities are key groups for patient advocacy and empowerment. AML specialists, patients, and patient advocates have pooled some valuable advice through their experiences in treating and living with AML with the goal of improving care for all AML patients. PEN has been fortunate to receive some tips from patient and AML Empowerment Lead Sasha Tanori and AML specialists Dr. Catherine Lai and Dr. Naval Daver toward patient activation and empowerment.
Sasha talked about her AML experience as a Mexican American and the delay in her diagnosis. “You didn’t go out and seek care if you are hurt, you just sucked it up, you went to work, you went to school, you did your job, you took care of your family, and that was it. If you had any type of ailments or illness, you would just rub some Vaseline and do the sana sana and just move on about your day.”
Sasha’s care in a rural healthcare setting also contributed to the delay in her diagnosis. “In my local town they had no clue what was wrong, they didn’t know it was cancer, they didn’t know what was going on. They just kept doing tests after tests after tests, and they’re on blood work, and finally, they were just like, ‘We have no clue, we’ve got to send you somewhere else. You’ve got to get in an ambulance and leave.’”

Dr. Lai advises patients to take proactive actions in their care. “Ask your physician and your oncologist when you’re talking with them about what all the newest therapies are and what would be specifically the best treatment for their specific leukemia with respect to the different mutations.”
Testing has become a key factor in optimizing treatment for each patient’s specific AML. Dr. Daver also stresses the importance of testing. “Patients, when they transformed what we call secondary AML or MDS, seemed to have a higher predilection for certain high-risk communications such as TP53, and these are best treated with ongoing frontline clinical trials at large academic centers.”
Dr. Daver also explained the importance of genetic mutations currently under study in combination clinical trials. “Patients should be checked for arrangements like MLL rearrangement NPM1 mutation, new fusions as these may be amenable to therapy with the menin inhibitors, there are multiple trials with five different menin inhibitors, single agent trials and also combination trials now ongoing across multiple centers both in the U.S. and ex-U.S.”
The future of AML care is full of hope, and Dr. Lai shared her perspective. “There are a lot of new, exciting therapies that are coming out, and that it’s really novel sequencing strategies and combinations that I think will be the future of AML.”
Clinical trial participation continues its vital role in improving AML care, and Dr. Daver took the opportunity to stress the importance of trials. “Clinical trials are critical, both for the patients themselves to get access to what we call tomorrow’s medicine today as well as potentially to help move the entire field forward.”
[ACT]IVATED AML Program Resources
The [ACT]IVATED AML program series takes a three-part approach to inform, empower, and engage both the overall AML community and AML patient groups who experience health disparities. The series includes the following resources:
- [ACT]IVATED Expert Interviews with experts Dr. Catherine Lai and Dr. Naval Daver moderated by an AML patient
- [ACT]IVATED Resource Guide (en Espanol here) a downloadable, printable support resource packed with a newly diagnosed patient checklist, expert tips, AML facts, AML mutations, cytogenetic abnormalities, and support resources
- [ACT]IVATED Patient Vignettes to learn valuable experiences and lessons learned from other AML patients
- [ACT]IVATED Activity Guide – a downloadable, printable support resource packed with information and activities to educate, empower, and support AML patients and care partners in their journeys through care
Though the underrepresented AML groups of Black and Latinx patients have experienced health and care disparities, experts and patient advocates are taking action to improve care for all. By shining the light on gaps in care, PEN aims to aid in reducing these gaps along with continued research advances and clinical trial participation. AML patients can educate and empower themselves to become more confident and active partners in their care. By doing so, they can make more informed decisions for improved health outcomes. We hope you can continue to use the [ACT]IVATED AML program resources to advance your path to becoming an informed, empowered, and engaged patient.








![[ACT]IVATED AML Resource Guide](https://powerfulpatients.org/wp-content/uploads/ACTIVATED-AML-Resource-Guide-180x180.png)