Tag Archive for: myeloma
What Is a FISH Test?
What is a FISH Test? from Patient Empowerment Network on Vimeo.
What is a FISH test for multiple myeloma patients? Watch as expert Donna Catamero explains how fluorescent in situ hybridization (FISH) testing is used, and myeloma patient and Empowerment Lead Lisa Hatfield shares her experience with FISH testing and her advice to other patients.
See More from START HERE Myeloma
Related Resources:

|

|

|
Transcript:
Donna Catamero:
So, FISH is a cytogenetic technique. So, what we do is, when we do the bone marrow, we send that off and we look at the genetics. Like I said, it’s a snapshot. And certain mutations will put patients in different risk stratifications, so we normally do this at the time of diagnosis and then with each relapse.
In a FISH test, a bone marrow biopsy is taken to map out the genetic material of a cell using fluorescent dyes. These dyes show specific parts of chromosomes and help locate genetic issues like 11;14 translocation, 17 deletion, and others that are important in determining multiple myeloma treatment. If you have not had a FISH test, make sure to ask your doctor if the test should be performed to aid in your diagnosis and treatment.
Lisa Hatfield:
The first time I heard FISH test I had no idea what my doctor was talking about. It was actually a nurse practitioner who works with my myeloma specialist who said, “Your FISH test came back, and you have two abnormalities. One of them is called translocation 11;14, standard risk. And one is called monosomy 13, which sometime in the past used to be considered a higher risk but apparently it’s not anymore.” She was trying to explain this to me. I had no idea what she meant what a FISH test was. As time went on and I started to study a little bit more, do a little bit more research on myeloma, I understand the significance and the importance of having a FISH test done for anyone who’s getting diagnosed at a local hospital or community cancer center. I encourage everyone to make sure they can have a FISH test done even if that means consulting with a myeloma specialist to ensure that they can find those cytogenetic abnormalities or to test for those. Because that will help guide your treatment and your prognosis going forward. You want to know what those cytogenetic abnormalities are. They’ll be tracking those over time. So a FISH test is kind of confusing. But without going into too much detail, it’s an interesting test that they can do. It’s very helpful if it’s done at diagnosis. Important to be done at diagnosis, so those genetic abnormalities can be tracked over time through further testing.
What Is Early MGUS?
What is Early MGUS? from Patient Empowerment Network on Vimeo.
What happens in early MGUS, or monoclonal gammopathy of undetermined significance? Watch as expert Dr. Irene Ghobrial explains MGUS and how often it progresses, and patient and Empowerment Lead Lisa Hatfield shares her advice and information about ongoing research studies on MGUS.
See More from START HERE Myeloma
Related Resources:

|

|

|
Transcript:
Dr. Irene Ghobrial:
So MGUS, or monoclonal gammopathy of undetermined significance, is a precursor or the stage before myeloma happens, and it’s actually a very common disease or entity in many, many of us as we get older. In fact, maybe 5 percent of the population over the age of 50 would have this early MGUS.”
The condition of MGUS does not usually impact a person’s health or result in any symptoms. MGUS is most often found on a routine blood test that notes a high level of protein in the blood, and additional tests show the protein is a monoclonal antibody.
Though MGUS is not a cancer, it is sometimes classified pre-malignant since some patients with MGUS eventually develop cancers such as lymphoma, multiple myeloma, or amyloidosis.
Lisa Hatfield:
So MGUS, or monoclonal gammopathy of undetermined significance, is the precursor to typically smoldering myeloma and then to multiple myeloma. Not all MGUS is going to progress to multiple myeloma. In fact, it usually does not. Also important to have a hematologist on board if you are diagnosed with MGUS. There is a study being done right now in Iceland called the iStopMM Study or the Black Swan Study where they are looking at every resident over a certain age to detect how many people in the general population have MGUS. And they follow them over time longitudinally to see how many of those patients who have MGUS will progress to smoldering myeloma and then onto multiple myeloma.
So it’s really interesting. I guess what I would say about MGUS if you’re diagnosed with MGUS, not to panic. You have a lot of time to think about it, to have a hematologist follow you. And typically MGUS, as far as I know, is not treated. It is just monitored to see if it will progress onto smoldering myeloma and then onto multiple myeloma.
Top Two Multiple Myeloma Advances in 2022
What are the top two multiple myeloma advances in 2022? In the “Myeloma Treatment & Research Updates From 2022 ASCO and EHA Meetings” program, expert Dr. Krina Patel from The University of Texas MD Anderson Cancer Center shares promising news and research highlights from these important conferences.
1.DETERMINATION Study
The American Society of Clinical Oncology (ASCO) 2022 conference had a highly anticipated multiple myeloma session with an update about the impact of stem cell transplants. The DETERMINATION study spent over 10 years studying patient outcomes for those who received a stem cell transplant when they were newly diagnosed versus those who didn’t receive a transplant. Researchers were encouraged by the data that showed those who received a transplant at diagnosis kept their myeloma at bay in progression-free survival mode for 21 months longer than those who didn’t receive transplant at diagnosis. In addition, patients who received a stem cell transplant at the point of their second remission experience a long period of progression-free survival or myeloma hibernation.
2. Antigen Studies
Studies on antigens, or sort of flags on multiple myeloma, examined new ways to target myeloma treatment. Researchers discovered the new antigens of FcHR5 and GPRC5D provide novel methods to attack the multiple myeloma. Clinical studies can now look at developing new treatments to attack these antigens. These discoveries are especially important and hopeful for multiple myeloma patients who’ve already received B-cell maturation antigen (BCMA) treatment and then relapse, since BCMA has been the focus of the antigen treatment approach.
Multiple myeloma researchers at the ASCO and EHA conferences have discovered exciting findings and hope for the future of myeloma care. The studies revealed advances for improving care options and for extending progression-free survival periods. If you want to learn more about multiple myeloma care and treatments, check out our multiple myeloma information.
What is Smoldering Myeloma?
What is Smoldering Myeloma? from Patient Empowerment Network on Vimeo.
What occurs during smoldering myeloma? Watch as myeloma expert Dr. Irene Ghobrial explains smoldering myeloma and progression, and patient and Empowerment Lead Lisa Hatfield shares her perspective of learning from smoldering myeloma patients.
See More from START HERE Myeloma
Related Resources:

|

|
Transcript:
Smoldering multiple myeloma, also known as SMM, is an early form of multiple myeloma when patients don’t experience issues or symptoms of the condition.
Dr. Irene Ghobrial:
Smoldering myeloma – and, the name says it; it’s almost myeloma, it has a higher chance of progressing to myeloma – in general, it’s about 10 percent per year, and usually, the bone marrow has more than 10 percent plasma cells…….3:04- 3:23 You want to make sure that patient is followed up carefully, and you want to offer, potentially, clinical trials because we want to prevent progression. The hope in the future is you don’t wait until you have lytic lesions, fractures in your bones, kidney failure, and then we treat. The hope is we treat you earlier, and we can make a huge difference in that early interception for myeloma.
Lisa Hatfield:
So smoldering myeloma, or SMM, smoldering multiple myeloma, is the precursor to multiple myeloma. Not every person who has smoldering is going to move right into myeloma. They have high-risk smoldering myeloma, which is not the same as high-risk multiple myeloma. It’s really important if you’re diagnosed with smoldering myeloma, to find a specialist.
And the reason why is we have a couple people in one of my support groups who were diagnosed with smoldering myeloma. And depending on the provider you talk with, some choose to treat smoldering myeloma. Some choose to watch and wait and monitor that myeloma. The other important thing to know is there are many clinical trials out there for smoldering myeloma patients. And your provider, particularly any specialists you may have contact with, even if it’s just for a consult, they can help navigate you to those clinical trials that might be best for you. Some of them require you to be close to a large medical center. Some of them allow you to live at your local location and just travel maybe once a month or once every couple of months. But it’s really important to talk to a specialist about those clinical trials to see if that would be something that would be of interest to you.
How is Multiple Myeloma Staged?
How is Multiple Myeloma Staged? from Patient Empowerment Network on Vimeo.
How is staging used in multiple myeloma? Watch as expert Dr. Abdullah Khan explains staging and its use, and myeloma patient and Empowerment Lead Lisa Hatfield shares how the use of staging and its factors have evolved over time.
See More from START HERE Myeloma
Related Resources:

|

|
Transcript:
Healthcare professionals use a combination of lab test results, imaging tests, and bone marrow exams to determine the stage of multiple myeloma. The revised International Staging System or Durie-Salmon Staging System may be used in determining a patient’s multiple myeloma stage.
Dr. Abdullah Khan:
“The patients are assigned stages I to III. To determine the ISS you need lab values for the beta-2 microglobulin and albumin. For the revised ISS, you add on the lab value for LDH, lactate dehydrogenase, and you also add in the chromosome risk profile. So, there are certain genetic changes that predict a more aggressive myeloma. And the ones added to the revised ISS staging system are translocation 4;14, translocation 14;16, and deletion 17p.”
Lisa Hatfield:
So staging with multiple myeloma is really unique. A lot of times people think that every cancer has four stages. That is not true with myeloma. There are three stages for myeloma. And even now as of this year, some providers, some oncologists are not even staging myeloma. They’re looking at the risk factors, the cytogenetic risk factors to see if you’re standard risk or high risk. They’re not even using the staging system. It’s interesting. Back when I was diagnosed back in 2018, there were two staging systems used. One was the Durie-Salmon scale. I was diagnosed as stage III, which is the highest level. Mine was based on the fact that I had a lot of bone lesions and bone involvement.
But there’s also one called R-ISS, the revised ISS staging. And that one I was staged at stage I. So it’s really important to get a myeloma specialist on board quickly, because my myeloma specialist explained why I had two different stages I was staged at. She used the R-ISS, the more current system, the stage I and also looked at my cytogenetic risk factors. So your doctor will talk to you about FISH testing. And FISH testing might show something like translocations in the myeloma cells themselves or genetic abnormalities in the myeloma cells themselves. And that helps them dictate also what your risk will be going forward and how to treat that, how to treat your myeloma as a result of those risk factors and the stage you’re diagnosed at.
Your care provider may use other criteria in determining a person’s best optimal treatment. Make sure to ask if you have additional questions.
Where Should I START Following My Myeloma Diagnosis?
Where Should I START Following My Myeloma Diagnosis? from Patient Empowerment Network on Vimeo.
What should multiple myeloma patients do following diagnosis? Watch as myeloma expert Dr. Peter Forsberg shares care and support advice, and patient and Empowerment Lead Lisa Hatfield shares support that she’s found helpful and advice for moving forward to treatment.
See More from START HERE Myeloma
Related Resources:

|

|
|
Transcript:
Being diagnosed with myeloma can be a big shock. Here are some key steps you can take from a myeloma expert:
Dr. Peter Forsberg:
I think the first thing you want to do is make sure you have a care team in place you’re comfortable with. That means support from friends and family. It also means providers you’re comfortable with. Usually you’re diagnosed by an oncologist and hopefully that’s somebody that you already feel a good comfortable relationship with.
I always think it’s worthwhile to consider getting a second opinion, another voice. And that could be even if you’re diagnosed at the most high-power academic center in the country, or whether it’s in a more community-type setting. I think having another voice just to make sure everything makes sense, that it seems fairly consistent, and that you understand things as thoroughly as you can. But you do want to get the ball rolling in terms of making a care plan and moving towards therapy if that’s the next step, without taking too much time.”
Lisa Hatfield:
Well, to start following your myeloma diagnosis, I think the first thing that has to happen is you have to allow yourself time to take in that information from your provider, to think about it, always have another person with you to take notes. Because the shock of getting a cancer diagnosis can overwhelm your mind, and having somebody with a notebook and pen and can take notes during every appointment was really critical for me. My husband went with me, and it was a huge godsend going back and looking at those notes whenever I had to go to another provider to talk about my diagnosis. So I think having a person go with you, having a good medical team, some people prefer to go on the Internet and research myeloma. I did like to do that. I probably found too much information, but it helped me come up with a plan of what type of questions to ask my providers and possibly treatments. I wanted to understand treatments better. So I think trying to figure out your myeloma diagnosis, first start with your medical team, always have somebody with you, and just take your time trying to understand what the team is telling you. There’s usually not a huge rush with a myeloma diagnosis. You don’t have to act within 24 hours, so allow yourself some time.
How is Multiple Myeloma Diagnosed and What Testing is Necessary After?
How is Multiple Myeloma Diagnosed and What Testing is Necessary After? from Patient Empowerment Network on Vimeo.
What testing is involved in multiple myeloma diagnosis and treatment? Watch as myeloma expert Dr. Elizabeth O’Donnell explains specific types of myeloma testing and what they check for, and patient and Empowerment Lead Lisa Hatfield shares testing that she’s received and typical tests for myeloma diagnosis and care.
See More from START HERE Myeloma
Related Resources:

|

|

|
Transcript:
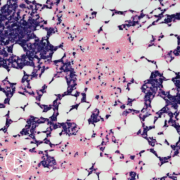
So how is multiple myeloma diagnosed? The International Myeloma Working Group (IMWG) confirms diagnosis with both:
- Presence of malignant plasma cells in the bone marrow at greater or equal to 10 percent or presence of extramedullary or bony plasmacytoma, confirmed with biopsy
- CRAB features:
- Calcium elevation: serum calcium greater than 0.25 mmol/L (> 1mg/dL) higher than the upper limit of normal or greater than 2.75 mmol/L (> 11 mg/dL)
- Renal failure (or kidney failure): creatinine clearance less than 40 mL per minute or serum creatinine greater than 177 μmol/L (> 2 mg/dL)
- Anemia: hemoglobin concentration of greater than 2 g/dL below the lower limit of normal, or a hemoglobin concentration of less than 10 g/dL
- Bony lesions: one or more osteolytic lesions found on X-ray, CT scan, or PET‑CT scan
- Ratio of involved/uninvolved serum free light chain ratio greater than or equal to 100
- Clonal plasma cells in the bone marrow greater than or equal to 60 percent
- One or more focal lesions found on MRI studies (measuring a minimum of 5 mm in size)
Dr. Elizabeth O’Donnell:
Testing really does depend a little bit on the stage at which your disease is found. In general, we use a very specific blood test that lets us know that there is clonal protein present. Remember, plasma cells are a type of white blood cell, and they make something called antibodies. We use a test called a serum protein electrophoresis, which is a blood test – an SPEP, we call it – that can tell us the difference between normal, healthy antibody and clone that are made from the plasma cells that we see in MGUS, smoldering, and multiple myeloma…once we identify that there’s a plasma cell disorder, then that can set in place a workup, depending on the amount of clonal, monoclonal, M-protein that we see.
So, sometimes that involves bone imaging. Historically that was a skeletal survey where we took lots of X-rays of your body. Now we have other tests we use. PET scans, CT scans, whole body MRIs. Sometimes it depends where you’re getting your treatment, and also it depends a little bit on your doctor’s degree of suspicion.
Lisa Hatfield:
So my myeloma was diagnosed using a scan. An MRI was done of my spine, and that’s when my doctor saw the plasmacytoma in my spine. Further testing indicated that I had something called kappa light chain myeloma. So a lot of patients will have regular tests done, blood work that may show anemia. I think if anybody has an indication of myeloma, further testing should be looked at. There’s something called a light chain assay, a normal CBC, a metabolic panel, a light chain assay was critical in my case, because all my protein levels were coming back normal. Some patients have an elevated level of protein in their blood. Mine was normal. So having all the standard blood work plus having the light chain assay done.
And then really the gold standard for diagnosing myeloma, unfortunately, right now is a bone marrow biopsy. It’s not fun. It’s not horrible. So for patients who are anticipating that, you can get through it. It will be okay. That is the gold standard for diagnosing the myeloma, the type of myeloma, and then any cytogenetics related to that myeloma that help guide the therapy that you might be getting going forward.
What is Multiple Myeloma (MM)?
What is Multiple Myeloma (MM)? from Patient Empowerment Network on Vimeo.
What happens in multiple myeloma? Watch as myeloma expert Dr. Peter Forsberg explains what occurs in the body with myeloma, and patient and Empowerment Lead Lisa Hatfield shares emotions she experienced after her diagnosis and how her outlook changed as she learned about myeloma treatment.
See More from START HERE Myeloma
Related Resources:

|

|

|
Transcript:
Dr. Peter Forsberg:
So, multiple myeloma is a blood cancer. It comes from cells that live in your bone marrow called plasma cells. They’re part of your immune system. And when they do their job, they help protect you from infections.
They’re antibody-producing cells. In myeloma, unfortunately something changes in those cells, and they begin to grow and live beyond what they normally would. So, myeloma is a disease that results from that and when myeloma is diagnosed, it’s usually because those plasma cells or the antibody they produce has started to cause problems, to cause destructive changes or symptoms. So, that’s multiple myeloma.
Lisa Hatfield:
When I first really understood what myeloma was, I think it’s natural to freak out at first. It’s an incurable blood cancer. You hear the word “incurable” first, and it’s very very scary. Once I digested some of the information I was receiving and understood it’s a type of blood cancer that can be managed nowadays – it’s a little bit different than 20 years ago when it felt more like a death sentence that could be managed – I started to feel a little more confident. I think initially I had to understand that I would probably go through this grief cycle and have a little bit of shock, have some denial, have some anger. But once I accepted that, it became a lot easier. But when I first understood myeloma, it was was scary, it was shocking. And it just took some time to finally settle in and understand it better.
Three Factors That Determine Myeloma Treatment Decisions
What are the key factors under consideration to determine a multiple myeloma treatment approach? In “Key Factors That Guide Myeloma Treatment Decisions” program, expert Dr. Joshua Richter from Multiple Myeloma at the Blavatnik Family – Chelsea Medical Center at Mount Sinai explains how to determine optimal approaches.
1. Disease-Related Factors
The growth rate of myeloma – whether fast-growing or slow-growing – is a key factor in treatment decisions. Treatment in pill form may be an option for slow-growing myeloma, while intravenous or other treatment methods may be necessary to treat fast-growing myeloma.
2. Treatment-Related Factors
A myeloma specialist will also take treatment-related factors into account. Some of these considerations will include issues like whether a patient stopped responding – or was refractory – to another treatment. Or if a patient experienced treatment side effects that couldn’t be lessened enough through adjusting dosage or by other means, that should be considered as well.
3. Patient-Related Factors
Myeloma treatment options must also take other patient health concerns into account. Considerations like physical fitness, kidney health, heart health, and medical problems like high blood pressure and diabetes must be considered. In addition, the patient’s myeloma symptoms must be weighed in the analysis for treatment decisions.
Myeloma specialists have some key factors to consider in narrowing down an optimal treatment approach. If you’d like to learn more about multiple myeloma, check out our multiple myeloma information.
CAR T-Cell Therapy Care Partners: Tools for Accessing Support
CAR T-Cell Therapy Care Partners: Tools for Accessing Support from Patient Empowerment Network on Vimeo.
How can care partners access support during the CAR T-cell therapy process? Expert Dr. Amitkumar Mehta discusses the support patients may need during CAR T and resources for accessing patient and family support.
Dr. Amitkumar Mehta is Director of the Lymphoma Program and CAR T Program and Medical Director of the Clinical Trials Office at O’Neal Comprehensive Cancer Center at UAB. Learn more about Dr. Mehta.
See More from The Care Partner Toolkit: CAR T-Cell Therapy
Related Resources:

Why Is a Care Partner Essential for Patients Undergoing CAR T-Cell Therapy? |

|

How Is CAR T-Cell Therapy Changing the Myeloma Treatment Landscape? |
Transcript:
Katherine:
What support services or resources are available for care partners of patients who are undergoing CAR T-cell therapy?
Dr. Mehta:
Unfortunately, I have to say that there are not that many support systems existing. It depends on the center most of the time. And, remember, that many of the centers – you know, CAR T is not offered at every community center.
Usually, they are certified centers. So, on an average, patients might have to travel to go to the center, right? So, it’s mainly center dependent. Now – and, you know, like, if I talk about my center, as I was mentioning, that I like to have the caregiver as a part of the process so they are aware what the patient is going through. Second person is – or second team person is our clinic nurse or CAR-T coordinator who actually talks to the patient in depth as well as patient’s caregiver.
Now, if you are living farther away from the center, three hours, four hours, five hours, in that case, where do I lodge myself, whether there is any other support system? We are going to stay here. Where I’m going to eat? Where is the center? Where do I have to them, whether I have to take them daily or not? So, those kinds of information is provided mainly by the center.
And centers also have many other support systems that we can tap in. The most important is to highlight is CAR T is not cheap. It’s very expensive treatment, right? So, there’s an extra step of insurance approval. Well, what is your copay? So, financial toxicity so to speak also come in picture and not only for the patients but their caregiver also.
We need to sit down if they need additional help. What other sources? What are the other agencies or maybe a local church or local community it can help? One other thing that our center has done, which has helped quite a bit, we have a patient ambassador. There was a patient who had gone through CAR T, and he had such an experience that he decided to offer his service to other patients who were going through CAR T. And he is always available.
So, he always – whenever he comes for the clinic visit and says “I’ll be happy to talk to anyone including his family, right, his mother and his father. They’re available that if [they support the patient], the caregiver, we would like to talk to them. And we would like to share our experience. And, if they have any questions, we can share the resources available to go through CAR T because, at the end, it’s a potentially curative option.
Why Is a Care Partner Essential for Patients Undergoing CAR T-Cell Therapy?
Why Is a Care Partner Essential for Patients Undergoing CAR T-Cell Therapy? from Patient Empowerment Network on Vimeo.
How can care partners access support during the CAR T-cell therapy process? Expert Dr. Amitkumar Mehta discusses the support patients may need during CAR T and resources for accessing patient and family support.
Dr. Amitkumar Mehta is Director of the Lymphoma Program and CAR T Program and Medical Director of the Clinical Trials Office at O’Neal Comprehensive Cancer Center at UAB. Learn more about Dr. Mehta.
See More from The Care Partner Toolkit: CAR T-Cell Therapy
Related Resources:

CAR T-Cell Therapy Care Partners: Tools for Accessing Support |

|

How Is CAR T-Cell Therapy Changing the Myeloma Treatment Landscape? |
Transcript:
Katherine:
What is the role of a care partner of a patient who is undergoing CAR T-cell therapy?
Dr. Mehta:
CAR T-cell therapy is very important therapy and has evolved as a potentially curative therapy in a relapse setting. It does have a downside. And downside, when I say is side effects, which needs to be monitored closely, and it has to be detected early and intervened early, right? Steroids, as well as tocilizumab (Actemra) or anti-IL-6 treatment, are very, very effective in mitigating some of the side effect of CAR T.
But the whole process is very involved, right? You have a patient identified. Then you go through collection. Some people might get some bridging therapy, then chemotherapy, and then they get admitted. Importantly, after the infusion for two months, some of them could have neurological side effect, and that’s why for label and for safety, the patients cannot drive for two months or operate heavy machinery.
So, the whole process requires a good support. In my opinion, when we screen a patient, that “Okay, somebody’s referred to me, or my patient going through a CAR-T process,” how to make sure that they have a caregiver. And caregiver is immensely important, not only for the safety but also moral support for the patient, right?
Katherine:
Yeah.
Dr. Mehta:
And, importantly, what I make sure is that they’re part of the whole discussion. When we sit down and discuss the whole process, side effects, what’s going to happen, they are there.
They know what their loved one is going to go through. So, caregiver support is immensely important. In some patients, unfortunately, they don’t have a caregiver support. For the sake of safety, we might have to give them opportunity to see whether they can actually secure some sort of support. Maybe their distant family member living in a different state and if they can live with them, or their neighbor, or their close friends. If they can bring them to the clinic visit so that we can also discuss with them the whole process. So, caregiver is a very, very important and vital part of the whole process of CAR T.
Best Practices for Finding a Myeloma Specialist
Best Practices for Finding a Myeloma Specialist from Patient Empowerment Network on Vimeo.
Finding a myeloma specialist is imperative to ensure you’re receiving the best care possible. If you’re unsure where to look there are many resources at your disposable. Watch as myeloma patient advocates, Lisa and Sujata discuss their experiences with finding a myeloma specialist and share valuable resources.
See More from START HERE Myeloma
Related Programs:
|

|
Transcript:
Sujata Dutta:
Lisa what would be your experiences or maybe some of your thoughts around best practices around finding a myeloma specialist?
Lisa Hatfield:
Oh yeah. That’s also a really good question. So I live in Boise, Idaho, and most of the people in my support group here have stayed local, which is great, but a couple of people… In fact, at the time I was diagnosed, there was a gentleman who has myeloma, he was in Seattle having a stem cell transplant, he chose to go there because they have a much higher volume of… They do a much higher volume of stem cell transplants, and he just felt comfortable having all of that, not just the doctor, we have good doctors here, they have a huge support staff in Seattle where they do stem cell transplants.
So I asked the group, our group leaders, and then the gentleman who was in Seattle, why do people go somewhere else? Why would they do that? Because it’s not quite as comfortable leaving home for a period of time, and he talked a lot about how he felt just it was a second set of eyes to look at his case and he had some other complications with his myeloma. So for me, the best thing that I did is when I was thinking about going to see a specialist, which we did pretty quickly because my spine was quickly deteriorating, we end up calling MD Anderson, but after that, so we were assigned to a specialist.
She works at MD Anderson and only sees myeloma patients. After that, I wanted to have my stem cells collected somewhere else, and I ended up calling the International Myeloma Foundation their info line, and they actually can provide a list of specialists in your area or help connect you, especially in times of… Now that COVID is starting to settle down, but during COVID, a lot more specialists were doing Zoom calls or telemedicine visits, so I think that they have a really great… For patients who are looking for a specialist, which I assume you also highly recommend because you’re… You’re in a great area for specialist, I’m not. So I would recommend seeking a second opinion from… Not a second opinion, seeking taking a consultation from a specialist, because as you mentioned, myeloma is so nuanced, it is very complex and complicated.
Sujata Dutta:
Yeah and again, this highlights a difference. So I live in Minnesota, and I am blessed to be living here, being diagnosed with MM is not a good thing for anyone. But then being in a place where you have all the resources and the support that you need for dealing with something like myeloma is important, and I’m also in a system which is integrated. So obviously in Minnesota, close to Rochester Mayo. My Cancer Center, Frauenshuh Cancer Center is… It’s in St. Louis Park, and we have University of Minnesota, so these three institutes are integrated and patient information can be shared if needed. So when I was diagnosed, I actually did not have to go look for a hematologist or myeloma specialist.
My diagnosis was done by a hematologist in Frauenshuh cancer center, and then she sent my reports to Mayo to the Hematology Department for a second opinion. So for me, I think I’m so fortunate and they did all of this for me, I didn’t have to do that, and then I was anyways is in the care of an MM specialist, which I think is important. And again, reiterating what he just said is like they really know the disease well enough, like I’m not saying that our regular oncologist who don’t know that, but MM is so nuanced.
If you have the opportunity, I guess you should try and be associated with an mm-specialist, a hematologist, in my case, it was laid out to me on a platter, I should say. I was very fortunate, but for the… I know a lot of people may not have the opportunity to do that, but if you have that, you should definitely try and consider that because it’s quite an important conservation, I think.
Lisa Hatfield:
It is. I think you’re right, I know my current oncologist now, my local oncologist, he is awesome, he’s incredible, he’s a great physician, he was a great diagnostician. He’s really good. My husband, I both really like him. He also appreciates that I go somewhere else. And so that is the one thing I know I was terrified. Asking my doctors, what do you think about me seeing a myeloma specialist. I only had one little bit challenging experience when I told one of the doctors I had seen, I want to go to MD Anderson, and he said, Well, you’ll just be a number there and they don’t do much more than we would do here for that piece of my care, that’s probably true.
And even though we have really great care here and a great medical system, and I feel super fortunate with my cancer, my local cancer center there, all of the staff there is excellent. My oncologist is awesome. I still strongly believe that my course might have been different had I not seen a specialist because it is so unique and every patient is so different, and also specialist have access to some treatments that I did not have access to here locally.
So, I think that that’s super important. I’ll just mention really quick, since we’re talking about specialists, the IMF has their info line, which is… I had to write it down. The phone number is 1-800-452-CURE, which is 2873. So 1800-452-2873, and they can put people… They can direct people to a specialist, and then healthtree.org also has a list if people want to go on, maybe they’re in some dex accelerated insomnia, I guess some night they can go to Healthtree.org, and just… They can click on myeloma, there’s two tabs. Click on myeloma and I just scroll all the way down to patient resources rather than trying to navigate through that. And under patient resources, it says, Find a specialist.
So those are two resources the patients can have, I didn’t look for those, we just called MD Anderson, but I appreciate all your comments, and I think it’s great when people live near a center, I highly recommend going to the bigger center, especially if there’s a myeloma specialist my big fear was just offending my doctors here, and I think some people worry about that too, I’ve talked to other people in our support group.
Lisa Hatfield:
I don’t know if you have any suggestions for that, Sujata, if you think that… I feel strongly now about people seeing specialists, but at the time I was nervous about offending my doctors…
Sujata Dutta:
Yeah, and I can relate to that because you build this relationship, you really then you’re going to see them for however long, and so you really want that relationship to be maintained as it is in a good condition, so I totally understand why you would have hesitated even to think about, Oh my gosh, am I going to offend him her by saying, I want to actually see somebody, and I’m glad that your experience was good, meaning like your doctor was supportive of you actually seeing another one. I have also heard of other patients having to navigate difficult conversations, similar to what you share is like, why do you want to see somebody, like Do you not trust us or in that kind of conversations, which I think is a little bit difficult for the patient because we’re going through a lot anyways.
And I always believe like, this is not just for the patient. The entire family goes through the whole process of diagnosis, treatments, all and everything that ensues. So it’s really difficult for the patient and who’s already going through a lot, and I would really hope that the providers, the doctors understand the state of mind, and agree, if the patient wants to see somebody else to support them in that, in that decision-making, as I say, I have been really fortunate and I had a really good experience, but I have, as you said, None of others who have not had as a pleasant of an experience, I’ve also known of patients who do not have those…
Like you were able to go somewhere else, from Idaho to MD Anderson, I know of some people in some different states who do not have that kind of support, and in fact, they have pretty challenging systems, like there is a person in my support group who lives in Alaska, and for anything, any emergencies, they have to fly down to Seattle.
So, I can only imagine what that must be like to be in that situation where you’re going through so much and then you have to figure out the logistics and the tactical things about how do you reach from point A to point B and then start with whatever procedures so thank you so much for sharing those resources. I think they’re going to be really useful for folks that are listening to this call. Those resources are really, really important. I guess we can also say PEN also has some really amazing resources that folks can leverage as they navigate through this difficult journey.
Lisa Hatfield:
Yeah, I agree with that. And I was going to mention that, so people… When you talk about resources and accessing the resources that that is a big problem, we see that here, because we’re in a more considered more rural area, and so we draw from multiple rural states, our support group does, but also there’s the financial difficulty. So, I’ll just throw that out there too.
Those are two really good resources that I mentioned before, but if people want to reach out to me at PEN or send an email, that would be fine too. I can help direct them to decent resources or some place they could at least start looking for resources because it is really important for people to get that consult from a specialist, I think so… Yeah, I appreciate that.
What Can I Expect During a Bone Marrow Biopsy?
What Can I Expect During a Bone Marrow Biopsy? from Patient Empowerment Network on Vimeo.
Myeloma patient advocates Lisa and Sujata share their experiences with bone marrow biopsies – what to expect and how to prepare.
See More from START HERE Myeloma
Related Programs:

|
Transcript:
Sujata Dutta:
And then there was one more thing that you spoke… When we started with the conversation, BMB. Let’s talk about BMB the dreaded swear word.
Lisa Hatfield:
It is next to dex. I think it’s the second. Maybe it’s equal with Dexamethasone, people talk about dex being the worst thing about myeloma, the BMB, the bone marrow biopsy. Yeah. Did you have one? Right when you were diagnosed?
Sujata Dutta:
Yes, and it wasn’t a pleasant experience. I was obviously, as I mentioned, I had a surgery an emergency surgery, it was pretty… It lasted for six hours and I was wrapped up in all sorts of things, and then I had to have the BMB while I was on an ICU bed, so… Totally not in the best place to start, and it was the first time I was going to have it. So it wasn’t a pleasant experience. It was super painful, they could not sedate me for obvious reasons, because whatever was going on, but post that I had the next BMB, I’ve had a couple… I’m not sure that’s a good thing or a bad thing, the next one, I had it in Mayo and I learned that I could actually be partially sedated and so I wouldn’t feel anything, which was like, Oh my gosh, I thought that was the best discovery mankind had ever made. And ever since then, I’ve always requested for being seated through that process, because otherwise it can be really, really painful, so I don’t know if you want to talk about what the procedure is. I am going to assume some of the folks here have been through this, unfortunately.
Lisa Hatfield:
Yeah, because the bone marrow biopsy is the only way to actually see the myeloma cells, the cancerous plasma cells, it is necessary, it’s also necessary to get it done so they can diagnose the genetic abnormalities, the cytogenetics. But yes, I actually had a little bit different experience. So again, every patient is so different, I prefer not to be sedated because I don’t like sedation, I don’t like the way I feel, I don’t feel good when I have it, so I did have it done and I was… Where I went the first time they didn’t offer sedation, it was, this is 20 minutes, and it wasn’t comfortable.
I will admit that I didn’t like the worst part for me was when they numb the area with lidocaine, they gave you the little shots before they do that, so I’ve had six of them total now, but I’ve had the most recent one. The sixth one I had, they did sedate me and I think it’s conscious sedation, so it’s like you said light sedation, I don’t remember any of it, but I didn’t like it because I had two days of recovery from the anesthesia, so… Yeah, so I think the…
Going back to somebody who’s maybe anticipating it for two nights straight, I couldn’t sleep, I was so nervous about the bone marrow biopsy, I just thought This is going to be so painful. I had excruciating pain in my spine anyway, ’cause it was collapsing as I was going through, I had radiation first, so the bone marrow biopsy didn’t seem to affect me quite as much the first time, but this last time, it seemed to be a little more uncomfortable, especially afterwards, but from my understanding from the bone marrow biopsy, they go in either with the needle, basically the thick needle or where you go to the Mayo Clinic in Scottsdale uses as a drill, and I guess that’s supposed to be faster, and a lot of people think it’s more comfortable, go into the bone marrow and try to take some of that bone marrow out… The soft part of the bone out, they actually take two different samples, but I think the most, uncomfortable part if you’re not sedated, I think is that vacuum-type feeling, and then there’s like a pop… And that was super uncomfortable. I thought that was probably the worst part of not sure if it’s pain or discomfort or what, but I do remember that looking back though, now, every time I’ve had one, I always say that wasn’t so bad.
I remember it, but it wasn’t… I don’t remember it being too bad, so what they do is they will collect enough… They usually have a lab person available as they’re to make sure that they have enough of a sample and the right… The right cells and enough of it, so they usually will only go in once I had one where they had to go back in a second time to try to aspirate some more… The bone marrow, they’ll look at that takes a few days to go through the lab and look at that and see what your genetic abnormalities are with the myeloma cells themselves, and what the volume of cancer cells is in your bone marrow.
But yeah, I just remember, either way, if you’re sedated, you don’t feel it at all while it’s happening, if you’re not sedated, you can feel, especially when they’re numbing it up, the lidocaine shots and that stings, it’s a sting three or four times and takes a little time for it to set in, and then that suction that pop, that’s what was the most uncomfortable, and I think that really the most pain that I felt was the bruise-like pain, the couple of days afterwards, they’re not walking, but just sitting on it is bandaged up really…
Well, you can’t take a shower for a day, but when I would go to sit on it, it just got bruised, but… Yeah, the bone marrow biopsy, nobody looks forward to those… It’s nice to know that there is something in the works, even mass spec testing, which isn’t quite as sensitive… It’s nice to know that there’s something that works, to maybe look at other ways to test for the myeloma. Yeah, not fun. It’s a necessary thing though that when people are diagnosed with multiple myeloma.
Sujata Dutta:
That’s absolutely the true statement. I don’t like it at all. I am also anxious before I have my… I’ve had four now, so… And every year I’ll have to have one, so I know that that’s a necessity, as you said, I do feel anxious, but I keep telling myself this is needed to assess overall disease involvement and hopefully the results are better than last year, so I kind of… That’s how I sort of create some positive energy around that experience because it’s not a pleasant experience, and as you said, it does hurt for a couple of days after I actually have… Sometimes it goes on for a week that I have, or discomfort, but again, each to his own people might have different experiences, but I think the more we talk about it, the more we hear other people’s experiences, we might just feel like, Hey, mine was not all that bad, I look at her, him, what they’ve gone through and things like that, or even just thinking like… It’s different, it’s nuance.
Everybody goes through different experiences like you prefer not being seated, I prefer being sedated, so it depends on each one’s experiences, but the bottom line is there are options available, everybody understands, it’s a difficult procedure, everybody understands it’s not pleasant, nobody wants to put the pain through that if they had a choice.
Right now, we don’t have one, so I think just thinking about in a positive way and embracing it, I guess might just help, it helps me, so I’m hoping that it helps others as well, just changing the perspective a little bit.
Lisa Hatfield:
Yes, so who does your bone marrow biopsies? I’ve been to… Sometimes a nurse practitioner does them and sometimes an RN does mine, and I know some of our local doctors do them, oncologists do them, what type of professional does your bone marrow biopsies?
Sujata Dutta:
With Mayo, I’ve had it twice there, they have specialists, they have a whole team that does obviously Mayo, they do like MM treatments, like they have 500 patients doing biopsies every year. That’s what I heard. I had mine there too, so it’s a well-oiled machine, they just have departments for every little thing, so that’s different, but even when I do it with my local cancer center, they have a specialized team, so it’s not the nurses, there’s a specialized team. There’s a different procedure.
Again, it’s different to how Mayo does it. When I do it at my cancer center, they actually do a scan before I have a BMB, and to make sure that they’re going in the right place. Which I thought like Wow, that’s great. Just as a second level of precision, but yes, that’s different to Mayo, but it’s always like a specialist doing it for me.
Lisa Hatfield:
Yeah, and then how often do you have to have those on a regular basis, like annually or just as things change with treatment?
Sujata Dutta:
Annually. So, only just… Obviously, for my diagnosis I had that and then six months later, and I had a stem cell transplant and I did a BMB prior as well then, a couple of months after I did that again. So that was the only time and it happened more regularly, but since then it’s been like yearly.
Lisa Hatfield:
Yeah Okay. Yeah, the bone marrow biopsy is interesting because I know a lot of… There’s different ways that they test that and now they have a more sensitive test, so everybody has different..That’s the other part of alphabet soup. Some people have something called flow cytometry or NGF or NGS. So anyway, yeah, it’s kind of interesting that everybody will have different ways of going through that or different experiences, so anybody who has questions, you’re welcome to reach out to me at PEN or any of the other resources that are out there.
How to Approach the “Alphabet Soup” of Myeloma Treatment
How Do I Navigate the Myeloma Alphabet Soup? from Patient Empowerment Network on Vimeo.
After an initial myeloma diagnosis, you’re plagued with various acronyms referring to treatment, different mutations, and much more. Hear from myeloma patient advocates, Lisa and Sujata, as they break down how they’ve navigated and continue to navigate through what they deem the “alphabet soup” of myeloma treatment.
See More from START HERE Myeloma
Related Programs:

|
|
Transcript:
Lisa Hatfield:
Hi, my name is Lisa Hatfield, and I’m a myeloma patient. I was diagnosed back in 2018. I am an Empowerment Lead at Patient Empowerment Network, and one of the things that we are frequently asked is, What are all of these letters and acronyms when you’re diagnosed with myeloma? So just a nutshell, this is why myeloma is so complicated and confusing based on my story. So, I was diagnosed, like I said back in 2018, I have kappa light chain only myeloma. When I was a newly diagnosed myeloma patient, which is MDMM versus RRMM, which is relapsed/refractory multiple myeloma patient, I have kappa light chain only myeloma.
I have…and I’m just going to spew out all of my letters and numbers, I have translocation 11, 14, I have monosomy 13, I don’t have an M spike, which means all of my antibodies are normal, my IgM IGA, IGG are normal. After a surgery and radiation, I went through six months of KRD, followed by another three years of just the R, which is Revlimid, every month I have…in addition to my myeloma labs, I have a CBC, a CMP. Every year I have something called a BMB, bone marrow biopsy. I have a PET CT and MRI every year, and then I do something with my bone marrow biopsy to check for something called MRD status by NGS, which is currently, I’m MRD positive at 10 to the minus 6. So, all of those letters, it’s just a big alphabet soup for people to try to understand myeloma, it gets really, really confusing.
One of the things as a myeloma patient that I recommend to people is the IMF, The International Myeloma Foundation, just to add a few more letters to it, you can look at their website at myeloma.org. They break down each of these phrases and words and letters and acronyms and whatnot.
So newly diagnosed patients and patients who have had myeloma for a while can understand all of these letters and all of these numbers and what these genetic mutations mean and what the tests mean. So, I guess, Sujata, I know you’ve been through this too. We’re just having conversation. How did you…when you were first diagnosed, I’m curious too, and for other patients, how did you get through all of the letters and things being thrown out at you.
Sujata Dutta:
Yeah, Lisa, this is funny. So, my name is Sujata Dutta, I’m a board member at the Patient Empowerment Network, and I’m also an MM patient. I was diagnosed with multiple myeloma in December of 2019. And Lisa, you summed it up really well. This alphabet soup is actually a real thing. The first time when I got to know about it, I actually, obviously, like many, many folks that I have known that are on this journey, it comes up as a surprise, it just is… For me, it was interception, I can actually say that word and spell it, I think, but at the time when I was diagnosed, I had no clue what the doctor was talking about, I had this massive inflammation of my lymph nodes and I had to have emergency surgery ’cause the lymph nodes had caused damage to my big intestine, and then we did some research, we as in the doctors, and after a week post-that surgery, I was diagnosed with multiple myeloma. Again, I can say that today, but when they told me about multiple myeloma, I’m like, I have no clue what you’re talking about. They had literally had to dumb it down and say this is a kind of a blood cancer…
I’m like, oh cancer all right then. So, the alphabet soup is actually a real thing, I do have M-spike Lisa, unlike you. My kappa light chains are fine, but it’s been a long journey and not there yet, so still…my goal is to achieve MRD or remission. I’m not there yet, I still have involvement through my proteins, not so much in the bones, so let’s break that down a little bit, Lisa.
Let’s talk about that alphabet soup and how do you navigate that through as a new patient, I would say not even a new patient, like an existing patient like me, sometimes I’m like baffled, like, “Oh, my gosh, what is this report saying to me?” So, thanks for sharing that resource about IMF but what else…as you started, just think about those early days, weeks when you were diagnosed and all of these terms were thrown at you, how did that feel, and how did you overcome some of it, if not all?
Lisa Hatfield:
That’s a good question. So, I went in to see my, my local oncologist here, after I’d gone through radiation surgery down at MD Anderson because I was going to have my chemo here, and in his office, there was a poster up for a local myeloma support group, which I was not excited about, I thought, Well, maybe I’ll go, but I don’t want to…I already feel down enough that I’ve already overwhelmed enough with my diagnosis, but we just…I called the lady, her name is Sheri, called her up, we talked about myeloma, she had myeloma for seven years, and I was super inspired by that, so we showed up, I had a walker I and walk with a walker because of all the damage to my spine and showed up limping along with my walker, and everyone there was talking about, “Oh, you’re newly diagnosed, what is your M-spike?” That was something new that I hadn’t heard, and I hadn’t had that discussion with my doctor, I didn’t realize at that time, it was because I did not have an M-spike.
So I think, like you said, it’s overwhelming enough to just receive that diagnosis and in my mind, I remember thinking back, Okay, if I talk to a new patient, if I can get through this and make it a few years out, what are the things that were the most confusing to me, and I think understanding the type of myeloma, if I were to…
If patients were to ask me, understanding the type of myeloma patient has, the genetic mutations and understanding what their M-spike is or is not, if they are just…if they’re a light chain, only if they have light chain only disease. Those would be the things I think, because it is so confusing to patients in them, I think as they go along, maybe they can ask their team, “Well, what does that mean? Or what do those letters mean?” Yeah, it’s okay to ask those questions.
Sujata Dutta:
Absolutely. Ask as many questions as you can, you’re encouraged as a patient to ask questions or at least I was. I think what is also important to note is like with MM, it’s an individual, it’s a very individualized sort of a disease, so although we put it under the bucket of multiple myeloma, everybody experiences it differently, they even have reactions to medication very different, like just yesterday I was talking to somebody in my support group and they had a really different experience with one of the drugs that I take regularly, daratumumab (Darzalex) every four weeks. She just had the first dose and it was such a bad reaction, she ended up in ER.
So not scaring anybody, I’m just saying everybody has different reactions, somebody might take to some medication really well versus others may not…and just between the two of us, we have different types, you don’t have that, and so there are these nuances, which I think it’s just important to acknowledge, there’s nothing to be scared of…it’s just acknowledging the difference of how multiple myeloma works versus some other cancers maybe…I think it’s important. And you brought up a good point about trying to understand the labs, we don’t have to be experts.
I don’t think I want to be an expert. I have folks that are experts that will take care of me, but just so that I understand the basics of it, and then I’m able to ask questions for my own self, like educating myself.



