Tag Archive for: thyroid cancer patient
Bridging Gaps in Care and Empowering Patients Facing Thyroid Cancer
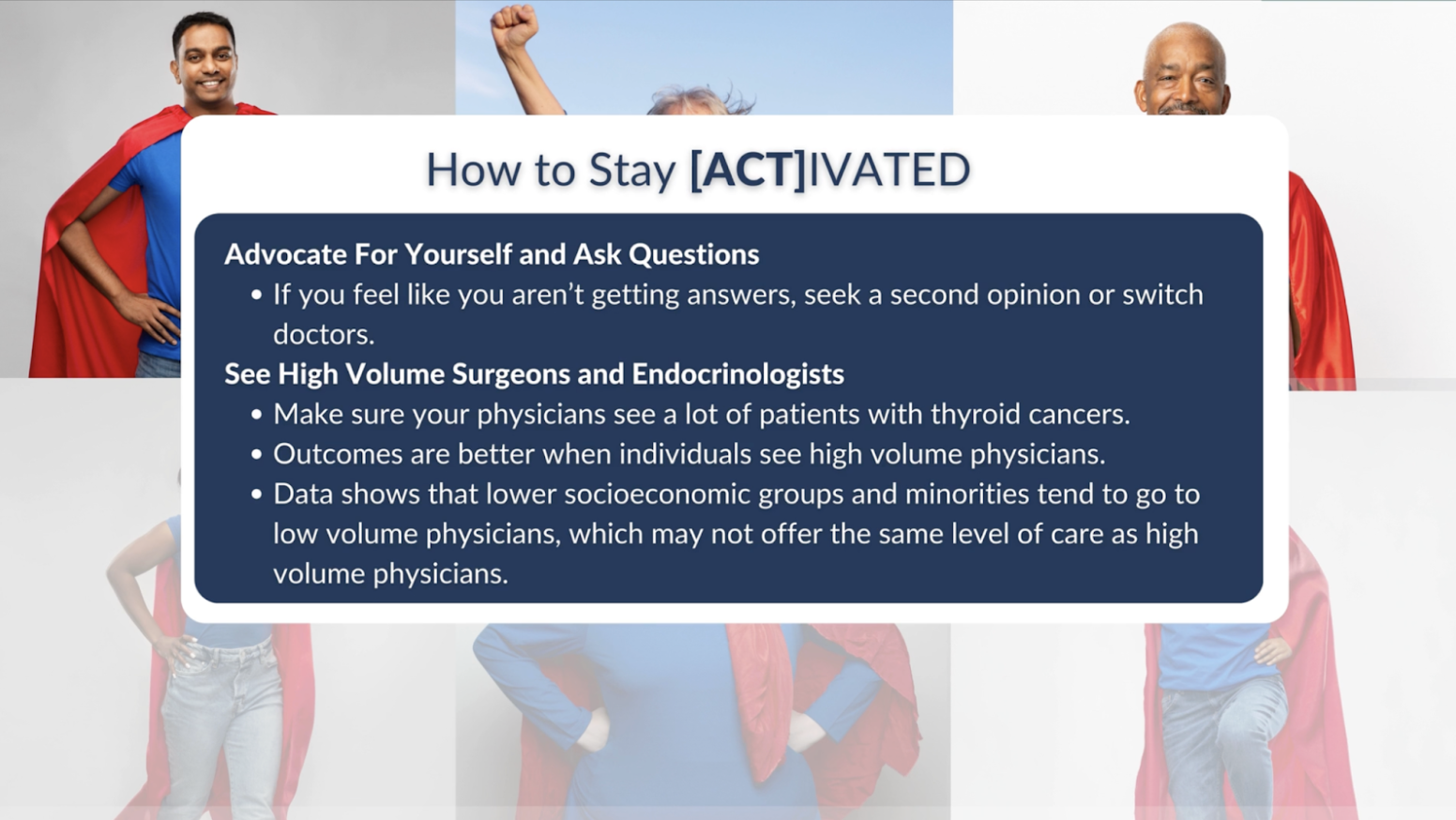
Patient Empowerment Network (PEN) is dedicated to helping educate and empower patients and care partners in the thyroid cancer community. Thyroid cancer research and treatment options are ever-changing, and it’s vital for patients and families to educate themselves about clinical trials, treatment advancements, barriers to and disparities in care. With this goal in mind, PEN introduced the [ACT]IVATED Thyroid Cancer program, which aims to inform, empower, and engage patients to stay updated about the latest in thyroid cancer care.
Thyroid cancer awareness needs more visibility for multiple reasons. Thyroid cancer incidence is higher in women with 70 to 75 percent of cases occurring in women. And many patients may not be aware that thyroid cancer is the most common cancer in patients who are age 15 through age 33.
PEN is pleased to add information about thyroid cancer to educate more patients and their families. Cancer survivor Lisa Hatfield interviewed expert Dr. Megan Haymart from the University of Michigan as part of the [ACT]IVATED Thyroid Cancer program.

Thyroid Cancer Disparities and Challenges
Thyroid cancer patients may be impacted by a variety of disparities in incidence, diagnosis, and care. Raising awareness about these disparities can help patients and patient advocates work toward closing disparity gaps. Dr. Megan Haymart discussed the thyroid cancer gender disparity that impacts more women than men. “So about 70 to 75 percent of all thyroid cancer cases occur in women. And this is very similar to other endocrine diseases, especially other thyroid conditions. So hypothyroidism, hyperthyroidism, those are also more common in women. And so we think that the reason for this is probably multifactorial. So one, there’s probably something about thyroid conditions in a biologic level that differs between men and women.”
Thyroid cancer patients may be affected by socioeconomic barriers to care. Dr. Megan Haymart discussed potential barriers to optimal care. “And there’s strong data for thyroid cancer and other cancers as well, that sometimes what’s happening is individuals who are lower socioeconomic status or a minority race or ethnicity are sometimes clustering at low volume hospitals. And so they may not be getting the best care because of where they’re going.”
Socioeconomic impacts on thyroid cancer extend to other disparities too. Dr. Megan Haymart shared about a difference that often goes along with socioeconomic status. “And then related to socioeconomic status, we also know that there can be differences based on education level as well.”
Thyroid cancer may feel more overwhelming for young patients. Dr. Megan Haymart shared the different types of stress that young thyroid cancer patients may feel. “…it’s very stressful especially for younger patients who are at a transition point in their life, related to college, related to starting new jobs, related to starting a family, all their friends are healthy and they get a cancer diagnosis, it can be very stressful and overwhelming. And so if you’re worried, if you’re stressed, that’s normal. Patients shouldn’t feel bad about that. No one should make them feel bad about it.”
Thyroid Cancer Care Solutions and Successes
Thyroid cancer care is changing and becoming more personalized to each patient and their preferences for treatment. Dr. Megan Haymart discussed how she’s encouraged about the future of thyroid cancer treatment. “…one that I’m the most excited about with the guidelines is the guidelines are going to emphasize tailored care more and shared decision-making more. And so I think these are key. And so for a lot of thyroid cancer management, there is not one right or wrong treatment option. It depends a little bit on the patient and what their preferences are.”
For thyroid cancer patients, it’s important to see care providers who diagnose and treat a high number of patients with thyroid cancer. Dr. Megan Haymart shared her advice. “…if you feel that you’re not getting the answers that you want, don’t be afraid to get a second opinion…make sure that you’re seeing high volume physicians who see a lot of patients with thyroid cancer. This is for both the surgeons and the endocrinologists, because we know that outcomes are better when individuals see high volume physicians. “
It’s also important for thyroid cancer patients to be comfortable with the care provider and that the provider is truly listening to them. Dr. Megan Haymart shared her expert advice. “…if patients feel like they’re being dismissed, if they’re anxious, if they’re worried, if they’re stressed, if they feel like their questions aren’t being answered, you can always get a second opinion or see someone else.”
Switching to a different thyroid cancer care provider isn’t necessarily as complicated as some patients might think. Dr. Megan Haymart discussed the importance of patients advocating for themselves. “And so I think it’s very important to advocate for yourself and don’t be afraid to look around. And if the center that’s closest to you isn’t the best center for thyroid cancer, and if there’s a better one that’s 30 minutes away, and you’re capable of getting there, I would encourage you to go.”
Delving deeper into the patient experience, PEN’s Thyroid Cancer Empowerment Lead Carly Flumer was diagnosed at the age of 27. And though she experienced many challenges through her cancer journey and still does as a survivor, Carly has also discovered new passions as a result of her experience. “…there have many silver linings of having cancer. I found my passion in helping other cancer patients through different avenues, I’ve made friends and joined communities of people who “get it,” and I found new strength in who I am as a person.” Learn more and connect with Carly here.
[ACT]IVATED Thyroid Cancer Program Resources
The [ACT]IVATED Thyroid Cancer program series takes a three-part approach to inform, empower, and engage both the overall thyroid cancer community and thyroid cancer patient groups who experience health disparities. The series includes the following resources:
Though there are thyroid cancer disparities, patients and care partners can be proactive in educating themselves to help work toward optimal care. We hope you can take advantage of these valuable resources to aid in your thyroid cancer care for yourself or for your loved one.
Thyroid Cancer Patient Profile: Beena Patel
As Beena Patel shares the story of her thyroid cancer journey and path to becoming an integrative medicine professional personified, it becomes clear that she’s making a positive impact to many patients and to those seeking wellness. In her professional life, she works as an oncology physician assistant, holistic life & health coach, yoga teacher, and energy healer. Beena shares the initial feeling that sparked her passion for patient empowerment, “I felt like I’m meant to do this. And I had even more of a fire in me, like I’m going to help people, and I’m going to help cancer patients feel empowered over their care.”
Beena’s cancer journey began when she was 21 and in Montreal celebrating post-college accomplishments with a group of friends. They were mainly driving to festivities and eating a lot of food. She felt like she must have gained 5 pounds, but found that she had actually lost 5 pounds after she was back home. She was in physician assistant school at the time and told her doctor about her weight loss, which prompted her to check her neck and thyroid. Her doctor said her thyroid felt palpable and decided to do further hormone testing, radiological testing, and an ultrasound. Something abnormal was found in the testing, which was followed up with a biopsy that confirmed diagnosis of thyroid cancer. Beena was shocked with her diagnosis at such a young age and felt unsettled with the timing for it to happen when she had just started physician assistant training.
Traveling back and forth between her doctor’s office and the hospital felt overwhelming for Beena. “It was a lot for a young woman and a woman of color, to see not only how painful it is to go through any type of diagnosis, let alone cancer, and having to feel so alone throughout the process. Also seeing how people do pass you off when you’re a young woman of color, and I would say a woman of any age, but I think women who are younger, trying to navigate life, and figuring out your path. And then you get a diagnosis and you’re like, ‘No one understands me,’ so it was a lot to handle.”
Beena’s thyroid cancer treatment included a total thyroidectomy to remove her entire thyroid gland. Her care team also tested some lymph nodes at that time, but didn’t find anything concerning. “I didn’t get radioactive iodine, but then three years later, I did have a mild recurrence, so they did do radioactive iodine at that time.” Beena is now doing well and takes thyroid replacement therapy to maintain her metabolism and other thyroid-related processes.
Empowering herself has been a vital piece of Beena’s patient journey. She felt like her first doctor on her cancer journey wasn’t really listening to her, so she found a different doctor. “You have to find the right fit. It’s like dating. Don’t settle until you feel like you not only have the scientific background, but the right doctor who has clinical expertise, who you feel has clinical knowledge and compassion, as well as the time to spend with you and to educate you as a patient. Your doctor should make you feel seen, heard, and understood. It’s a relationship that you’re creating with this provider, so it’s very important to find a good fit.” She also feels patient resources like NIH.gov, clinicaltrials.gov, and the Patient Empowerment Network (PEN) website are valuable in the process of patient education and empowerment.
Beena had to start physician assistant school a second time after her cancer became too disruptive, and she felt she became empowered at that time. She went through a difficult breakup about 6 months earlier and was feeling disconnected from her body. Yoga and meditation helped her cope with stress, but she was looking for something deeper. She found a Reiki practitioner in New York City and received a treatment for the first time. “I just felt like I transcended everything that I’d gone through in the last decade. I just felt good and calm and at peace. And so when I felt that, I knew I had to share that with patients, I knew there was something deeper.” After she was at Columbia University Irving Cancer Research Center for a few months, Beena had already started doing patient consultations with integrative medicine, and her patients were very responsive to the consultations.
“Many patients aren’t aware of Reiki, or they don’t know that yoga is available to them, but I started doing consultations to educate them. They were willing to try something new, since we weren’t replacing the medication.” Beena realized that she had a gift with patients as she was able to bring peace when they were stressed or had a panicked look on their face. She also recalls during her cancer journey that a medical fellow actually lied to her about the diagnosis and seemed uncomfortable in telling Beena the actual diagnosis. “Some people don’t know how to be comfortable with emotions, because they weren’t taught emotional intelligence. And so I learned that when I would go into the room with a patient, I would hold it together even when I didn’t know what I was doing.”
Beena would request that someone else accompany her in the room, like another provider who was more experienced. She would maintain her calmness and return to her center, and she attributed that ability to her daily meditation practice. She would tell the patient to take a deep breath, and she could watch their heart rate decreasing in real time. The patients would become calmer. “So even if there was an emergency, I could hold it until the intensive care unit (ICU) or someone from another department came in to check on the patient, and it’s like we have that power to help people just by being emotionally and mentally balanced.” And when Beena went to Memorial Sloan Kettering Cancer Center, they were more supportive of integrative medicine. “Music therapists would come, and they had yoga nidra (yogic or psychic sleep) at nighttime and Reiki. They had a patient population that was more aware and educated about integrative medicine, so they would ask for it.”
Patients would request to do a technique like yoga or breath work before they went for radiation treatment in the hopes that it could eliminate the need for anxiety medication. “Sometimes it would work and other times it wouldn’t. Some would pass out at their radiation treatment. So we adjusted things to a combination of breath work and meditation and decreased the anxiety medication dosage. Patients loved having that ability to manage their care from an empowered standpoint.” Beena would also run the integrative medication combination by the care team to keep them informed about the patient.
Integrative medicine is at Beena’s core of medical values that use a mixture of Western and Eastern medicine techniques. She helps patients understand the energetic root of the issues that are happening in the body. “I do think in the future there could be more Eastern philosophies, I think we could get back to energy healing and understanding root causes, the ancient medicine that was passed on from our ancestors.”
Beena is grateful that she is feeling healthy and for the different ways that she’s able to help patients. As for her other advice for cancer patients, she recommends advocating for yourself for the sake of your health. “Be open to ask for support. It’s your body and your health. And be open to us for support, be open to ask when you don’t understand something, and let us know about any supplements that you take. If you feel like you don’t have a good relationship with your healthcare team, be willing to do empowered research and go to the person who you feel comfortable with and who you feel understands you.”
Navigating Thyroid Cancer: Tips from Someone Who’s Been There
So you’ve been diagnosed with the “C” word, specifically thyroid cancer, and now you’re seeing a whole new care team. This usually includes an endocrinologist who specializes in disorders of the endocrine system, including the thyroid. As a patient who has been living with thyroid cancer on and off for the past 5 years, here is a non-exhaustive list of tips about treatment and how to manage, including questions to ask your care team and tips for your appointments as you go along your own cancer journey.
11 Tips for Navigating Thyroid Cancer
- Have a good relationship with your endocrinologist, as they will be treating you for life.
- Make sure your values, morals, and opinions are respected as part of the treatment process. The cure isn’t the only part of the cancer journey.
- Ask about different treatment options (i.e. surgical removal).
- Inquire about potential side effects of each treatment and how to mitigate them, especially if you undergo chemotherapy and/or radiation.
- Ask for clarity on medical jargon, such as thyroid-specific blood tests.
- Bring in a list of questions to each appointment.
- If possible, have a caregiver, such as a family member or friend, come with you to each appointment as a second set of eyes and ears.
- Join support groups that are available both online and in-person.
- Utilize your patient portal, if you have one, for messaging your care team, renewing prescriptions, and viewing lab and ultrasound results.
- If you end up having to take synthroid, keep a diary or log of how you feel at each dose to be able to report back to your care team.
- Advocate for yourself if something doesn’t feel right.
As a patient in a new and very unique environment with a disease you never thought you would get, knowing how to navigate this beautiful, yet terrifying journey is hard. However, if you stick to your values, ask questions, create a strong relationship with your care team, and advocate for yourself, it’ll make the process a lot smoother.
Carly Flumer is a young woman who was diagnosed with stage I papillary thyroid cancer at the age of 27. She recently received her Master’s degree from Boston University in Health Communication and received her Bachelor’s from George Mason University in Health Administration and Policy. While being diagnosed with the “C” word at such a young age was a surprise, as it would be to anyone, she found strength, support, and inspiration in sharing her cancer journey on social media. As a result of her health outcome, she looks to advocate for other cancer patients through education, research, and health literacy.
“Wait, There’s a Good Cancer?”
When the Luck of the Draw Leads to the Short End of the Stick
Cancer is one of the most feared diseases. Everyone is affected by it in some way, but no one really imagines getting it themselves. So imagine hearing that you got the “good” cancer, a commonly used term for thyroid cancer. That can’t be right. Cancer is cancer…isn’t it? But who are we, as patients, to question what our doctors tell us? They’re the ones who went to medical school and have years of training. But maybe thyroid cancer isn’t that bad?
That’s what I thought when I was told that my cancer was the “good” one by more than one doctor. In fact, one doctor told me that thyroid cancer was “the cancer to have if you had to get it.” I didn’t have any symptoms at the time, so I took these words, spoken to me by medical professionals, as truth. Unfortunately, I learned that there was no such thing as a “good” cancer once I began treatment.
While thyroid cancer is slow-growing, does have a very good prognosis, and can be easily treatable, no cancer is the same. For example, I had the papillary variant of thyroid cancer, a common diagnosis amongst most thyroid cancer patients. I underwent surgery to remove half of the thyroid with the tumor, but my treatment didn’t end there. It was discovered in the pathology report that I had metastasis that was not shown on the original ultrasound that showed the tumor in my thyroid. As a result, I had to undergo a second surgery for the removal of the remaining half of my thyroid. Additionally, I was told by my surgeon that, because of the metastasis, he didn’t know if cancer could be elsewhere in my body, and I would need to undergo oral radiation therapy. “Wasn’t this the ‘good’ cancer?” I thought over and over.
Furthermore, what doctors don’t explain, at least very well in my case, is what not having a thyroid is going to be like. I wasn’t aware of what a thyroid was nor its functions when I was told that it was harboring a tumor. Nor did I know until I had to be placed on a supplement, or rather a replacement, for my lack of thyroid. I learned quickly that the thyroid essentially interacts with every other system in the body through controlling metabolism, heart rate, temperature, energy level, etc. My body slowly adjusted to this new medication with a prescribed dose that was initially “simply a guess” based on my age, weight, and overall health. From there, my healthcare team and I adjust the dose based on how my body responds. If I think about this, especially as a woman, my body goes through many changes as I age, and I’m sure many of them are affected by a properly-functioning thyroid, which I no longer have. I’m not saying that I’m not eternally grateful for their actually being a supplement I can take to, quite literally, live, on a daily basis. What I am saying is that the stigma and the choice of words and phrases surrounding this cancer, perpetuated by medical professionals needs to stop. At the very least, they need to recognize thyroid cancer as a cancer, a diagnosis that inevitably impacts the life, good or bad, of every patient who has this terrible disease well into survivorship.
If you’re a thyroid cancer patient, whether newly-diagnosed, in treatment, no evidence of disease (NED), or anywhere in between, educate and advocate for yourselves. Find doctors who take the time to understand your wants and needs as an individual human being. Never think that your cancer is “less than,” because it matters.
Carly Flumer is a young woman who was diagnosed with stage I papillary thyroid cancer at the age of 27. She recently received her Master’s degree from Boston University in Health Communication and received her Bachelor’s from George Mason University in Health Administration and Policy. While being diagnosed with the “C” word at such a young age was a surprise, as it would be to anyone, she found strength, support, and inspiration in sharing her cancer journey on social media. As a result of her health outcome, she looks to advocate for other cancer patients through education, research, and health literacy.
Thyroid Cancer Glossary of Terms
Thyroid Conditions
Hyperthyroidism – A condition that occurs when the thyroid gland makes more thyroid hormones than the body needs. Thyroid hormones control the way the body uses energy and affect the body’s metabolism. Signs and symptoms include weight loss, fatigue, rapid or irregular heartbeat, sweating, diarrhea, nervousness, mood swings, shaky hands, trouble sleeping, trouble tolerating heat, muscle weakness, and a goiter (an enlarged thyroid gland that may cause the bottom of the neck to look swollen). Also called overactive thyroid.
Hypothyroidism – Too little thyroid hormone. Symptoms include weight gain, constipation, dry skin, and sensitivity to the cold. Also called under active thyroid
Types of Thyroid Cancer
Anaplastic Thyroid Cancer – a rare, aggressive type of thyroid cancer in which the malignant (cancer) cells look very different from normal thyroid cells
Follicular Thyroid Cancer – cancer that forms in follicular cells in the thyroid. It grows slowly and is highly treatable. The cancer cells look and act in some respects like normal thyroid cells
Medullary Thyroid Cancer – cancer that develops in C cells of the thyroid. The C cells make a hormone (calcitonin) that helps maintain a healthy level of calcium in the blood
Papillary Thyroid Cancer – cancer that forms in follicular cells in the thyroid and grows in small finger-like shapes. It is the most common type of thyroid cancer. The cancer cells look and act in some respects like normal thyroid cells. Variants include:
- Columnar cell
- Cribiform-Morular
- Diffuse sclerosing
- Encapsulated
- Follicular variant of papillary
- Hobnail
- Hürthle cell
- Insular
- Macrofollicular
- Oncocytic
- Solid/trabecular
- Spindle cell
- Tall cell
- Warthin-Like
Poorly Differentiated Thyroid Cancer – a rare form of thyroid cancer that is often aggressive. It is associated with high risk of cancer recurrence, spread to lung and/or bones and increased risk of death. Patients are often treated with a combination of surgery, radioactive iodine and/or radiation therapy and possibly newer, molecular targeted therapies
Thyroid Cancer Terms to Know
Adenocarcinoma – Cancer that begins in glandular cells. Glandular cells are found in tissue that lines certain internal organs and makes and releases substances in the body, such as mucus, digestive juices, or other fluids
Advanced – Has spread to other places in the body; far along in course
Benign – Not cancerous. Benign tumors may grow larger but do not spread to other parts of the body. Also called non-malignant
Lobe – a portion of an organ (ex. thyroid)
Lobectomy – surgery to remove a whole lobe (section) of an organ (ex. thyroid)
Locally Advanced – has spread to nearby tissues or lymph nodes
Malignant – Cancerous. Malignant cells can invade and destroy nearby tissue and spread to other parts of the body
Metastatic – spread of cancer from the primary site (place where it started) to other places in the body
Neoplasm – An abnormal mass of tissue that results when cells divide more than they should or do not die when they should. Neoplasms may be benign (not cancer), or malignant (cancer). Also called tumor
Nodule – A growth or lump that may be malignant (cancer) or benign (not cancer)
Partial Lobectomy – surgery to remove a whole organ (ex. thyroid)
Radioactive Iodine – a radioactive form of iodine, often used for imaging tests or to treat an overactive thyroid, thyroid cancer, and certain other cancers. For imaging tests, the patient takes a small dose of radioactive iodine that collects in thyroid cells and certain kinds of tumors and can be detected by a scanner. To treat thyroid cancer, the patient takes a large dose of radioactive iodine, which kills thyroid cells. Radioactive iodine is given by mouth as a liquid or in capsules, by infusion, or sealed in seeds, which are placed in or near the tumor to kill cancer cells
Recurrent – Cancer that has recurred (come back), usually after a period of time during which the cancer could not be detected. The cancer may come back to the same place as the original (primary) tumor or to another place in the body. Also called recurrence and relapse
Refractory – Cancer that does not respond to treatment. The cancer may be resistant at the beginning of treatment or it may become resistant during treatment. Also called resistant cancer
Risk – patients with differentiated thyroid cancer (papillary or follicular) have different levels of risk of a recurrence or of persistent disease
- Low Risk of recurrence or persistent disease means: no cancer in nearby tissue or outside the thyroid bed other than 5 or fewer small involved lymph nodes (under 0.2 centimeters), and cancer that is not one of the variants.
- Intermediate Risk (Medium Risk) means some tumor in nearby neck tissue at the time of surgery, more than 5 lymph node metastases 0.2 to 3 centimeters in size, or a tumor that’s a variant or has vascular invasion
- High Risk means extensive tumor outside the thyroid, distant metastases, incomplete tumor removal, or a cancerous lymph node over 3 centimeters in size.
T3 – also called triiodothyronine; a type of thyroid hormone
T4 – also called thyroxin and thyroxine; a hormone that is made by the thyroid gland and contains iodine. T4 increases the rate of chemical reactions in cells and helps control growth and development. T4 can also be made in the laboratory and is used to treat thyroid disorders
Thyroglobulin – the form that thyroid hormone takes when stored in the cells of the thyroid. Doctors measure thyroglobulin level in blood to detect thyroid cancer cells that remain in the body after treatment. If the thyroid has been removed, thyroglobulin should not show up on a blood test. Some patients produce anti-thyroglobulin antibodies, which are not harmful but which mask the reliability of the thyroglobulin value
Thyroid Gland – a gland located beneath the larynx (voice box) that makes thyroid hormone and calcitonin. The thyroid helps regulate growth and metabolism. Also called thyroid gland
Thyroid Gland Squamous Cell Carcinoma – A rapidly growing primary carcinoma of the thyroid gland composed of malignant squamous cells (cells are found in the tissues that form the surface of the skin, the passages of the respiratory and digestive tracts, and the lining of the hollow organs of the body). The clinical course is usually aggressive
Stage – The extent of a cancer in the body. Staging is usually based on the size of the tumor, whether lymph nodes contain cancer, and whether the cancer has spread from the original site to other parts of the body
Unresectable – Unable to be removed with surgery
Sources:
cancer.gov
Carly Flumer is a young woman who was diagnosed with stage I papillary thyroid cancer at the age of 27. She recently received her Master’s degree from Boston University in Health Communication and received her Bachelor’s from George Mason University in Health Administration and Policy. While being diagnosed with the “C” word at such a young age was a surprise, as it would be to anyone, she found strength, support, and inspiration in sharing her cancer journey on social media. As a result of her health outcome, she looks to advocate for other cancer patients through education, research, and health literacy.
Cancer: The Scariest Ride of Them All
June is home to National Cancer Survivors Day (June 7th), a day to celebrate the journey of survivors, who are defined as “patients diagnosed with cancer.” While there are multiple resources for cancers patients, including an entire website dedicated to the National day, I thought that I would share my perspective of what it means to be a patient/survivor on an emotional/mental level:
Emotional/Mental
- Sadness and in denial when diagnosed
- Angry that this is happening to you specifically
- Hopeless because of a lack of control
- Frustration when you don’t understand your treatment plan
- Guilt knowing other cancer patients have it worse
- Anxiety when preparing for a scan or an appointment
- Betrayal when you find out who your true friends and family are
- Hope knowing you may make it out on the other side
- Strong when you make it through the next chemo and/or radiation treatment
- Resilient when you’re declared “in remission”
- Fear that the cancer may come back
This is only a glimpse into the many feelings felt, the life that is suddenly a roller coaster with ups and downs and hidden twists and turns. Sometimes you may not hear the whole story, the emotions guarded underneath a face that tries to “be strong” through it all. Really take a listen when you, as a caregiver, a medical professional, a friend, or a family member, ask a cancer patient, “How are you feeling?” Look at the facial expressions, the body language, and the words they’re using. To summarize: Be present.
Carly Flumer is a young woman who was diagnosed with stage I papillary thyroid cancer at the age of 27. She recently received her Master’s degree from Boston University in Health Communication and received her Bachelor’s from George Mason University in Health Administration and Policy. While being diagnosed with the “C” word at such a young age was a surprise, as it would be to anyone, she found strength, support, and inspiration in sharing her cancer journey on social media. As a result of her health outcome, she looks to advocate for other cancer patients through education, research, and health literacy.



