Expert Advice | Strategies for Managing MPN-Related Fatigue
Expert Advice | Strategies for Managing MPN-Related Fatigue from Patient Empowerment Network on Vimeo.
Fatigue related to myeloproliferative neoplasms (MPNs) can be overwhelming and may have an impact on other parts of your life. So, what can be done about it? MPN specialist Dr. Naveen Pemmaraju shares advice for understanding and managing this common symptom, including lifestyle choices that may be beneficial.
Dr. Naveen Pemmaraju is Director of the Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN) Program in the Department of Leukemia at The University of Texas MD Anderson Cancer Center. Learn more about Dr. Pemmaraju.
Related Programs:
Transcript:
Katherine Banwell:
Well, it’s obvious that there’s some symptom overlap along with this. And so I’m wondering what the strategies are for managing these. Let’s start with fatigue first.
Dr. Pemmaraju:
Let’s do that.
Katherine Banwell:
How do you manage that?
Dr. Pemmaraju:
This is one of the tougher parts of what we do. I’m glad you’re pinning me down to say it, because really this is the majority of what we need to be talking about in the clinic. I’m going to just be honest, you know, with all the scientific breakthroughs and everything, some of these are limited. The fatigue, this is some of the strategies I use and some of the experts in the field. I think one is managing the underlying disease. So, as you mentioned, if you have high-risk, intermediate to high-risk myelofibrosis, one of the great findings of our field is the JAK inhibitor class generally helps to improve symptom burden.
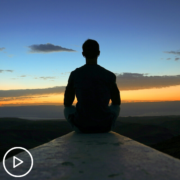
So, that is the splenomegaly, the fatigue, the pruritus. Maybe not so much the itching, but some of these other things. So, I think treating the underlying disease, that’s okay. Number two is many clinics, onc centers around the country are starting to open up a supportive care or fatigue center clinic. So, I am referring several of my patients there, we’re talking about diet, nutrition, exercise. We used to never talk about these things. Ruben Mesa has found that doing yoga and meditation can genuinely actually help the pathobiology to reduce the cytokine storm and improve the fatigue and quality of life.
Dr. Angela Fleischman, our colleague at UC Irvine, has done work suggesting that possibly an antioxidant diet such as the Mediterranean diet can help the overall general fatigue, well-being, wellness. And then of course I mentioned earlier, but I’ll mention here too, sometimes fatigue is outside of the MPN. Have you had your TSH or thyroid checked? What about your vitamin D levels? How are you doing on these PCP general checks? Things that may be contributing to the life and the happiness.
And finally, let me make a plug for mental health. I don’t know how much we were emphasizing before the COVID pandemic, but after, the last three or four years have been tough. Healthcare providers, caregivers, patients themselves, mental health checkup, that can also be contributing to fatigue, not getting out of bed, in addition to the organic medical problems. So, let me advocate a multifactorial approach, scientifically summed up as treating what you can with the underlying MPN, fine, treating the side effects and symptoms of the MPN, as you said.
And then, other, which can be a huge bucket, particularly as we get older, to not forget about that. Again, checking the thyroid level. And then when you’re on these different treatments, you can personalize it. Interferon, obviously, has its own separate set of side effects and then of course the other agents. So, I think that may be the best way to approach it. Maybe a three-bucket approach. The MPN itself, and then the treatment itself, and then the other, something like that.
Katherine Banwell:
And as you’ve mentioned, it’s all going to be personalized and individualized.
Dr. Pemmaraju:
Hugely.
Katherine Banwell:
Right, because what’s going to work for one person is not necessarily going to work for another.
Dr. Pemmaraju:
Hear, hear, well said to that. You know, you think you make a great diagnosis in the clinic, someone’s having fatigue, they’re on therapy for your MPN. You check the TSH, it’s wildly abnormal. Okay, you refer them to endocrine. Six months later, the thyroid level is completely normal now on thyroid medicine. And yet, the fatigue, brain fog, everything is still not clear.
The MPN is under good control. What gives? That’s the difficult part of these diseases. So, I really love what you said about the personalization and to keep looking and keep trying.