Becoming an Empowered and [ACT]IVATED MPN Patient
Patient Empowerment Network (PEN) is committed to efforts to educate and empower patients and care partners in the myeloproliferative neoplasm (MPN) community. MPN treatment options are ever-increasing with research advancements in treatments and testing, and it’s essential for patients and families to educate themselves with health literacy tools and resources on the latest information in MPN care. With this goal in mind, PEN kicked off the [ACT]IVATED MPN program, which aims to inform, empower, and engage patients to stay abreast of up-to-date information in myeloproliferative neoplasm care.
The [ACT]IVATED MPN program is aimed at newly diagnosed MPN patients, yet it can help patients at any stage of disease. [ACT]IVATED MPN helps patients and care partners stay updated on the latest options for their MPN, provides patient activation tools to help overcome care disparities and barriers to accessing care, and powerful tips for self-advocacy, coping, and living well with a blood cancer.

Myeloproliferative Neoplasm Disparities
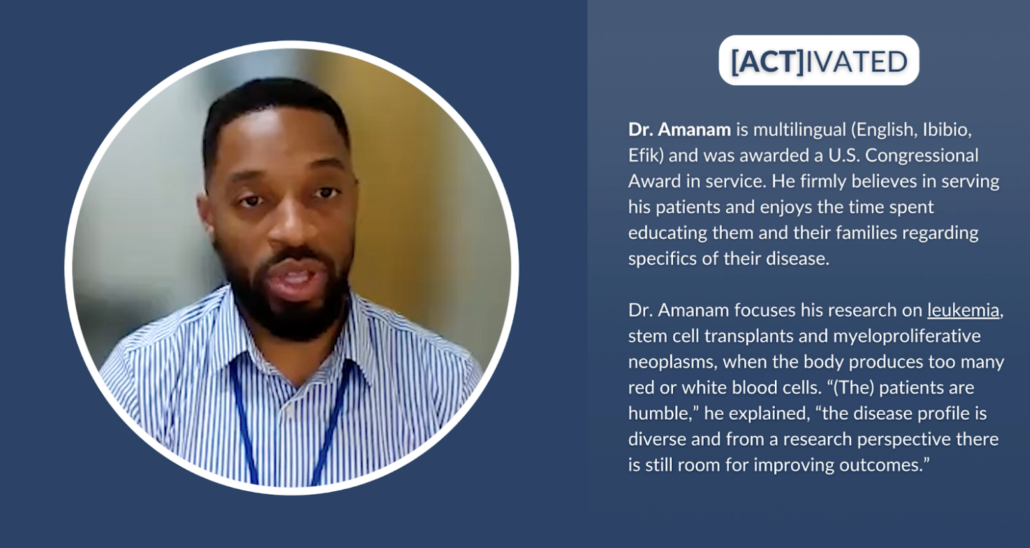
Race or ethnicity may have an impact on some health conditions, including MPNs. Cancer patient Lisa Hatfield interviewed Dr. Idoroenyi Amanam, Assistant Professor in the Division of Hematology at City of Hope. He explained about MPN risks and outcomes that may be impacted by patient race or ethnicity. “…we know that if you have high blood pressure, you have a higher risk for these complications-associated MPNs. And we know that African American males have a higher risk for that, so I think those things are…that example is a clear indicator that really identifying these basic risk factors that are related to diet, exercise, your weight, and other behavioral, possibly behavior-related factors may put you at higher risk to have complications from MPNs.”
Dr. Amanam further shared research findings and what needs further study to draw conclusions. “We have looked at incidences of thrombotic events in patients who have MPNs, and we tried to see if there was a difference between racial groups, and we didn’t. We did see that if you’re younger, you do have a higher risk of thrombosis over time, but there was no difference for if you were white, Hispanic, or African American. What we did find though, in a small single center study is that if you are non-white, there’s a higher risk of death over time. And I think we still need a lot of work to get a better understanding as to why that’s the case.”
Solutions for Improved Myeloproliferative Neoplasm Care
Clinical trials are key in moving MPN research forward to improved treatments and care. Dr. Amanam shared his perspective about other players besides patients who can help move the needle forward. “I think that going back to the idea that we want to practice the best science, we want to be able to publish the best data. The responsibility is on the clinicians, the scientists, the clinical trialists, the drug companies, the institutions to really be able to structure clinical trials that are relevant to our real world experience. And so how can we better encourage that? I think from a government perspective, potentially incentivizing drug companies and institutions and the other major players that really are involved in pushing this field forward to practice better science.”
Dr. Amanam expanded on how clinical trials can be diversified. “And once we’re clear that being able to have a diverse participant pool will give us the best results and therefore will lead to your drug being approved. I think we will have more participants from all groups.”
Some underrepresented patient communities may experience obstacles to MPN care. MPN Nurse Practitioner Natasha Johnson from Moffitt Cancer Center provided advice to help patients. “Patients themselves can research clinical trials by looking at clinicaltrials.gov and see what’s out there and contact the academic center that’s performing those trials. There’s free information online that provides recorded sessions from conferences or speakers or speaking done by the MPN experts that you can just look to and get to easily to help understand the disease, knowing the symptoms, and then guiding treatment.” Natasha Johnson continued with additional advice for optimal care. “.…to try to get into a large cancer center or academic center and see an MPN expert. Many times, this is just by self-referral. Charity is sometimes provided through these. Zoom visits can be done as consults or follow-up visits. So my encouragement would be search these out, find out who the experts are, and contact them directly and see if there is any possibility or a way that you can get in to see an MPN expert for a consult so you can get the best care possible.”
Signs of MPN disease progression is something that patients and providers must be on the lookout for. Natasha Johnson shared her advice for patients to empower themselves against disease progression. “…monitor your blood cell counts, be your own advocate. Think about if they’re changing, could it be medication, or is it disease progression? Monitor your symptoms. Look at the total symptoms score or write down your symptoms and try to record where you’re at in intervals. Are things getting worse? If they are, don’t wait three months for your next appointment. Contact your healthcare provider and ask to be seen. Ask about getting a repeat bone marrow biopsy to establish where the current disease status is because that can open up doors possibly to more treatments.”
The future of MPN care has an additional approach to address. Dr. Amanam shared his perspective and how patients can help advocate for improved treatments. “I think in the next three to five years, we’re going to have drugs that are going to actually be able to treat the underlying disease before it gets to a point where you may need more aggressive therapy…And so it’s exciting where we’re going, and I think the questions that as a patient that I would ask are, because of the fact that we only have few FDA-approved therapies, are there any clinical trials that are able to target the underlying disease as opposed to just treating the symptoms? I think that’s very important for the patients to ask, especially in this space now.”
Rates for stem cell transplant approvals must improve for lower income groups and for African American and Hispanic groups to provide better health outcomes for blood cancers like MPNs. Dr. Amanam explained what’s involved with transplants and how others can help as donors. “You can donate your bone marrow, or you can donate your stem cells that are not inside of your bone marrow. And typically as a donor, your experience of actually donating is about a day. And the recovery time after you donate your bone marrow or stem cells, it’s typically within about one to three days. So the benefit of donating your stem cells or bone marrow outweighs the inconvenience of a day or a couple of days of your schedule being altered. So I think that’s really important to understand. And I think if we can get more people to be aware of this, I think we can definitely get more donors.”
![[ACT]IVATED Program Logo](https://powerfulpatients.org/wp-content/uploads/Screenshot-2023-08-24-at-3.03.57-PM-1030x586.png)
[ACT]IVATED MPN Program Resources
The [ACT]IVATED MPN program series takes a three-part approach to inform, empower, and engage both the overall MPN community and patient groups who experience health disparities. The series includes the following resources:
- Myeloproliferative Neoplasm Basics for Newly Diagnosed Patients
- Are MPN Risks and Outcomes Impacted by Race or Ethnicity?
- What Does the Future of Myeloproliferative Neoplasm Care Look Like?
- Are There Any MPN Disparities in Subtypes and Genetics?
- Have MPN Disparities Been Addressed by Institutions?
- MPN-Related Complications | Are BIPOC Patients at Higher Risk?
- How Can MPN Clinical Trials Be Diversified?
- Understanding MPN Treatment Goals and Shared Decision-Making
- Are There Disparities in Stem Cell Transplant Outcomes?
- Bone Marrow Registries | What Myeloproliferative Neoplasm Patients Should Know
- Graft-Versus-Host Disease Risk for BIPOC Patients
- Emerging MPN Therapies in the Research Pipeline
- How Can Myeloproliferative Neoplasm Care Barriers Be Overcome?
- Myeloproliferative Neoplasm Financial and Care Resources
- How Can Underrepresented MPN Communities Access Support?
- [ACT]IVATED MPN Resource Guide
- [ACT]IVATED MPN Resource Guide en español
- [ACT]IVATED MPN Patient Vignettes
- [ACT]IVATED MPN Activity Guides
Though there are myeloproliferative neoplasm disparities, patients and care partners can take action to empower themselves to help ensure optimal care. We hope you can take advantage of these valuable resources to aid in your MPN care for yourself or for your loved one.
La historia de Yolanda: mi camino hacia un diagnóstico de neoplasia mieloproliferativa
La historia de Yolanda: mi camino hacia un diagnóstico de neoplasia mieloproliferativa from Patient Empowerment Network on Vimeo.
Yolanda, paciente latina con trombocitemia esencial (TE), tenía muchos síntomas antes de recibir su diagnóstico final. Observe cómo comparte los síntomas que experimentó, su largo camino hasta el diagnóstico y las lecciones aprendidas sobre el empoderamiento del paciente.
Related Resources:

|

Yolanda’s Story: My Path to a Myeloproliferative Neoplasm Diagnosis |

|
Transcript:
Mi nombre es Yolanda y a mediados de los 40 me diagnosticaron trombocitemia esencial (ET), una neoplasia mieloproliferativa. Soy una mujer latina, y mi camino hasta el diagnóstico llevó mucho tiempo.
Recordando mi experiencia, mis síntomas empezaron con fuertes dolores de cabeza y mareos que me impedían terminar mi trabajo. También experimenté una fatiga debilitante que me mantenía en cama durante un día o me hacía sentir como si mi visión y mi pensamiento estuvieran nublados. Todo era muy extraño y fui al médico, que me recetó antibióticos para una infección. Más tarde sentí entumecimiento y hormigueo en las manos y los pies, y luego dolor en el abdomen. Finalmente, mi médico decidió hacerme análisis de sangre completos para ver qué niveles podían ser anormales, a lo que siguió una biopsia de médula ósea para investigar más a fondo.
Cuando finalmente recibí el diagnóstico de trombocitemia esencial, sentí cierto alivio, pero también una sensación de hundimiento y temor ante lo que podría esperarme. Creo que uno de los problemas a la hora de recibir el diagnóstico puede haber sido que parecía saludable. Tal vez mi médico habría pedido los análisis de sangre antes si no tuviera buen aspecto. Pero intento mirar hacia delante y no hacia atrás.
Me recomendaron un especialista en MPN, que inicialmente me recetó una dosis baja de aspirina. Luego me recetó hidroxiurea (Hydrea). Me ha ido bien y me siento agradecida por tener opciones de tratamiento. Pero si mi enfermedad avanza hasta un punto en el que necesite otras opciones, ya he decidido que consideraré participar en un ensayo clínico. Creo que he sido relativamente afortunada y quiero compartir mi historia sobre el cáncer para ayudar a otras personas.
Algunas de las cosas que he aprendido en mi camino hacia MPN son:
- Empodérate haciendo preguntas a sus médicos sobre su MPN y sobre lo que puede esperar antes, durante y después del tratamiento.
- Infórmese sobre las opciones de ensayos clínicos. Puede haber programas que le ayuden con los gastos de viaje, alojamiento y otros gastos no cubiertos. Y los ensayos clínicos pueden ofrecer una opción para su MPN si ya ha utilizado todas las demás opciones.
- Tú eres la persona responsable de tu salud. Si cree que algo va mal en su cuerpo, defiéndase. Pida que le hagan más pruebas para averiguar qué le pasa.
- Tenga cuidado con dónde busca información sobre el cáncer. Utiliza fuentes creíbles como MPN Research Foundation, The Leukemia & Lymphoma Society y Patient Empowerment Network.
Estas acciones fueron clave para mantenerme en mi camino hacia el empoderamiento.
Share Your Feedback
Create your own user feedback survey
Yolanda’s Story: My Path to a Myeloproliferative Neoplasm Diagnosis
Yolanda’s Story: My Path to a Myeloproliferative Neoplasm Diagnosis from Patient Empowerment Network on Vimeo.
Latina essential thrombocythemia (ET) patient Yolanda had many symptoms before receiving her ultimate diagnosis. Watch as she shares the symptoms she experienced, her long path to diagnosis, and her lessons learned about patient empowerment.
Related Resources:

|

La historia de Yolanda: mi camino hacia un diagnóstico de neoplasia mieloproliferativa |

|
Transcript:
My name is Yolanda, and I was diagnosed in my mid-40s with essential thrombocythemia (ET), a myeloproliferative neoplasm. I’m a Latina woman, and my path to diagnosis took an extended time.
Thinking back on my journey, my symptoms began with severe headaches and dizziness that made it too difficult to finish my work. I also experienced debilitating fatigue that would either keep me in bed for a day, or I’d feel like my vision and thinking were in a fog. It all felt very strange, and I saw my doctor about the symptoms, but he prescribed antibiotics for an infection. Then later I felt numbness and tingling in my hands and feet and then pain in my abdomen. Finally, my doctor decided to run full blood work to see which levels might be abnormal, and that was followed with a bone marrow biopsy to further investigate.
When I finally received my diagnosis with essential thrombocythemia, I felt some relief but also a sinking feeling and dread of what might be ahead for me. I feel like one issue with getting diagnosed may have been that I looked healthy. Maybe my doctor would have ordered the blood work sooner if I didn’t look well. But I try to look forward rather than back. An MPN specialist was recommended to me, and he initially put me on low-dose aspirin.
Then I was prescribed hydroxyurea (Hydrea). I’ve been doing well and feel grateful to have treatment options. But if my disease progresses to a point where I need other options, I’ve already decided that I’ll consider participating in a clinical trial. I feel like I’ve been relatively lucky and want to share my cancer story to help others.
Some of the things I’ve learned on my MPN journey include:
- Empower yourself by asking your doctors questions about your MPN and what to expect before, during, and after treatment.
- Learn about clinical trial options. There may be programs that will help you with travel, lodging, and other uncovered expenses. And clinical trials may provide an option for your MPN if you’ve already used all other options.
- You are the person in charge of your health. If you feel like something is wrong in your body, advocate for yourself. Ask for more testing to find out what is wrong.
- Be careful about where you look for cancer information. Use credible sources like MPN Research Foundation, The Leukemia & Lymphoma Society, and Patient Empowerment Network.
These actions were key for staying on my path to empowerment.
Share Your Feedback
Create your own user feedback survey
Are MPN Risks and Outcomes Impacted by Race or Ethnicity?
Are MPN Risks and Outcomes Impacted by Race or Ethnicity? from Patient Empowerment Network on Vimeo.
Are myeloproliferative neoplasm (MPN) risks and outcomes impacted by patient race or ethnicity? Expert Dr. Idoroenyi Amanam from City of Hope explains common MPN symptoms, potential risks and outcomes, and patient advice for optimal care.
[ACT]IVATION TIP:
“…if you have stroke, heart attack, blood clots, abnormal counts, please follow up with your doctor and ensure that you get referred to the appropriate specialist to help assist in managing your complications.”
Related Resources:

Myeloproliferative Neoplasm Basics for Newly Diagnosed Patients |

What Does the Future of Myeloproliferative Neoplasm Care Look Like? |

MPN-Related Complications | Are BIPOC Patients at Higher Risk? |
Transcript:
Lisa Hatfield:
Dr. Amanam, how does race impact clinical MPN outcomes or complications? And are certain populations more susceptible to getting MPNs?
Dr. Indoroenyi Amanam:
Yeah, it’s a great question. I think, because of the fact that symptoms are not as clearly related to MPNs as opposed to some other diseases. So the major presenting symptoms for MPNs are related to high blood pressure or some other vascular abnormality, including strokes or blood clots. It takes a little work to diagnose MPN patients, and half of them are asymptomatic. And if you actually look at diagnosis rates, they’re one to three cases per 100,000 per year. And so this is very rare, and I think that we don’t have enough data to really understand if some groups are at higher risk to develop MPNs than others.
We have looked at incidences of thrombotic events in patients who have MPNs, and we tried to see if there was a difference between racial groups, and we didn’t. We did see that if you’re younger, you do have a higher risk of thrombosis over time, but there was no difference for if you were white, Hispanic, or African American.
What we did find though, in a small single center study is that if you are non-white, there’s a higher risk of death over time. And I think we still need a lot of work to get a better understanding as why that’s the case. So far we don’t have a clear signal for that, but I do think, in the same…the story that we understand for healthcare in general, there are some differences in terms of access to care, the quality of care that’s delivered in, you can guess that possibly that’s one of the reasons why that that affects African Americans and Hispanics disproportionately in this setting as well.
So my activation tip for this question would be if you have stroke, heart attack, blood clots, abnormal counts, please follow up with your doctor and ensure that you get referred to the appropriate specialist to help assist in managing your complications.
Share Your Feedback
Create your own user feedback survey
Myeloproliferative Neoplasm Basics for Newly Diagnosed Patients
Myeloproliferative Neoplasm Basics for Newly Diagnosed Patients from Patient Empowerment Network on Vimeo.
What do newly diagnosed myeloproliferative neoplasm (MPN) patients need to know? Expert Dr. Idoroenyi Amanam from City of Hope shares how he explains the condition, possible MPN complications, and proactive questions to ask your doctor.
[ACT]IVATION TIP:
“…if you see high platelet counts on a routine blood check or high white blood cell counts or high red blood cell counts, you should ask your doctor to delve a little bit deeper to try to get an answer as to why your counts are presenting in that fashion.”
Related Resources:

|

What Does the Future of Myeloproliferative Neoplasm Care Look Like? |

|
Transcript:
Lisa Hatfield:
Dr. Amanam, how do you explain MPN to your newly diagnosed patients?
Dr. Indoroenyi Amanam:
Yes, MPN is a very rare disorder, and so most patients haven’t heard of MPNs in comparison to breast cancer or colon cancer, and so it’s…sometimes it appears very ambiguous as to what it actually is, and for patients, I generally tell them that there’s some…it’s a disorder that causes increased production of their red blood cells or their platelets, or the cells that help support the tissue in their bone marrow. And there’s some complications associated with that, namely blood clots, strokes, and heart attacks. And there’s also a small risk of these patients converting over into more aggressive blood cancers, namely acute leukemia.
So my activation tip for this question is that, if you see high platelet counts on a routine blood check or high white blood cell counts or high red blood cell counts, you should ask your doctor to delve a little bit deeper to try to get an answer as to why your counts are presenting in that fashion.
Share Your Feedback
Create your own user feedback survey
[ACT]IVATED MPN Resource Guide en español
[ACT]IVATED MPN Resource Guide
What Is a JAK2 Mutation?
Editor’s Note: This resource, What is a JAK2 Mutation?, was originally published by MyHealthTeam.
One of the most commonly mutated proteins found in myeloproliferative neoplasms (MPNs) is the protein Janus kinase 2 (JAK2). This important discovery has changed how doctors diagnose and treat people with MPNs. We will be discussing both the JAK protein and the JAK gene.
MPNs are blood cancers caused by the overproduction of blood cells in the bone marrow. Mutations in the gene controlling JAK2 protein production occur most often in the three classic types of MPNs:
- Polycythemia vera (PV): Overproduction of red blood cells
- Essential thrombocythemia (ET): Overproduction of platelets
- Primary myelofibrosis (MF): Buildup of scar tissue in the bone marrow, inhibiting the production of new blood cells
The V617F mutation in the JAK2 gene is found in:
- 96 percent of polycythemia vera cases
- 50 percent to 60 percent of primary myelofibrosis cases
- 50 percent to 60 percent of essential thrombocythemia cases
Additionally, more than 50 different JAK2 mutations have been found in other parts of the JAK2 gene, primarily in PV cases.
What Is the JAK2 Gene?
The JAK2 protein plays an important role in controlling the production of blood cells from stem cells found in the bone marrow.
The JAK2 gene is responsible for genetically coding the JAK2 protein. This protein is part of the JAK/STAT pathway, which transmits signals to promote cell growth.
When the JAK2 protein is activated, it relays a signal to the protein STAT, which then binds to another STAT molecule in a process called dimerization. This group of molecules then moves into the cell’s nucleus, turning on genes that tell the cell to grow and proliferate.
What Causes JAK2 Mutations?
There are two main types of JAK2 mutations found in MPNs.
V617F Mutation
The V617F mutation is caused by a change in a single base in the genetic code. This simple change then switches the amino acid valine (V) to phenylalanine (F) at position 617 in the JAK2 protein, changing the shape of the protein. When this mutation is present, JAK2 signaling is turned on and cannot be turned off, leading to uncontrolled cell growth. In the case of MPNs, this causes an overproduction of blood cells, leading to blood cancers.
Multiple Mutations
Many different types of mutations can be found within multiple parts of the JAK2 gene. More than 50 different mutations have been identified in the gene, and almost all of these occur in people with PV.
One part of the JAK2 gene is particularly susceptible to mutations. This area genetically codes for a linker that connects two parts of the JAK2 protein. Common mutations here include deletions and insertions. A deletion is when entire pieces of the protein are lost. Insertions occur when incorrect pieces are put into the protein. Insertions and deletions change the shape of the JAK2 protein, which can affect its function.
Do JAK2 Mutations Cause MPNs?
MPNs are caused by a mutation in a single stem cell found in the bone marrow. These mutations cause the cell to rapidly divide, creating too many of one cell type. JAK2 gene mutations are involved in many cases of MPNs. In addition to JAK2 genes, mutations found in CALR and MPL genes are also common contributors to the development of MPNs. These three mutations are usually mutually exclusive, meaning that if one mutation is present, then the others are not.
JAK2 Mutations and MPN Diagnosis and Prognosis
A number of tests are required to diagnose MPNs, each providing a different piece of information. The doctor will begin with a physical examination and health history. They may also order a complete blood count (CBC) with a differential, which assesses the number of red blood cells, platelets, and white blood cells.
Because most MPNs are associated with a specific genetic mutation, a pathologist may use blood samples to test for these. Two tests used to identify genetic abnormalities are quantitative polymerase chain reaction (qPCR) and fluorescent in situ hybridization (FISH). Typically, only one of the two tests is required for diagnosis. It is also an option to perform DNA sequencing to identify the driving mutation in an MPN case.
Quantitative Polymerase Chain Reaction
Quantitative polymerase chain reaction (qPCR) is the most commonly used method for diagnosing JAK2 mutations. qPCR is also the most sensitive test, and it can detect small amounts of mutation when other methods fail.
With qPCR, DNA obtained from a blood test is mixed with a fluorescent dye, which is run through a machine that amplifies the sequences containing the JAK2 mutation.
Fluorescent In Situ Hybridization
This test determines whether someone has chromosomal abnormalities contributing to a cancerous phenotype. For example, one type of MPN, chronic myeloid leukemia (CML), is characterized by the presence of a Philadelphia chromosome (named for where it was discovered). A Philadelphia chromosome forms when two pieces of broken chromosomes stick together. This is also called the BCR-ABL1 gene, because one broken piece contains the BCR gene, and the other contains the ABL1 gene.
Most people with MPNs who are Philadelphia chromosome-negative (Ph-) have the V617F mutation in JAK2. This important discovery revealed the driving mutation behind Ph- MPNs. Before the discovery of JAK2 mutation, the cause of these defects was unknown. This also led to the development of specific JAK2 inhibitors for treatment of myeloproliferative disorders.
In 2016, the World Health Organization (WHO) revised its document “WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues.” This revision included new criteria for diagnosing MPNs by the three main driver mutations in JAK2, CALR, and MPL genes. PV is characterized by the presence of a JAK2 mutation. ET and MF are characterized by the presence of any of the three driver mutations.
JAK2 Mutations and MPN Treatments
Since the discovery of JAK2 mutations in MPNs, researchers have developed a number of inhibitors targeting the protein. There are currently two JAK2 inhibitors approved by the U.S. Food and Drug Administration (FDA) for the treatment of MPNs:
Jakafi
Jakafi (ruxolitinib) is approved for treatment of MF hydroxyurea-resistant PV. It is also being investigated for use in people with hydroxyurea-resistant ET. Additionally, some trials are investigating the effects of Jakafi in combination with the antimetabolite chemotherapies Vidaza (azacitidine) and Dacogen (decitabine). Antimetabolites are a special type of cancer drug that interfere with DNA by acting as a substitute for the normal building blocks of DNA.
Inrebic
Approved in 2019, Inrebic (fedratinib) is the newest MPN drug in almost a decade. It’s used to treat three forms: high-risk MF, post-polycythemia vera MF, and post-essential thrombocythemia MF with splenomegaly (enlarged spleen).
Other JAK2 inhibitors are currently in phase 3 clinical trials, including Pacritinib for the treatment of MF and severe thrombocytopenia, and Momelotinib for the treatment of MF. These promising new drugs are in final phases of testing.
Overall, the discovery of JAK2 mutations in MPNs has helped advance drug research, development, and MPN treatment. It has also helped combat uncontrolled proliferation of blood cells, improving the lives of people with MPNs. New medications continue to be developed and tested, providing a hopeful future for those affected by myeloproliferative diseases.
Finding Support With an MPN
You are not alone living with an MPN. When you join myMPNteam, you gain a community of others who know what it’s like to face a rare blood cancer diagnosis.
Do you know whether your MPN has tested positive for a JAK mutation? Did your doctor explain what the results of the test mean for your condition? Share your experiences on myMPNteam.



