Becoming an Empowered and [ACT]IVATED MPN Patient
Patient Empowerment Network (PEN) is committed to efforts to educate and empower patients and care partners in the myeloproliferative neoplasm (MPN) community. MPN treatment options are ever-increasing with research advancements in treatments and testing, and it’s essential for patients and families to educate themselves with health literacy tools and resources on the latest information in MPN care. With this goal in mind, PEN kicked off the [ACT]IVATED MPN program, which aims to inform, empower, and engage patients to stay abreast of up-to-date information in myeloproliferative neoplasm care.
The [ACT]IVATED MPN program is aimed at newly diagnosed MPN patients, yet it can help patients at any stage of disease. [ACT]IVATED MPN helps patients and care partners stay updated on the latest options for their MPN, provides patient activation tools to help overcome care disparities and barriers to accessing care, and powerful tips for self-advocacy, coping, and living well with a blood cancer.

Myeloproliferative Neoplasm Disparities
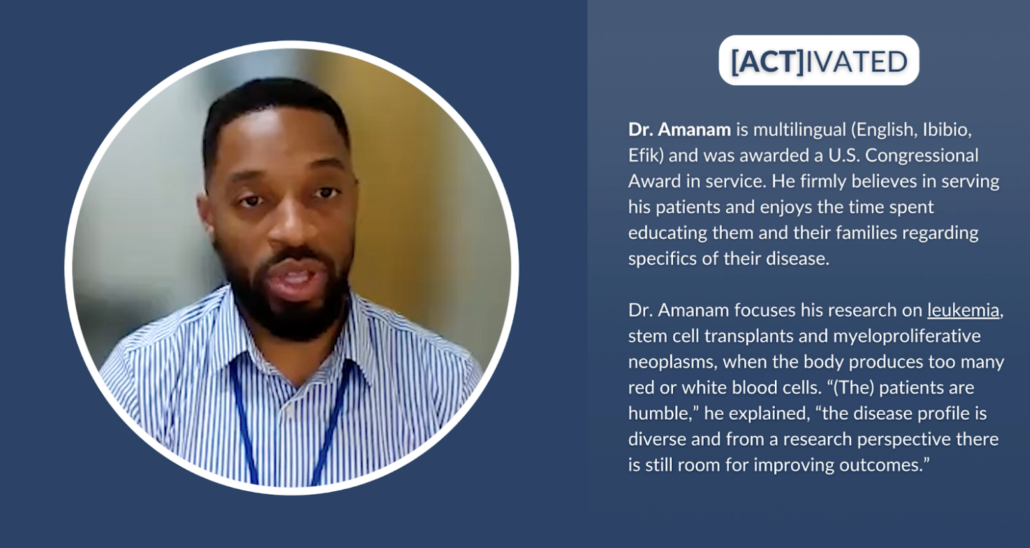
Race or ethnicity may have an impact on some health conditions, including MPNs. Cancer patient Lisa Hatfield interviewed Dr. Idoroenyi Amanam, Assistant Professor in the Division of Hematology at City of Hope. He explained about MPN risks and outcomes that may be impacted by patient race or ethnicity. “…we know that if you have high blood pressure, you have a higher risk for these complications-associated MPNs. And we know that African American males have a higher risk for that, so I think those things are…that example is a clear indicator that really identifying these basic risk factors that are related to diet, exercise, your weight, and other behavioral, possibly behavior-related factors may put you at higher risk to have complications from MPNs.”
Dr. Amanam further shared research findings and what needs further study to draw conclusions. “We have looked at incidences of thrombotic events in patients who have MPNs, and we tried to see if there was a difference between racial groups, and we didn’t. We did see that if you’re younger, you do have a higher risk of thrombosis over time, but there was no difference for if you were white, Hispanic, or African American. What we did find though, in a small single center study is that if you are non-white, there’s a higher risk of death over time. And I think we still need a lot of work to get a better understanding as to why that’s the case.”
Solutions for Improved Myeloproliferative Neoplasm Care
Clinical trials are key in moving MPN research forward to improved treatments and care. Dr. Amanam shared his perspective about other players besides patients who can help move the needle forward. “I think that going back to the idea that we want to practice the best science, we want to be able to publish the best data. The responsibility is on the clinicians, the scientists, the clinical trialists, the drug companies, the institutions to really be able to structure clinical trials that are relevant to our real world experience. And so how can we better encourage that? I think from a government perspective, potentially incentivizing drug companies and institutions and the other major players that really are involved in pushing this field forward to practice better science.”
Dr. Amanam expanded on how clinical trials can be diversified. “And once we’re clear that being able to have a diverse participant pool will give us the best results and therefore will lead to your drug being approved. I think we will have more participants from all groups.”
Some underrepresented patient communities may experience obstacles to MPN care. MPN Nurse Practitioner Natasha Johnson from Moffitt Cancer Center provided advice to help patients. “Patients themselves can research clinical trials by looking at clinicaltrials.gov and see what’s out there and contact the academic center that’s performing those trials. There’s free information online that provides recorded sessions from conferences or speakers or speaking done by the MPN experts that you can just look to and get to easily to help understand the disease, knowing the symptoms, and then guiding treatment.” Natasha Johnson continued with additional advice for optimal care. “.…to try to get into a large cancer center or academic center and see an MPN expert. Many times, this is just by self-referral. Charity is sometimes provided through these. Zoom visits can be done as consults or follow-up visits. So my encouragement would be search these out, find out who the experts are, and contact them directly and see if there is any possibility or a way that you can get in to see an MPN expert for a consult so you can get the best care possible.”
Signs of MPN disease progression is something that patients and providers must be on the lookout for. Natasha Johnson shared her advice for patients to empower themselves against disease progression. “…monitor your blood cell counts, be your own advocate. Think about if they’re changing, could it be medication, or is it disease progression? Monitor your symptoms. Look at the total symptoms score or write down your symptoms and try to record where you’re at in intervals. Are things getting worse? If they are, don’t wait three months for your next appointment. Contact your healthcare provider and ask to be seen. Ask about getting a repeat bone marrow biopsy to establish where the current disease status is because that can open up doors possibly to more treatments.”
The future of MPN care has an additional approach to address. Dr. Amanam shared his perspective and how patients can help advocate for improved treatments. “I think in the next three to five years, we’re going to have drugs that are going to actually be able to treat the underlying disease before it gets to a point where you may need more aggressive therapy…And so it’s exciting where we’re going, and I think the questions that as a patient that I would ask are, because of the fact that we only have few FDA-approved therapies, are there any clinical trials that are able to target the underlying disease as opposed to just treating the symptoms? I think that’s very important for the patients to ask, especially in this space now.”
Rates for stem cell transplant approvals must improve for lower income groups and for African American and Hispanic groups to provide better health outcomes for blood cancers like MPNs. Dr. Amanam explained what’s involved with transplants and how others can help as donors. “You can donate your bone marrow, or you can donate your stem cells that are not inside of your bone marrow. And typically as a donor, your experience of actually donating is about a day. And the recovery time after you donate your bone marrow or stem cells, it’s typically within about one to three days. So the benefit of donating your stem cells or bone marrow outweighs the inconvenience of a day or a couple of days of your schedule being altered. So I think that’s really important to understand. And I think if we can get more people to be aware of this, I think we can definitely get more donors.”
![[ACT]IVATED Program Logo](https://powerfulpatients.org/wp-content/uploads/Screenshot-2023-08-24-at-3.03.57-PM-1030x586.png)
[ACT]IVATED MPN Program Resources
The [ACT]IVATED MPN program series takes a three-part approach to inform, empower, and engage both the overall MPN community and patient groups who experience health disparities. The series includes the following resources:
- Myeloproliferative Neoplasm Basics for Newly Diagnosed Patients
- Are MPN Risks and Outcomes Impacted by Race or Ethnicity?
- What Does the Future of Myeloproliferative Neoplasm Care Look Like?
- Are There Any MPN Disparities in Subtypes and Genetics?
- Have MPN Disparities Been Addressed by Institutions?
- MPN-Related Complications | Are BIPOC Patients at Higher Risk?
- How Can MPN Clinical Trials Be Diversified?
- Understanding MPN Treatment Goals and Shared Decision-Making
- Are There Disparities in Stem Cell Transplant Outcomes?
- Bone Marrow Registries | What Myeloproliferative Neoplasm Patients Should Know
- Graft-Versus-Host Disease Risk for BIPOC Patients
- Emerging MPN Therapies in the Research Pipeline
- How Can Myeloproliferative Neoplasm Care Barriers Be Overcome?
- Myeloproliferative Neoplasm Financial and Care Resources
- How Can Underrepresented MPN Communities Access Support?
- [ACT]IVATED MPN Resource Guide
- [ACT]IVATED MPN Resource Guide en español
- [ACT]IVATED MPN Patient Vignettes
- [ACT]IVATED MPN Activity Guides
Though there are myeloproliferative neoplasm disparities, patients and care partners can take action to empower themselves to help ensure optimal care. We hope you can take advantage of these valuable resources to aid in your MPN care for yourself or for your loved one.




















