What Questions Should You Ask About a Proposed Thyroid Cancer Treatment Plan?
What Questions Should You Ask About a Proposed Thyroid Cancer Treatment Plan? from Patient Empowerment Network on Vimeo.
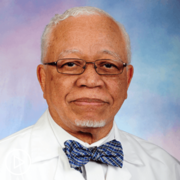
What questions should you ask about a proposed thyroid cancer treatment plan? Dr. Wirth provides guidance on self-advocacy, seeking a second opinion, and discussing essential molecular testing for identifying targetable gene alterations.
Dr. Lori Wirth is the Medical Director of the Center for Head and Neck Cancers at Massachusetts General Hospital. Learn more about Dr. Wirth.
See More from Evolve Thyroid Cancer
Related Resources:

|

|

|
Transcript:
Katherine:
What questions should patients ask about their proposed treatment plan?
Dr. Wirth:
So, Katherine your questions are so spot on, and these are the kinds of questions that we get asked in clinic all the time. And I could say one thing that I think, I don’t know if medical students still are in this, but I learned this in medical school. If a patient says to you, “What would you say to me if I were your mother?”
You’re not supposed to answer that question because of course you’re going to have your biases. But I realize people ask me that question all the time. And so, it’s a good question, so I should answer it because it’s a good question. But I think that I would simply encourage people to not be shy. Their doctors care deeply about them. Their doctors are pressed for time, but their doctors are always going to be happy to stop and answer every single question that the patient has. And the most basic questions are the best ones, but sometimes they’re also the hardest question to ask. But coming with a list of the important questions is very helpful. Bringing along a family member or friend and having them have their list of questions is also very helpful.
But writing down especially the hard questions can help you ask the question because it can be hard to say, “How long might this drug help me live?” Asking about how long I might live can be really hard to say, but if you’ve got it written down there, it’s a little bit easier to say. Or if it’s hard for you to get those words out, hand your doctor over your notebook, and your doctor can look at the questions and help answer the questions.
So, I just would encourage people to think in advance about what the questions are that they want to make sure that they cover and jot them down. And don’t be shy. Don’t be shy about saying, “Do you think it would be worthwhile for me to get a second opinion? And if so, who do you recommend?” And most doctors are perfectly content with somebody asking if they think a second opinion would be a good idea.
And I’ve always said if I were diagnosed with cancer, I would want to have a second opinion just to be sure that what my favorite doctor was saying to me really sounded right. So, don’t be shy about asking for second opinions. With thyroid cancer I also think now it’s so important that we’re doing the molecular diagnostics of the tumors for patients to identify those patients that have targetable gene alterations. And it is still a relatively new thing in oncology to do molecular diagnostics for thyroid cancer as well as other solid tumors. And so, it is something that is not always recommended or offered to patients. But that’s something that patients with thyroid cancer should absolutely ask their doctors about.