How Is Research Advancing Myeloma Treatment and Care? from Patient Empowerment Network on Vimeo.
A panel of myeloma experts, including Drs. Omar Nadeem, Irene Ghobrial, and Betsy O’Donnell, discuss how clinical trials advance myeloma research and share an update on promising therapies in development.
Dr. Omar Nadeem is the Clinical Director of the Myeloma Immune Effector Cell Therapy Program and Associate Director of the Multiple Myeloma Clinical Research Program at the Dana-Farber Cancer Institute. Learn more about Dr. Nadeem.
Dr. Irene Ghobrial is Director of the Clinical Investigator Research Program at Dana-Farber Cancer Institute and Professor of Medicine at Harvard Medical School. Learn more about Dr. Ghobrial.
Dr. Betsy O’Donnell is Assistant Professor of Medicine at the Dana-Farber Cancer Institute specializing in Plasma Cell Disorders.
See More From INSIST! Myeloma
Related Programs:
Transcript:
Katherine Banwell:
Where do clinical trials fit into a patient’s treatment plan?
Dr. Omar Nadeem:
Yes. So, clinical trials as a term, a lot of times patients have a lot of questions about what that means. There’s a lot of misconceptions, I would say.
Sometimes patients think they will get either a placebo and they won’t get the adequate treatment, or that they may not get the right treatment, right, because they’re taking a chance going on a clinical trial. It’s actually the opposite. So, all the trials are really designed to improve upon what we already know works in a particular disease, right? So, when we think about trials let’s say in relapsed myeloma, where the patient has already had some of the approved therapies, we’re looking at the most promising new therapies that have shown efficacy either in the lab or first in human studies and then moving them through the different phases and studying them in more and more patients.
And that’s how all these drugs get started, right? So, they all get started at that point and then make their way to earlier lines of therapy.
Then you’re trying to answer different questions as part of clinical trials. So, which one of these therapies can I combine, for example. Which ones can I omit, which ones – so, they’re all sort of getting the standard therapy and getting something either added on top of it or removed, depending on what the question that we’re asking.
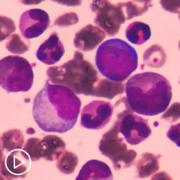
And then in the world that we currently live in with precursor plasma cell disorders, as Dr. Ghobrial mentioned, we have lots of patients that are at high risk of developing multiple myeloma in their lifetime, and that could be in a few years to a decade. And a lot of these therapies are so effective, and we’re now trying to really study some of these rationally in that patient population, so that’s a very different clinical trial, for example, than what I described earlier.
So, it really depends on what you’re trying to achieve and where you are in the phase of your disease.
Katherine Banwell:
This next question is open to all of you. Are there therapies in development that are showing promise for patients with myeloma? Dr. O’Donnell, let’s start with you.
Dr. Betsy O’Donnell:
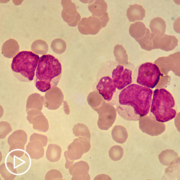
Yes. So, I think we are so fortunate in multiple myeloma to have so much interest in our disease and so many great drugs developed. So, as Dr. Nadeem was discussing, CAR-T cells are an immunotherapy, the ones that are approved now, we actually are fortunate to have two CAR-T cells approved, target something very specific called B-cell maturation antigen.
We’re now seeing the next generation where we’re looking at other targets on the same cancer cell, that plasma cell, so those are evolving.
Same thing is true in the bispecific antibody space. Again, those target BCMA now, but we have newer bispecifics who look at alternate targets, and really what this does is it gives us different ways of approaching the cancer cell, particularly as you relapse through disease.
Dr. Irene Ghobrial:
I would probably say we’re also getting into targeted therapies and more of personalized, so if you have an 11;14 translocation, venetoclax (Venclexta) would be an amazing drug for that. And the more we can say my own personal myeloma, what’s the best treatment for me, that’s how we’re trying to do it. So, it may not be exactly precision medicine, but we’re getting closer and closer to precision medicine of my myeloma, my specific drugs. And even if people have a 17p deletion, then we would say let’s think of that immunotherapy.
It is truly a renaissance for us, and we’re starting to get into trispecifics, into off-the-shelf CAR-T, into so many new things. Into two different antigens that are expressed for the CAR-Ts. I mean, we are really beginning the era of immunotherapy, and we’re excited to see how much we can go into that because it will completely change myeloma, and hopefully we will cure many patients. We think we have already amazing drugs. It’s a matter of when to use them and who is the right person for this right drug.
Katherine:
What are you hopeful about the future of care for myeloma patients? Dr. Ghobrial, do you want to start?
Dr. Irene Ghobrial:
I’m hopeful that we truly cure myeloma, and no one should ever develop end organ damage.
We should identify it early and treat it early, and no one should ever come in being diagnosed with multiple myeloma.
Katherine Banwell:
Okay. Dr. Nadeem?
Dr. Omar Nadeem:
Yes, I think I definitely agree with what Irene said, and really having a more thoughtful approach to each individual myeloma patient. As I mentioned earlier, we have so many available therapies. I want to be able to know exactly which patients need which path in terms of treatment, and which ones we can maybe de-escalate therapy, right? So, thinking about which patients do well and maybe can get away with not being on continuous therapy, and those that absolutely need it. Identifying them better to give them the best therapy.
Katherine Banwell:
Dr. O’Donnell, do you have anything to add?
Dr. Betsy O’Donnell:
I think we all share a common goal, which is cure, and for those who we can’t cure yet, I think really working on making the experience as good as it possibly can be and focusing on the factors that we can control and optimizing those, both for patients and their caregivers who are in this journey together with the patient.