PEN Blog Archives
CSC Arizona Embraces digital sherpa® Train-the-Trainer Program
When the staff at Cancer Support Community (CSC) Arizona heard about the Patient Empowerment Network (PEN) digital sherpa® Train-the-Trainer program, they knew it was just the kind of programming they were looking for. “We wanted to be able to help the more vulnerable members of our community,” says Caitlin Morrissey, CSC Arizona’s Executive Administrative Coordinator. The goal was to help make things easier for the cancer patients they serve, and Caitlin says that helping patients to navigate things like social media and ride shares, and helping them to connect with loved ones as well as their healthcare providers through PEN’s digital sherpa® program, was a great way to start.
The digital sherpa® program is designed to help cancer patients (who are mainly 65 and older) learn to use technology as a tool to help them through their cancer journey. Patients and their care partners can learn basic internet and social media skills. They can also learn how to access their patient portals and find information and support regarding their illness. Patients can also have their specific technology-related questions answered. Organizations who want to implement the digital sherpa® program can utilize the digital sherpa® Train-the-Trainer program, which is designed to do exactly what it says. The program trains volunteers and other individuals to be trainers, or sherpas, for the digital sherpa® program.
“It’s an amazing program and I’m excited to be a part of it,” says Caitlin who started overseeing the digital sherpa® and the digital sherpa® Train-the-Trainer programs shortly after CSC Arizona adopted them in early December 2021. Despite beginning the program during the busy holiday season and while their offices were still operating remotely due to the pandemic, Caitlin has already seen impactful results. She says participants are relieved and excited when they learn what their devices can do, and they have provided very positive feedback through program surveys. Participant Arcelia Lopez said the program gave her access to a new world.
“From the very beginning to the end was an opportunity to have an experience that opened a new world,” Arcelia wrote. “This was a lifesaving experience that I embraced. Everything that was offered and designed was so conducive to learning and building self-confidence.”
Arcelia’s survey responses solidified Caitlin’s passion for the program. “It was amazing to have that feedback from her. It really drives home how important this is,” says Caitlin.
In 2021, organizations like CSC Arizona, that participated in the digital sherpa® Train-the-Trainer program received a $2,500 microgrant from PEN to help offer the program to their communities. CSC Arizona didn’t waste any time putting their microgrant to good use. Director of Operations Kyle Jones recognized that some of their community members didn’t have access to computers or devices, so he purchased several Chromebooks for participants to use for the digital sherpa® workshops. CSC Arizona was also able to give Chromebooks to two individuals, one of which was Arcelia. “Having the gift of the Chromebook changed my life mentally and emotionally and secured my future in having the confidence I needed to maintain my health. It changed me in a way that I didn’t know was possible. It allows me to live in a way that I didn’t know was possible,” wrote Arcelia in response to the program.
Caitlin says that implementing the digital sherpa® Train-the-Trainer program was seamless. She says the program was easy to follow, could be completed online, and didn’t take too much time so they were able to offer help to patients right away. In a short time, CSC Arizona has already used the digital sherpa® Train-the-Trainer program to create a lasting impact in their community. Their fledgling program of trainers includes Caitlin, Kyle Jones, and one outside volunteer. They have offered small group workshops, one-on-one trainings, and have made a house call. Thanks to the online aspects of the program, they were even able to help a patient in Illinois who discovered that they were offering the program and reached out for some help. Going forward Caitlin wants to build the program. She wants to recruit more volunteers and she is already introducing the digital sherpa® program to new patients as they come into CSC Arizona. She looks forward to adding regular group sessions but also continuing to offer the one-on-one sessions to anyone who needs them. Caitlin also has plans to create and offer the digital sherpa® workshops specifically geared toward Spanish speaking participants. “I’m really excited to continue offering it and making it better and better as we go along,” she says.
Caitlin and the rest of team at CSC Arizona are utilizing the digital sherpa® Train-the-Trainer program to empower and make a difference in the lives of the cancer patients they serve. “Every detail is looked at and every detail is considered,” Arcelia noted in her survey. “It creates an opportunity to not allow cancer to win.”
Jennifer Lessinger is a professional writer and editor who learned the value of patient empowerment during her struggle with a hard-to-diagnose and complex endocrine disorder.
Medicare Doesn’t Cover Free At-Home Covid Tests, But You Still Have Other Options to Attain Free Ones
The Biden Administration’s new mandate that insurers cover the cost of at-home test did not include beneficiaries of Medicare. This is very unfortunate because Medicare recipients are the largest at-risk population.
The new mandates that private insurers cover the cost of at-home-test – up to eight per enrollee per month. And, because Medicare enrollees are not participant of this mandate, this leaves many afraid of the consequences. There are about 63.3 million people enrolled in Medicare and the majority of these beneficiaries, 55.1 million, are age 65 or older, and the rest, though younger, are generally people with disabilities. Many of which may have illnesses that leave them very vulnerable to COVID.
The mandate which took place on January 15th, means that most consumers with private health coverage can buy at-home test at a store or online and either get it paid for upfront by their insurance company by submitting their insurance card or get reimbursed by submitting a claim to their insurer.
Fortunately, there are still options for Medicare beneficiaries to get access to free COVID test.
Here are your options:
- You can order four free tests through Covidtest.gov, a new government website that officially launched on January 15th. This site is available to all households not just Medicare beneficiaries. This is for 4 free at-home test per month/per household. Therefore, you may have to reorder every month.
- You can also pick up at-home COVID test for free at Medicare-certified health clinics.
- Community health centers. Be aware that currently demand for the test are outpacing supply, so plan accordingly.
- For Medicare beneficiaries that are enrolled in a Medicare Advantage plan, reach out to your insurer as they may cover the cost of the at-home Covid test. It’s worth a try. The tests may be covered under a supplemental benefit through the insurer, not a required benefit.
- Don’t forget the many testing sites that are offering free Covid testing. Beneficiaries can get the lab-based PCR test, (can take a few days to get back the test results) rapid PCR test, and the rapid antigen test. These sites were really stacked during the Holiday’s, they may be less busy now. A bonus is that many of these sites are drive through, providing you with less exposure to people.
- Additionally, if a doctor or other authorized health-care provider orders the test, there is no cost-sharing.
- Medicare beneficiaries are allowed to get one lab test for free per year without a doctor’s order.
It hardly seems fair that Medicare beneficiaries have to jump through more hoops to get access to the free tests. However, this is due to the specific legal authority used to implement the directive.
It seems that for now, this is how it will continue unless there’s another strong push for Medicare recipients to be included in the mandate. At which point It would require congressional action. For now, Don’t Hold Your Breath!!

Diahanna Vallentine, BCPA, Financial Empowerment Lead
In 2002 Diahanna and her husband received the news that her husband had MGUS, a precursor to Multiple Myeloma. Upon her husband death in 2013, Diahanna immediately decided to make it her mission to help patients and caregivers empower themselves to speak up and to position themselves as partners in their treatment. Diahanna became a Board-Certified Patient Advocate. She is currently the Financial Myeloma Coach for The Myeloma Crowd Foundation.
Applications of Computer Vision In Healthcare
All the technological advances developed in healthcare allowed us to understand the anatomy and physiology of the different organs that structure the human body more precisely in recent decades. With the development of computer vision and artificial intelligence, it is relatively easy to identify the diseases from early phases to begin the treatment on time.
The advanced applications provide the ability to process, analyze, and understand complex information for early diagnoses. From a bird’s eye view, a complex interaction of SuperData, same as quality data, machine learning, and analytics applicable to detection, speech recognition, computer vision, etc., offers potential outcomes.
Computer vision developments promise to make healthcare more precise and accessible to all. Here, we focused on presenting the game-changing technology of computer vision in healthcare, by connecting biology aspects with artificial intelligence and computer vision for precise treatment.
The role of computer vision in healthcare
Computer vision encompasses training a model with the right data to help the model detect objects and draw conclusions. It automates, comprehends, and imitates human visual data systems to predict desirable outcomes. Computer vision functions include:
- Obtaining the images,
- Transforming the data into images,
- Separating multidimensional data from them.
Providing insights, this analyzed data is HIPAA-compliant and helps to identify patterns, objects, and trends in labeled data. Technological advances in computer vision provide the following benefits to the healthcare industry:
- Rapid medical research
- More accurate and coherent imaging analysis
- Decreased labor expenses and lower insurance costs
- Better patient identification in the cases of mistaken identity
- Consistent and accurate results
- Smart operating rooms eliminating manual efforts
- Safety equipment usage and identifying sterile processing failures
The top applications of computer vision in healthcare
Computer vision applications in healthcare sector and increasing, yet a few common examples include:
COVID-19 diagnosis
Due to the COVID-19 pandemic, the healthcare system is constantly facing challenges in terms of supporting critical patients and medical costs on time. Computer vision and artificial intelligence widely utilized for COVID-19 prediction and analysis.
Computed tomography (CT) images, Magnetic Resonance Imaging (MRI), and clinical data provide helpful input to AI algorithms, scanning different human body sections to identify the diagnosis. Training steps and higher resolution raise the model performance, allowing higher hyperparameters on the results, not to mention the importance of having a reliable annotation tool at hand.
For better clinical decision-making, visualization tools contribute to high-quality 3D images in the domain of COVID-19 detection. Here is more on COVID-19 diagnosis applications:
- X-ray radiography (CXR) — It assists radiologists in correctly recognizing lung infection and producing quantitative analysis and diagnoses.
- Disease progression score — It has become essential to analyze disease progression to recognize patients with a high risk to develop severe COVID-19 infection before it’s too late.
- Masked face recognition — One of the successful ways to prevent COVID-19 from spreading is wearing masks in public gatherings. Detection and recognition of masked faces tremendously benefit in large public settings.
Cancer detection
With technological advances, it is now possible to detect cancer in earlier stages. Since some symptoms of skin problems are similar, it’s difficult to identify forms of cancer including but not limited to skin, bone, breast cancer.
The trial of trained models over 1.2 million skin cancer images has shown successful results, the same as certified professionals. Cancer detection as well as cell classification applications cover the following:
- Semantic segmentation — The most challenging part of medical image analysis is to identify the pixels of organs or lesions from background medical images, including MRI or CT images. Semantic segmentation helps to classify each pixel belonging to a specific label.
- EEG analysis — The Electroencephalogram analysis mainly used for neural dysfunction including cancer detection, brain tumor, has great potential to bring forward advancement in accuracy and treatment of neural dysfunctions.
- Cell classification — Cell classification creates a visualization of specific tissues and organs to predict more accurate diagnoses. Cell classification applications include comprehending the consequences of drugs and genes in screening experiments, localization of various proteins, as well as diagnoses of cancer from images acquired using different approaches.
- Drug discovery — It incorporates many levels from recognition of targeted symptoms and diseases, implementation of experiments, and formation of chemical compounds outlined to transition in regions prompting the underlying disease.
- Cell biology — Researching the particular structure and attributes of an organism’s genetic fabrication can provide deeper analysis into development status. This outlook helps with cell image classification, where most of the time biological processes are hardly seen by the human eye.
- Digital pathology — Allowing patient tissue samples along with digital whole slide images (WSIs) to be distributed on an international scale for diagnostic, educating, and research purposes.
Movement Analysis
This measuring method is used in computer vision and image processing to identify movement. The purpose of movement analysis is to sense motion in an image, trace and identify an object’s motion in a particular time frame, class of objects that make a move together, and detect the direction of motion.
Gathering information helps healthcare providers trace muscle activity, perform gait analysis and diagnose possible mobility issues. For patients with cerebral palsy, joint issues, muscular dystrophy, and such diagnoses, movement analysis tests are required in a certified laboratory.
A variety of movement analysis systems allow movement to be captured in different settings, which can broadly be classified into devices interconnected to the body and video-based techniques. While some methods require to be captured in diverse environments, others can be distinguished in specific settings.
Tumor Detection
Approximately 70% of tumors are detected in the later stages of the disease when it is challenging to treat, which defines the low survival rate. Computer-aided diagnostic tools assist radiologists to spot malignant tumors in earlier phases. Deep learning systems predict what tumor is from the basis of large real-world data sets and examples.
Applying trained algorithms to evaluate images detects the most subtle tumor pattern within seconds, facilitating a supplementary resource for physicians. These applications are useful to save patients’ lives and diagnose with accurate treatment before any harmful stage. New techniques are developed to better the precision of tumor diagnosis.
Summing up
Computer vision in healthcare has evolved substantially over recent times, and various technological research has contributed a vast amount of important information to the industry. Computer vision has the probability to be applied across diverse environments and disciplines. The requirements and priorities for a computer vision in the healthcare sector heavily depend on the unique capture environment and research area across different disciplines. Computer vision in healthcare is advancing further from the newer implementations in technology. The applications are in development phases with the potential to improve medical procedures around the world. Helping doctors to reduce the time and efforts required in predicting health conditions or results of medication, these applications benefit healthcare providers.
Melanie Johnson, AI and computer vision enthusiast with a wealth of experience in technical writing. Passionate about innovation and AI-powered solutions. Loves sharing expert insights and educating individuals on tech.
#CloseTheCareGap in #CancerCare
World Cancer Day held every February 4th is the global uniting initiative led by the Union for International Cancer Control (UICC). The goal of this day is to raise worldwide awareness, improve education, and catalyze personal, collective and government action. By working together, millions of preventable cancer deaths are saved and access to life-saving cancer treatment and care is equitable for all – no matter who you are or where you live.
This year’s World Cancer Day’s theme, “Close the Care Gap”, is all about raising awareness of this equity gap that affects almost everyone, in high as well as low- and middle-income countries, and is costing lives. The PEN team, including staff, Empowerment Leads, and Board Members, put together a special video to raise awareness.
#CloseTheCareGap in #CancerCare from Patient Empowerment Network on Vimeo.
Cancer Facts
- Half the world’s population lacks access to the full range of essential health services, and many are denied basic cancer care
- Why? Due to differences in income and education levels, geographical location, and discrimination based on ethnicity, race, gender, sexual orientation, age, disability and lifestyle.
- 10 million people died of cancer in 2020. That’s equivalent to the population of Bangkok or twice the population of Ireland.
- There are now 19.3 million new cases of cancer in a year. Yet 30-50% of all cancers are preventable. Reduce the risks of cancer with healthier behaviors, regular screening, earlier detection and timely treatment of pre-cancers.
- Up to 10% of cancers are related to genetic mutation. 27% of cancer deaths are from tobacco and alcohol use.
- 70% of cancer deaths occur in low-to-middle income countries.
- Less than 30% of low-income countries have cancer treatment services available (compared to 90% in high-income countries).
- Cancer kills nearly 10 million people a year and some 70% of those are aged 65 or older, yet older populations face disproportionate barriers to effective treatment.
Resources
- Best Care No Matter Where You Live is an advocacy and empowerment program for patients and families facing a cancer diagnosis where many factors, including age, ethnicity, socioeconomic status, gender and insurance type may impact disease outcomes. Feel more in control of your health journey and gain confidence around your treatment decisions no matter your geography with powerful self-advocacy vignettes and empowered patient and care partner expert segments.
- Digitally Empowered™ helps you become more tech-savvy so you can find information and support to empower you and your loved ones during your cancer journey. By improving your tech skills, you can open the door to a whole new world of knowledge and tools to help you research your condition, ask informed questions and take an active role in shared decision making with your care team.
- digital sherpa™ Train-the-Trainer allows community-based organizations to bring digital sherpa™ to their members by giving them the tools and resources to host personalized workshops. digital sherpa™ helps cancer patients (mainly 65 and older) and their families become more tech-savvy. By educating them in basic internet and social media skills, this empowers them become more knowledgeable.
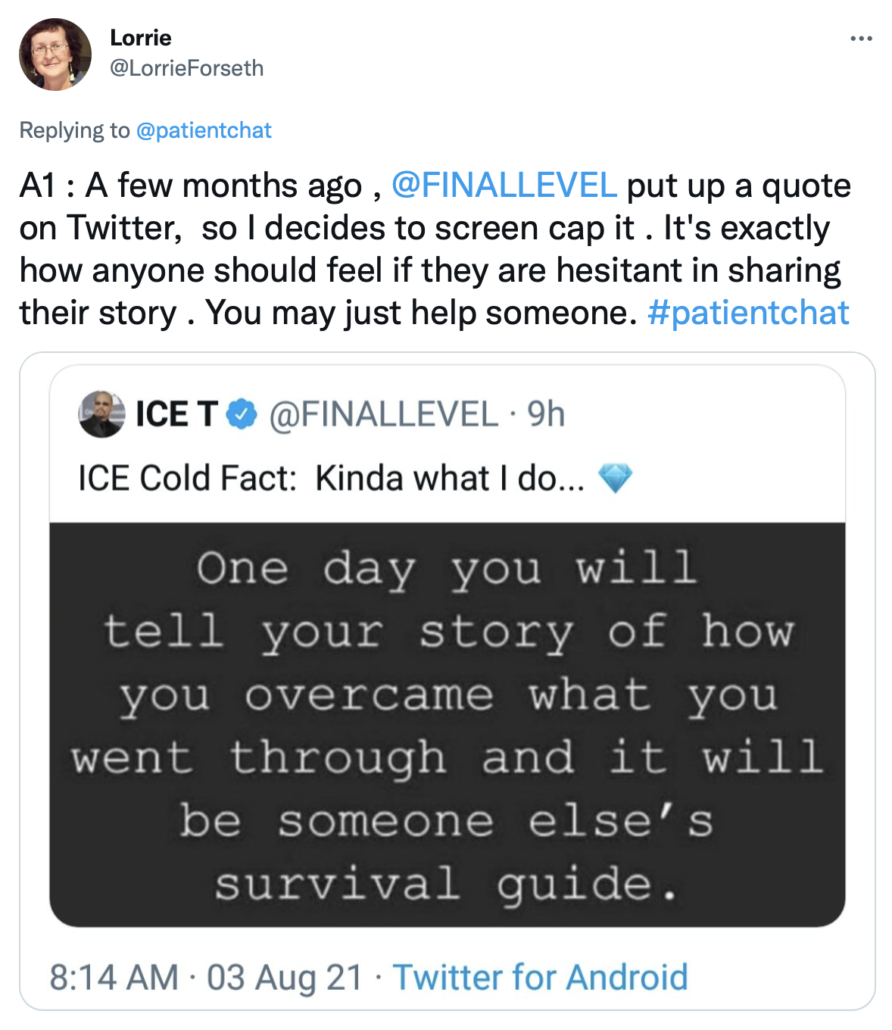
#patientchat Highlights – Building Power Through Your Story
Last week we hosted a “Building Power Through Your Story” #patientchat. The #patientchat community came together on Twitter for a lively discussion. Take a look at the top tweets and full transcript from the chat.
Top Tweets
Why is it important for patients and/or care partners to share their stories with others?
Full Transcript
January 2022 Digital Health Round Up
Technology has changed the face of healthcare; this new year begins with exciting advances that positively affect the patient and the provider. Providers embracing telemedicine are creating opportunities to change the entire patient experience. The use of AI (artificial intelligence) can take care of tasks that free up more time for providers to spend with the patients. AI is also being used to help identify patients with certain head and neck cancers, that would benefit from lower doses of radiation, decreasing radiation toxicity and side effects for patients.
Healthcare Technology
If you can achieve the right mix of high-tech, high-touch options, you’ve hit the sweet spot for improving equity and accessibility, patient engagement, health outcomes, loyalty, and profitability, reports MedCityNews.com. Telemedicine offers patients a way to seek medical care without missing work and often from the comfort of their own home. With proper education, telemedicine makes healthcare accessible to everyone regardless of language barriers or disabilities. Telemedicine does not replace the hands-on approach of medicine, but it offers interesting and convenient options for patients. During the pandemic, telemedicine has proven to be a powerful tool to stay in touch with patients and keep everyone safer. Find more information here.
Artificial Intelligence to Support Both Caregivers and Patients
In healthcare, as in all fields, the job of AI is not to replace humans, but rather to perform repetitive, tedious and time-consuming tasks so that people don’t have to – freeing time for tasks that require personal touch, reports Enterpeneur.com. AI uses algorithms to predict patient volumes for hospitals, anticipating appropriate staffing for caregivers. AI can quickly sort through images and information saving providers time to get them the appropriate information faster. Humans will always be the ultimate decision makers, but AI can be a tool to help them provide better care. With the increasing demands on providers, time with patients is the most important aspect of their job. Artificial intelligence allows for more efficient use of that time, allowing for better patient outcomes. Find more information here.
Artificial Intelligence to Help Patients Avoid Excessive Radiation
A Case Western Reserve University led team of scientists has used artificial intelligence (AI) to identify which patients with certain head and neck cancers would benefit from reducing the intensity of treatments such as radiation therapy and chemotherapy, reports MedicalXpress.com. The AI program analyzed hundreds of tissue samples from patients with a particular type of head and neck cancer. It was able to pick out some of those patients that could have done well with a lower dose of radiation. Reducing the level of chemotherapy and radiation can significantly reduce some of the toxic side effects of the treatments. Using Artificial Intelligence to achieve this can give the patient better quality of life. There is hope in the future that this application can be used in clinical trials and eventually with other types of cancer as well. Find more information here.
Technology is an important partner to healthcare providers and patients. Every day there are great advances in treatment due to artificial intelligence. The potential of telemedicine is expanding and helpful in our daily lives. Technology is an area of healthcare to follow and see all the benefits it will provide for patients and caregivers alike.
Dana Kaiser is a professional writer and a strong patient advocate, learning from experience during her 22-year career as a nurse.
Patient Advocacy: 6 Tips for Making A Visual Impact on Social Media
When it comes to sharing your advocacy message visual impact is a key factor in creating more visibility for your cause and increasing online engagement. In an increasingly crowded digital landscape, where our minds are drawn more readily to content that catches our eye, images can break through the online content clutter to quickly communicate your message.
It stands to reason that the visuals you create and share online should set the right professional tone for your advocacy activities. To help you do this, I’ve put together a list of six tips to increase the visual impact of your social media posts, alongside a list of tools to help you create more professional-looking graphics.
1. Upload A High-Resolution Image
Upload larger high-resolution images to social media. When an image file is too small, it will stretch, resulting in poor image quality and pixelation. Pixelated images appear unprofessional and reduce the likelihood they will be shared by others.
2. Choose Clear Typography
Typography is made up of elements such as font type and size, kerning (white space between individual characters or letters), and tracking and spacing. Typography is important when it comes to making your content more understandable to your reader. Visit Google Fonts directory, a free tool to help you choose the best font for your graphic design.
3. Pick The Right Colors
Color design is an essential design element. Ask yourself if your color choice is easy on the eye. If you use a combination of colors do they complement each other? Complementary colors are those that are placed opposite to each other on the color wheel.
Keep your color palette simple. Don’t be tempted to use too many colors in your designs. Pay attention to the hue and saturation values of the chosen colors – lightening or darkening tones to convey more warmth or strength as needed.
Consider how color can elicit emotion, which can result in either negative or positive feelings. A vibrant red, for example, makes a design element more stimulating and is good for drawing attention, such as for a call to action button. Red, on the other hand, can have more negative connotations – red for danger. It’s also a difficult color to see, especially for those who are visually impaired. If you choose to use red in your designs do so sparingly and intentionally.
4. Make Good Use of White Space
This tip is all about learning to embrace white space in your design template. Make use of grids when laying out your design. Layout grids help designers position text and images in a way that looks coherent and easy to follow.
5. Adapt Your Images To Suit Each Social Platform
No one post fits every platform. Each social network has its own dimensions and your design needs to be adapted to fit. An image creation tool like Canva makes it super easy to create your image according to the dimensions of your chosen social channel.
6. Avoid Using Stock Photos
The best images to create connections online are authentic images. Try as much as possible to use your own photos and images in your design. That’s not to say you can’t ever use stock images, but be mindful of not turning to over-used, cheesy stock images.
Ten Tools To Create Professional Looking Graphics
1. A Color Story
This app lets you choose from a large selection of filters to make your photos stand out. Instead of filtering your photos to look all the same, A Color Story filters aim to enhance the color you’ve chosen in your composition. One very helpful feature of the app is that it lets you save your editing steps to reuse for future edits, which will save you time when batch-editing photos.
2. BeFunky
There is so much you can do with this tool to enhance your visual assets, including creating collages, adding “one-click” photo effects (there are over 300 photo effects and filters to choose from), and an array of graphics (e.g. speech bubbles). The basic account is free to use and provides users with access to a library of 125 digital effects.
3. Canva
Whether you want a Twitter post or Facebook profile picture, you can create them quickly using Canva’s drag and drop editor. Select from a number of pre-set designs, or create something from scratch.
Canva.com
4. Easil
Easil is an online graphic design tool with pre-made templates that you can adapt in seconds with simple drag-and-drop tools. It’s especially useful for Instagram and Facebook stories.
easil.com
5. Infogram
Infographics are a great way to present your data in a creative way and this free design tool makes it super simple to put together your own infographics.
6. Life of Pix
Life of Pix offers free, high-quality images that are available for personal and commercial use. Each comes with a helpful color palette so you can plan your visuals accordingly.
7. Quotes Cover
Quotes Cover turns quotes or short text into images for social media and high-resolution images for posters or other print designs. It’s so simple to use. Simply enter your quote or text and then choose your preferred design elements, such as font, shadow effect, and color.
8. Ripl
A mobile app that lets you create short animated videos with professionally designed templates. Ripl is integrated with the major social media platforms, so sharing your final video is easy. Once you’ve connected your social profiles to Ripl, you can post directly to Facebook, Facebook groups, YouTube, LinkedIn, and more. You can export your videos if you want to use them outside of your social media platforms.
9. Typito
Typito allows you to make video content using its drag and drop tool, and add images, music and captions. Once you create your video you can export it into several formats, including landscape, square, etc. — giving you perfectly cropped videos for the platforms you use the most.
10. Unsplash
Unsplash gives you access to a bank of 50,000+ free-to-use photos. You can subscribe to receive ten new images every ten days directly into your inbox.
Here’s to your social media success!

A Stanford Medicine X e-Patient scholar, Marie Ennis O’Connor is an internationally recognized keynote speaker, writer, and consultant on global trends in patient engagement, digital health and participatory medicine. Marie’s work is informed by her passion for embedding the patient voice at the heart of healthcare values. She writes about the experience of transitioning from breast cancer patient to advocate on her award-winning blog Journeying Beyond Breast Cancer.
What Role Can Care Partners Play in Advocacy?
What Role Can Care Partners Play in Advocacy? from Patient Empowerment Network on Vimeo.
Care partners can play many roles in advocacy. Diahanna, Sherea, and Patricia discuss that as a care partner you have to stay knowledgeable and up to date about various treatments and discussions happening in your loved one’s disease area. Diahanna shares a time where she had to advocate for her late husband by speaking up to the nurse and nearly saving her husband’s life. She also expresses that as care partners, you cannot be afraid to ask questions on behalf of your loved one.
Care Partner Tips for Communicating with Healthcare Teams
Care Partner Tips for Communicating with Healthcare Teams from Patient Empowerment Network on Vimeo.
Ensure that you are in a position to ask the right questions of your healthcare team. Diahanna suggests familiarizing yourself with various online resources so you are aware of the potential needs of your loved ones. Watch as care partners, Diahanna, Sherea and Patricia share more crucial tips to help others communicate with one’s healthcare team.
Resources for New Care Partners
Resources for New Care Partners from Patient Empowerment Network on Vimeo.
Sherea explains that you cannot move forward, unless you are able to acknowledge all the feelings that may come with the initial diagnosis of your loved one. Watch as care partners Diahanna, Sherea, and Patricia also share their tips and go-to online resources for new care partners.
Is There a Difference Between Care Partner vs Caregiver?
Is There a Difference Between Care Partner vs Caregiver? from Patient Empowerment Network on Vimeo.
The term caregiver is generally more recognized around the world. Care partners Diahanna, Sherea, and Patricia share that being a care partner is generally more intimate than being a caregiver. Care partners are those who are taking care of family members and loved ones whom they’ve known before any initial diagnosis.
How to Seek Help as a Care Partner
How to Seek Help as a Care Partner from Patient Empowerment Network on Vimeo.
When in need of help care partners Diahanna, Sherea, and Patricia share that you should not be shy. There is a tendency for care partners to deny help, but if you are burned out while caring for a loved one you are no good for them or yourself. Diahanna explains caregiving to be a very humbling and rewarding experience.
What Should Healthcare Providers Know About Care Partner Burnout?
What Should Healthcare Providers Know About Care Partner Burnout? from Patient Empowerment Network on Vimeo.
Care partners are often able to fill in any gaps at appointments with their loved ones. Sometimes information at a visit can go in one ear and out the other for a patient as it can be a traumatic experience. Care partners Diahanna, Sherea, and Patricia discuss that providers should know that burnout is real and it is important to not only discuss the needs of your loved one, but discuss your needs as well.
How an MPN Care Partner Handles Burnout
How an MPN Care Partner Handles Burnout from Patient Empowerment Network on Vimeo.
MPN Empowerment Leads Summer and Jeff discuss care partner burnout. Jeff is the caregiver of Summer who is living with myelofibrosis. Jeff admits to doing majority of the research so he can properly advocate for Summer’s care. In this video, Jeff talks about various outlets he uses to counteract burnout such as photography, music and improv theater.
Want to connect with Jeff and Summer? Email them at question@powerfulpatient.org or text EMPOWER to (833)213-6657.
Transcript
Summer:
Wake up. I’ve finished making your bonbons, Jeff. You said you wanted these.
Jeff:
Thank you, Summer. Mmm.
Summer:
Is it delicious?
Jeff:
It’s delicious. Just what I needed.
Summer:
Well, I’m glad I could please you.
Jeff:
Well, I’m Jeff.
Summer:
I’m Summer.
Jeff:
And we’re your MPN Network Managers for the Patient Empowerment Network. We’re here to talk to you today about…
Summer:
What caregivers do, and sometimes caregivers might get burned out. So, we’re talking about what you can do periodically to not get burned out, to keep going, and being great like you are. What are some of the main things you do, Jeff?
Jeff:
Well, I…one of the main things I do is try to remove myself from worrying about myelofibrosis and Summer’s disease. And I go out into nature and I take a lot of nature pictures. I go to National Parks, and take pictures of scenery, beautiful scenery, and big mammals and stuff, which I really really enjoy doing. It sort of clears my head and really refreshes me. I recently took a trip, as a matter of fact, to Yosemite. That’s one of the things I do.
Summer:
And another thing has to do with music.
Jeff:
Yes, I love music and I play in a band. I play the keyboard and the guitar, and I do that once a week at my church and I really really…again it requires quite a bit of focus and it puts my mind in a completely different place. So I remove myself from the worries, is one of the things I do. I’m very fortunate because Summer is doing quite well and doesn’t need huge amounts of physical care.
Summer:
Right, but you do all of the medical stuff because I can’t stand to hear about medical stuff, it’s boring.
Jeff:
That’s right. I do do a lot of the research and keep up with what’s going on in the myelofibrosis area and that’s kind of what my portion of the caregiving is. We’ve talked before about working with, dealing with these disease requires a team approach: the patient, the caregiver, and the medical team.
Summer:
Right.
Jeff:
It’s very important.
Summer:
And we also do improv. That really helps.
Jeff:
That’s correct. We’ve mentioned before that we run a small theater, and one of the things we do in the theater is improvisational theater. We make things up, now you’ve got to be in the moment, so your head can’t be disclouded and worrying about other things. It takes your mind off of the disease, and in my case, worrying about Summer’s disease and the caregiving responsibilities. So that helps us. It actually helps both of us a lot.
Summer:
Right. So do you want any more bonbons or is that a no?
Jeff:
I’ll just take another bite. You know, if we keep going like this, you could become the caregiver and I’ll be the patient. So until next time, I’m Jeff.
Summer:
I’m Summer.
Jeff:
Bye!
Summer:
Bye!