Patient Profile: Alexis Chase, PhD
Patient Profile
Alexis Chase, PhD
“To be empowered you have to be open, to want to do it, and to accept where you are.” – Dr. Alexis Chase, An MPN Empowered Patient
Dr. Alexis Chase has had a pretty interesting life, but she doesn’t think that makes her unique. She says she thinks all women have interesting lives. Born congenitally blind in her right eye she was given the name Alexis Elizabeth Lucia Chase. “I’m very proud of my name,” she says explaining the origin. Alexis was the name of a doll her mother had as a girl, and it means protector of mankind. Elizabeth is a family name, and Lucia represents Saint Lucia, the patron saint of the blind. Her mother was a nurse and her father, who was the first to recognize she had a vision issue, had a degree in biology. She was very close with her parents who instilled in her a strong foundation in her Roman Catholic faith. While she was born in Connecticut, she spent most of her adult life in Georgia as a divorced mother who built a successful 27-year career in the prison corrections system. She worked her way up to warden and earned two PhDs, one in religious counseling and one in criminal justice and corrections. After her retirement she became an international advocate and consultant of gender and women’s rights issues that include vocational training, post-incarceration reintegration, and female prisoners with children. She has travelled as far as Afghanistan in her advocacy work, and she is also the proud nana to a cat named Nathan Edgar Chase. She’s done a lot, and much of what she’s accomplished, she’s done while living with cancer.
The first time she was diagnosed with cancer was in 1976. She was in the first trimester of a high-risk pregnancy when she was diagnosed with ovarian cancer. Her doctors thought it would be best to terminate the pregnancy, but she refused. She was determined to have the baby, her daughter, and as soon as she was born, Dr. Chase began treatment for her cancer, opting for an experimental drug that she says saved her life.
At the time, her parents, her desire to live for her daughter, and her strong faith gave her the support she needed. “They were right there with me,” she says of her parents who she is grateful to for her faith. “It’s my great equalizer. My rope of hope,” she says and adds that she can pull on her faith anytime and in any place. “You’ve got to believe in something greater than yourself because definitely we’re not it,” she says.
She’s had no recurrence of the ovarian cancer, but in 1996, during a regular wellness checkup, she was diagnosed with myeloproliferative neoplasms (MPNs), a group of blood cancers that affect the function of bone marrow and can cause a number of complications. In Dr. Chase’s case her MPNs includes iron deficiency, anemia, diseases of the blood and blood forming organs, and hypothyroidism. MPNs are chronic conditions that can transform into another blood cancer and can affect people at any age but are more common in older adults. MPNs are also progressive. Dr. Chase had no symptoms for the first four years after her diagnosis, and wondered if she’d been misdiagnosed, but in 2000 she says she just started to feel like something wasn’t right and that’s when her blood counts started to change. She began taking medication, but in 2020 it stopped working and her cancer team worked to find other medications and therapies to treat her.
MPNs are rare and she doesn’t know anyone else with the same diagnosis, but she says she has an incredible support network through her daughter, her friends that are like family, her church, and her cancer team. “They take great care of me,” she says, but she also takes great care of herself. In fact, she’s very meticulous about taking care of herself. She carefully takes her medications, and she makes herself a priority. She focuses a lot on her mental health and she stresses the importance of mental health for all cancer patients. She says she finds three ways to laugh at herself every day and she chooses six words every day that represent how she’s doing and to help her feel empowered. A recent example, “I feel surrounded by grace today”. Also, part of her self-care is taking the time to listen to calming and soothing sounds and inspirational messages and quotes.
She says it’s a blessing to have the cancer she has because she is able to handle it and it makes her take time to smell the roses. She’s handled it so well that during her career as a prison warden she never let on that she was sick. She managed to schedule her appointments around her work so no one would know. She didn’t want her illness to affect her career.
Always an empowered patient, she’s been known to walk out of a doctor’s office when a situation doesn’t feel right. “It’s important for people to feel like they are being heard and more importantly that they are being listened to.” She says “It’s also important to know what’s going on with your care. You know your body better than anybody.” Dr. Chase likes the Patient Empowerment Network (PEN) because of the resources it provides to help others feel empowered in their own care. “I found PEN and love that I can access it anytime,” she says. She feels it’s important for patients to take charge of their own care plans. “To be empowered you have to be open, to want to do it, and to accept where you are,” she says. Her recommendation to other patients is to read, and comprehend, everything they can about their illness. “If you don’t understand it, you need to have someone explain it to you,” she says and also recommends keeping a journal. “We have to have something tangible. We can’t remember everything.”
While she continues to accomplish a great deal while living with cancer, it’s not always easy. “The chronic cancer fatigue, it will get me. I fight it because I feel like once I give in it would overtake me,” she says. She does experience shortness of breath and plans her days around her energy level. “It slows me down, but I don’t let it stop me. I push myself because I know the next day or the next day I won’t be able to.” Along with continuing her consulting and advocacy work, Dr. Chase loves to travel and hopes to go to Turkey to see the Virgin Mary’s house. “You never know what God has laid out for you,” she says. “I’m still here. I’ve been symptomatic for 20 years and I’m still here.”
Read more patient stories here.
Jennifer Lessinger is a professional writer and editor who learned the value of patient empowerment during her struggle with a hard-to-diagnose and complex endocrine disorder.

 “It feels so good,” I said during our telemedicine appointment, “to be away from the hospital for eight weeks in a row.” It’s the longest hospital break I’ve had since being diagnosed with cancer last summer. Before mid-March, I’d been to four to ten medical appointments every month. Being a cancer patient felt like a full or half time job. Because of the pandemic, I’m now treated by my oncology team from the comfort of my own home.
“It feels so good,” I said during our telemedicine appointment, “to be away from the hospital for eight weeks in a row.” It’s the longest hospital break I’ve had since being diagnosed with cancer last summer. Before mid-March, I’d been to four to ten medical appointments every month. Being a cancer patient felt like a full or half time job. Because of the pandemic, I’m now treated by my oncology team from the comfort of my own home.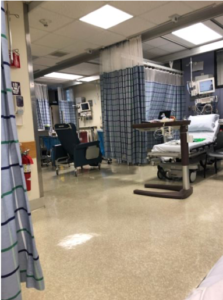 My partner drove me to the hospital on the morning of my surgery. We checked in before 6a.m. and waited, with others, in the lobby.
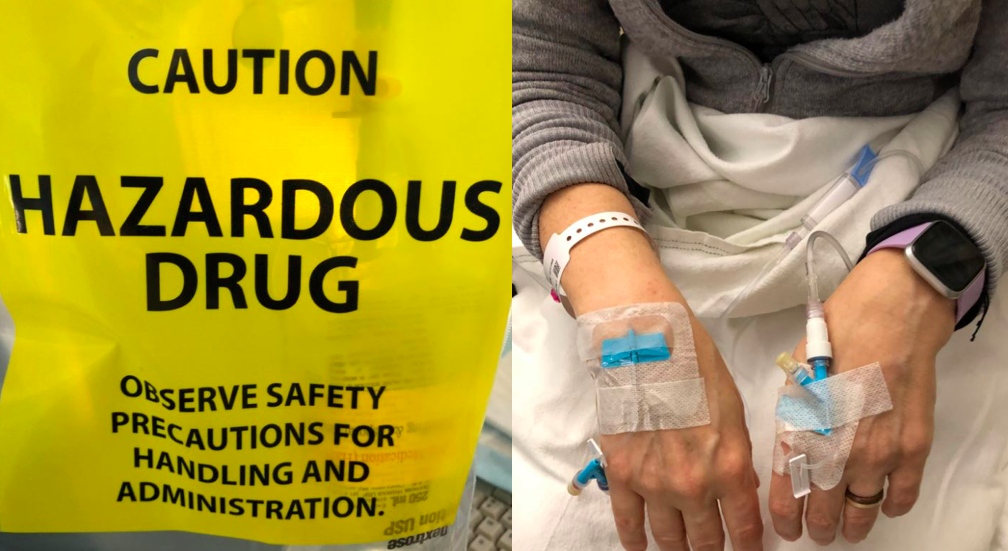
My partner drove me to the hospital on the morning of my surgery. We checked in before 6a.m. and waited, with others, in the lobby. This is me in post-op. My partner took this photo on his phone and was able to share it with my family and friends to let them know I made it through surgery. They were worried because it went hours longer than expected.
This is me in post-op. My partner took this photo on his phone and was able to share it with my family and friends to let them know I made it through surgery. They were worried because it went hours longer than expected. Going home after surgery is comforting and scary. My right leg was giving out from under me because my obturator nerve “got heat” during my surgery. I had trouble standing in the shower or lifting my right leg onto the bed or into a car. I had extensive swelling and bruising on my right side and pelvic area and had a bit of a reaction to the bandage tape. I didn’t know what was normal. And after a phone call to the hospital, I was asked to come back in for a check-up.
Going home after surgery is comforting and scary. My right leg was giving out from under me because my obturator nerve “got heat” during my surgery. I had trouble standing in the shower or lifting my right leg onto the bed or into a car. I had extensive swelling and bruising on my right side and pelvic area and had a bit of a reaction to the bandage tape. I didn’t know what was normal. And after a phone call to the hospital, I was asked to come back in for a check-up.