MPN Patient Profile: Robyn Rourick Part 2
Read the first part of Robyn’s MPN journey here…
Picking up after 26 years of watchful monitoring of her myeloproliferative neoplasm (MPN), scientist Robyn Rourick was then referred for an allogeneic stem cell transplant by her MPN specialist, Dr. Gotlib. The transplant team started working through the matching process for a bone marrow transplant donor, which often begins with close biological relatives. Although Robyn’s only sibling wasn’t a transplant match, a person considered a near perfect transplant match for Robyn was found.
At that point in her journey, the possibility of entering a Phase II clinical trial called ORCA-1 was presented by Robyn’s transplant doctor. She discovered that the ORCA-1 treatment had the potential to completely eliminate graft-versus-host disease (GVHD). The clinical trial made sense to her. In Robyn’s trained scientific mind, she agreed that the trial was founded on sound scientific rationale with the potential for clear benefit and signed up for it. She researched other things like whether the transplant team could look at biomarkers to guard against graft-versus-host disease, but she decided to take the clinical trial path as her best option.
As for her feelings about the stem cell transplant, Robyn felt there was likely going to be a positive outcome for her due to the ORCA-1 clinical trial. Her knowledge about the trial really brought her a lot of comfort and put her at ease for the time she’d be around her family post-transplant. Robyn was lucky because her doctor was actually the primary investigator on the study. When he presented the transplant study as an option, that’s when she started to do more searching to find what patient advocacy groups were out there.
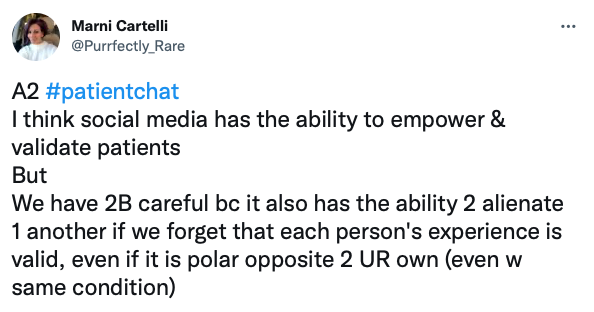
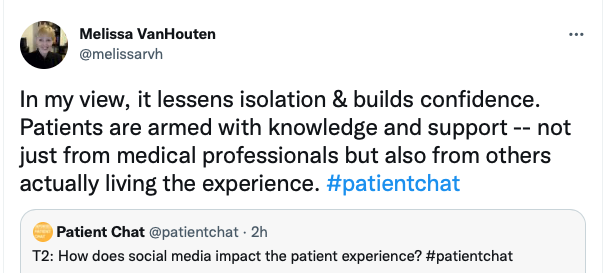
Looking back on her MPN journey, Robyn wishes that physicians would provide their patients with more patient advocacy resources, such as those available through organizations like Patient Empowerment Network (PEN). She feels fortunate that she discovered PEN through another patient advocacy website, and she firmly believes in PEN’s mission of empowering patients to gain knowledge to advocate on their own behalf. “I had the realization that in the clinical trial I was in, I was only the sixth patient, and the technology was stellar in terms of what we’re trying to do in terms of cell therapy. I just felt like patients need to know about the treatment advancements, and PEN is an excellent resource for learning about treatment and support options that I wanted to share my knowledge and patient experience with.”
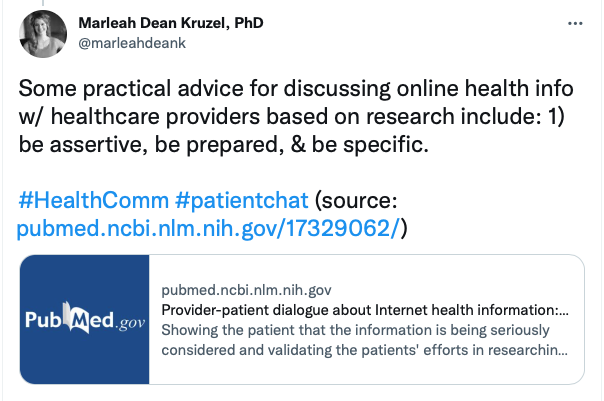
Robyn was fortunate to have a team of physicians in whose knowledge and treatment recommendations she could trust. She’s tremendously grateful, because she knows it’s not always the case, and so offers this advice for others, “Make sure that you’re comfortable with your physicians. And if not, then move on. Don’t be afraid to reach out and to make other connections to other doctors, even across the globe. You shouldn’t hesitate to request a conference call with another provider to see if they’re aligned with your diagnosis and your watchful waiting or treatment recommendations. Patients must have the utmost confidence going through their cancer journey.”
As for the scientists who handled her sample in the ORCA-1 trial, Robyn was able to meet the scientists and saw the analytical data of her sample. She was highly impressed with the protocols that they used with the samples. Robyn was just the sixth myelofibrosis patient to join the trial. To have spent her life working on medicines for patients and then to be on the receiving end of this cutting-edge treatment for transplants made her feel very privileged.
In her life post-transplant, Robyn has continued periodic blood work for routine monitoring and has been doing well. Two years following her transplant, Robyn’s myelofibrosis is in remission, and she has no evidence of fibrosis in her bone marrow. Her test numbers have been progressing nicely, and she hasn’t needed any additional treatment since undergoing the transplant. “I don’t have a single regret. I haven’t had a pimple, an itch, a scratch, absolutely nothing. My life has resumed exactly how it was before the transplant.”
In reflecting on her patient experience, Robyn offers this additional advice to other cancer patients, “Take a deep breath and give it some time to play out. The moment that I heard the word cancer and the risks with rapid progression, I had myself dead and buried. In my mind, what I needed to plan for was death. Prepare my family. Get everything in order. And to me, that was going to be the ultimate outcome. But then as things unfolded, I had conversations, did a little bit of research, and found out I did have some options. Things weren’t so negative in terms of progression and mortality. Don’t jump to the most negative outcome possible.”