What Do MPN Patients Need to Know About Clinical Trials?
What Do MPN Patients Need to Know About Clinical Trials? from Patient Empowerment Network on Vimeo.
What is a clinical trial and how does patient participation work? This animated video provides an overview of clinical trials, the process, and details key steps for engaging in your care.
See More From MPN Clinical Trials 201
Related Programs:
|
|

Clinical Trials As an MPN Treatment Option: What You Should Know |
Transcript:
Brian:
Hi, I’m Brian and this is my doctor, Dr. Liu.
I have myelofibrosis, which is a type of myeloproliferative neoplasm, or MPN as it’s commonly referred to.
And when discussing therapy with my doctor. She suggested a clinical trial might be my best treatment option. Dr. Liu, can you please explain what a clinical trial is?
Dr. Liu:
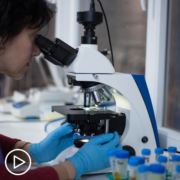
Absolutely. In basic terms, a clinical trial is a research study that involves human volunteers. The goal of cancer clinical trials is to discover new and improved approaches to prevent or treat the disease.
There are typically four phases of a trial. Each phase gathers valuable information about the treatment and helps measure its effectiveness1.
But, Brian you had some hesitations at first, right?
Brian:
That’s right. Although I trusted your advice, I definitely had questions about the process.
One thing I worried about was safety. I asked Dr. Liu how I would be kept safe if I participated in a clinical trial.
Dr. Liu:
I hear this concern a lot from patients. But every trial has a strict safety protocol, with set guidelines in place to protect patients.
Additionally, researchers must follow patient safety rules, which are regulated by the U.S Food & Drug Administration (the FDA). And an institutional review board (or IRB) regularly reviews a study at each study location. Plus, many trials are overseen by a group called a data and safety monitoring committee2.
Finally, there is also a clinical trial team that can include healthcare team members like cancer researchers and oncology nurses. This team regularly observes the health of each participant, through each stage of the process. Because of this, trials often involve more testing and visits, which can be a bigger commitment for a patient.
Brian:
When Dr. Liu explained the safety measures, it helped me feel more confident in the process and comfortable about participating. So, then I asked which trial she would recommend for my individual disease.
Dr. Liu:
It’s important to note that every trial has “eligibility requirements” that include things like a patient’s age, health, and prior treatments they have received. These requirements determine whether a patient qualifies for a trial.
We talked about which trials may be a good fit for Brian and discussed the pros and cons of each one. We also reviewed the logistical and financial impact the trials could have on his life.
Brian:
That’s right. Dr. Liu also pointed out that patients can leave a trial at any time–for any reason– once they have enrolled.
Dr. Liu:
That’s right—participation is completely voluntary.
Brian:
One of the main reasons that I joined a trial was because I wanted to find out if a treatment in development would be more effective in treating my cancer. AND I wanted to help advance research forward, so I could help the MPN community.
Dr. Liu:
Right, Brian. Patients may have different reasons for participating, but trials are the only way to develop and study new and improved treatments for MPNs.
Now that you understand more about trials, how can you find out more?
- Start by asking your doctor if there are any trials that you are eligible for.
- If there is a trial that your team recommends, ask to discuss:
- The treatment approach used in the study and the purpose of the trial.
- The risks and benefits of participation.
- The financial costs, if any, and if there are assistance programs to help if you need it.
- The location of the trial and whether it can be coordinated with your local institution if it isn’t conveniently located—or if transportation is available.
- And, how often you will need to visit the trial site and how long the trial will last.
- Finally, continue to educate yourself, using resources like clinicaltrials.gov.
Brian:
We hope you found this information useful! Visit powerfulpatients.org/MPN to learn more about clinical trials and MPN research.
Dr. Liu:
Thanks for joining us!