Tips for Patients on Staying Connected Despite Physical Distancing
We are in a crazy time right now, and no one has experienced anything like it…except for cancer patients. As high-risk patients, we know what it’s like to distance ourselves from others and practice good hygiene. I know I do.
As a thyroid cancer patient, I underwent radioactive iodine treatment, where I became radioactive. I was living with my family at the time, and I had to have my own room and bathroom. No family member could come within a certain distance from me. Not even my dog. I remember them leaving meals outside my door, and texting a parent or sibling when I needed something. It was strange, yes, but I knew it was what I had to do to keep myself and my family safe.
The same thing is happening right now. We’re told to stay at least 6 feet apart from people at all times. Performing normal tasks such as going to the grocery store, a friend’s house, and even work are no longer possible. It creates a sense of grief in all of us, as we feel lost without our normalcy. Instead, we are living a “new normal,” something that cancer patients have already been long accustomed to. It’s as if the rest of the world gets to see how we live, how we feel.
We may have to physically distance ourselves, but staying connected is still possible. And it is in these moments that we can learn how to cultivate strong relationships. We live in a world with an abundance of technology. We have the ability to call, text, email, video chat, Tweet, etc. Had this pandemic happened a long time ago, none of this would’ve been possible. Social distancing would be real.
To take advantage of the opportunities that are currently presented to us, I’d like to highlight the ways in which we can stay connected:
(NEW!) Virtual Empowered #PatientChat | Friday, May 15 @ 1PM EDT
The Virtual Empowered #PatientChat is a moderated conversation conducted online via Zoom and Facebook Live. This support group will feature an expert moderator, a panel of passionate patient advocates and care partners, and other people seeking a consistent friendly community. Learn more and register!
Support groups via Zoom
- Our Odyssey
- Smith Center – for AYA patients (located in the Washington, D.C. area but is open to patients all over)
- Look for ones from specific cancer orgs (ex. Thyca, Inc.)
Facebook support groups
These can be found for cancers from the general (ex. breast cancer) to the specific (ex. breast cancer with BRCA1 mutation)
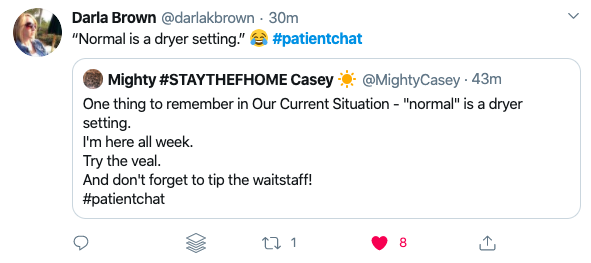
Tweet chats
Search for these using the hashtag as seen below. A few of my favorites include:
- #patientchat
- #ThyCaTalk
- #bcsm
- #HealtheVoicesChat
- #medtwitter
- #HCLDR
Carly Flumer is a young woman who was diagnosed with stage I papillary thyroid cancer at the age of 27. She recently received her Master’s degree from Boston University in Health Communication and received her Bachelor’s from George Mason University in Health Administration and Policy. While being diagnosed with the “C” word at such a young age was a surprise, as it would be to anyone, she found strength, support, and inspiration in sharing her cancer journey on social media. As a result of her health outcome, she looks to advocate for other cancer patients through education, research, and health literacy.