Metastatic Breast Cancer Treatment and Research News
Metastatic Breast Cancer Treatment and Research News from Patient Empowerment Network on Vimeo.
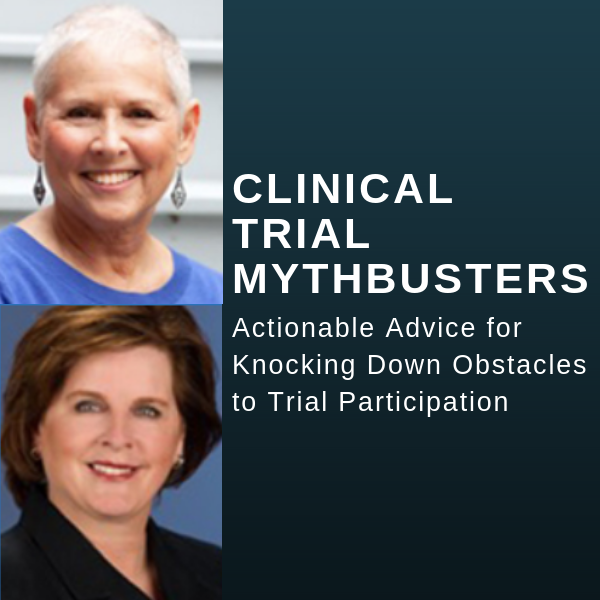
As metastatic breast cancer testing approaches continue to expand, new and promising treatments have emerged. Dr. Lisa Flaum shares information on recently approved treatment options and the role of genetic markers in accessing targeted therapy.
Dr. Lisa Flaum is a Medical Oncologist at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. Learn more here.
See More From The Pro-Active Breast Cancer Patient Toolkit
Related Resources:

|
Essential Testing Following a Metastatic Breast Cancer Diagnosis |
Metastatic Breast Cancer Treatment Decisions: Which Path is Best for You? |
Transcript:
Dr. Flaum:
There are a lot of new and promising treatments for metastatic breast cancer. So, the treatments in general and the novel treatments and studies really vary based on the subset of metastatic breast cancer. So, when we’re making our treatment decisions, a lot of it is defined by those markers. So, if someone has a tumor that is hormone receptor, estrogen and progesterone receptor positive, and HER2-negative, the mainstay of treatment is typically drugs that target estrogen and often partnering drugs that target estrogen with other more novel or newer treatments.
So, just in the last five plus years, there have been a number of new drugs and even new drug categories that we didn’t have previously. So, for that population of the estrogen receptor positive tumors, the biggest breakthrough over the last number of years has been a class of drugs called CDK4/6 inhibitors. So, that includes drugs like Ibrance, Kisqali, Verzenio. And they’ve emerged as a very important and effective and often a recommendation for our first-line treatment for these patients combined with anti-estrogen therapies that have vastly improved outcomes for patients. So, a much higher percentage of patients respond to these drugs, the duration of the responses has extended quite a bit. And importantly, patients tend to tolerate this drug class really, really well.
So, for many patients starting out with that diagnosis, this type of drug class is going to be part of the discussion. Even in the last year, another drug category has emerged with approval of a new drug called alpelisib, which is something called at PI3 kinase inhibitor. So, again, back to defining the options based on the molecular profile of the tumor. So, this newer oral drug also partnered with anti-estrogen therapy, has been an important breakthrough for the treatment of patients who harbor this specific molecular abnormality. So, important to define whether that’s an option by some of these molecular testing.
There’s also newer drugs and studies of newer drugs that affect the estrogen receptor in different ways than some of our traditional medications.
And this is an ongoing area of significant research. So, that’s the estrogen receptor positive tumors.
For patients who have HER2-positive tumors, these are tumors that tend to be more aggressive, that tend to require more aggressive upfront treatment, which usually involves drugs that specifically target HER2. So, again, defining what’s driving the tumor and hopefully having drugs available that can target that specific abnormality. So, HER2 targeted drugs have evolved quite a bit over the last couple of decades.
Initially, we just had a drug called Herceptin and then a drug called Perjeta or pertuzumab was developed. Then more recently a drug called Kadcyla. And then even in just the last six to 10 months, two new drugs that target that HER2 protein. One of them is called tucatinib, the other one is called Enhertu. They’re not necessarily appropriate for the first line of treatment, but really sort of expands our toolbox in terms of how we treat these types of tumors. And these are developments that have occurred, for one of the drugs, just in the last six months, and the other within the last year. So, a lot of progress.
And then for the third subset of tumors, which are the triple-negative tumors, those are the ones that do not over-express estrogen, do not have estrogen or progesterone receptors, and don’t overexpressed HER2. This has been historically an area of unmet need. So, tumors where we can’t use anti-estrogen therapies, we can’t use HER2 targeted drugs. And so, the main stay has always been chemotherapy. And even for this subset, we’ve had progress.
So, one of the drug classes that’s been approved in the last couple years for triple-negative breast cancers is immunotherapy. So, immunotherapy has gotten a lot of press. It’s been really breakthrough treatment for a lot of different cancers, has lagged behind to some degree in breast cancer, but has become now one of the early treatment options for people with metastatic disease, specifically those that harbor a molecular marker, an immune marker, something called PD-L1. So, another example of the tumor’s biology dictating potentially one of the treatment options.
There have been other drugs that have been approved for triple-negative breast cancers in women who have BRCA mutation, so who have germline genetic predisposition to breast cancer. And that opens another array of treatment tools that have been approved in the last few years. And then more recently, just over the last six months, another drug that’s been approved for triple-negative breast cancer, which is a drug called sacituzumab, again, not first treatment, but something that defines potentially future lines of treatment. So, big picture, there has been a lot of progress that increasingly alters our treatment tools for patients and allows us to have sequential treatments that can be effective if their given treatment is no longer effective.