12 Actionable Tips For Social Media Success in 2021
2020! What a year it was for all of us. In the advocacy world, we saw an unprecedented shift towards online activities. We relied on zoom calls, webinars and social networks to keep us connected and informed. Where many organizations and individuals may in the past have used social media as an add-on to in person events, this past year saw the virtual world take centre stage, and with it the need for a stronger social media presence.
I spent the latter half of 2020 teaching social media skills to more patient organizations than I have at any other time in the past decade. The realization that mastering social media has become an essential advocacy tool was brought home to us more than ever this year.
With hope on the horizon that vaccination may bring us closer to something resembling normality again, it is yet unclear how long it will take before the old way of doing things resumes. It is predicted that for 2021 at least we will still be relying heavily on online activities in the advocacy world.
To help you strengthen your online presence and create more visibility for your cause in the new year, I’ve put together this list of 12 actionable tips you can put into practice over the coming months. By following these monthly prompts I predict that come this time next year, you will be able to look back with satisfaction on all you’ve achieved over the previous 12 months.
January
Set SMART Social Media Goals
Get your 2021 social media activities off to a flying start by setting some SMART social media goals for your online activities.
Goals are the forerunner to success. Ask yourself what you would most like to achieve with social media this year, and then set specific and actionable goals to achieve it. For a goal to become a reality it needs to be specific, measurable, attainable, and realistic, as well as time specific. These are often called SMART goals.
February
Conduct a Social Media Audit
Take some time this month to audit your social media activities. A social media audit is a great way to take stock of where you’re at and identify what you can improve on going forward.
Start by creating a simple spreadsheet and list all your social accounts, including those you set up but haven’t used in a while. Audit how often you are posting on each platform and list which times you are posting and the results you are getting. How engaged is your audience with you on each of your social networks? It’s a good idea to benchmark where your social activities are at so that when it comes to the end of the year you can look back and see what has worked for you.
Some further things to audit:
- Have you fully completed your About sections on each network?
- Are your biographical details up to date?
- Do you need to include a new call-to-action?
- Do your cover photos needed updating? Are you still showing that summer picture now that it’s winter?
Want to dive deeper? Download my step-by-step guide to conducting a social media audit at http://bit.ly/3pvjVa5
March
Perform a Content Audit
Look back at your ten most recent pieces of content — blogs, images, videos, etc. Which content worked best for you in terms of engagement (i.e. comments, shares, etc.)? Can you do more with this content? For example, can you highlight some key statistics and share on social media in a more visual format?
What about the content you spent a lot of time creating which didn’t generate significant engagement? Ask yourself (or even better ask a friend) if it’s immediately clear what message you are trying to convey. Can you rework this content to make it more compelling – updating any outdated information, adding new research, refreshing images, etc.
April
Conquer Content Curation
The ability to curate credible content to share with our communities is a key skill for patient advocates. Hereditary cancer advocate, Amy Byer Shainman (@BRCAResponder) believes “patient advocates not only have a responsibility to curate trusted content but that it is an imperative if you are even going to be calling yourself a patient advocate.”
Content curation is defined as the process of gathering information relevant to a particular topic or area of interest. While this definition sounds simple, there’s a world of difference between simply gathering information and being an effective curator. A good curator knows how to find, aggregate, and synthesize reliable information, putting it into context for their communities and sharing it in a format that is easy to access and understand.
May
Develop an e-Newsletter
This month, consider developing an online newsletter. With the popularity of social media, you may think e-newsletters outdated, but nothing could be further from the truth. While you can go for a few days without checking social media, most people check their email several times a day. E-newsletters can help you build relationships and credibility and keep your activities to the forefront of people’s minds.
If you blog, use an e-newsletter to send a digest of your most recent blog posts. “I would advise anyone who wants to increase readership to her/his blog to consider sending out a monthly or weekly email with links to new posts and possibly one or two older ones,” recommends breast cancer blogger Nancy Stordahl (@nancyspoint). “I also share a couple of articles that have been in the news, or that I think might be of interest to my subscribers,” says Nancy. “Sometimes I share something personal and I often bounce around ideas. I love my subscribers and always value their input!”
Even if you don’t blog, you can still keep your subscribers updated with the latest research and news from the advocacy world by sending a regular e-newsletter. You can also share links to these newsletters on your social media channels.
June
Create Visual Impact
This month is all about getting creative with your visual assets. Visual content is 40x more likely to get shared on social media than other types of content according to research. Furthermore, people connect more emotionally with images than text, and in an increasingly crowded digital landscape images can break through the online content clutter. The type of visual assets you can create include images, videos, infographics, quotes and GIFs.
Check out my guide to creating professional looking graphics at https://bit.ly/3mYMzPe
Related: Patient Advocacy: 10 Ways To Create Share Worthy Content For Social Media
July
Build Your Authority on LinkedIn
Your LinkedIn profile is the cornerstone of your professional brand online. It’s so much more than a place to park your resume.
Take some time to identify how top patient advocates are using LinkedIn to build their thought leadership on the platform. You’ll find they are showing up consistently, publishing thought-provoking commentary and original think pieces and generating high levels of engagement with industry leaders. The wonderful thing about LinkedIn, as with all social media, is the ability to show up on a level playing field. The same opportunities to build online visibility are open to all – so take full advantage of this by doing more with your LinkedIn profile this month.
Start by optimizing your Linkedin profile at http://bit.ly/2wTorK3
August
Tap Into The Power of SlideShare
Many of us who do speaking engagements have built up our own library of slide-decks over the years. This month dust off those decks and upload them to SlideShare.
SlideShare is the world’s largest professional content sharing community. Surprisingly, given how the platform is optimized for social sharing, including the ability to embed presentations, it’s often overlooked and underused. And because it’s owned by LinkedIn, it’s super easy to highlight your uploads on LinkedIn’s platform – giving your thought leadership a further boost.
Take time to create visually impactful slides – even if this means re-doing some of your original slides.
Boring slides don’t get many views. Make sure to optimize for mobile viewers with big, bold visuals and text that is readable on mobile devices. New to SlideShare? Check out these tips: http://bit.ly/2XcrsyN
September
Increase Facebook Reach
Despite privacy concerns, Facebook still reigns supreme in the advocacy world. However there’s a problem when it comes to making an impact on Facebook. When organic Facebook Reach (i.e. the number of people who see your content without paid distribution) is estimated to currently be as low as 1–3%, succeeding on the platform is more difficult than ever. Take time this month to consider ways to increase your organic reach and boost engagement on Facebook.
Facebook recommends each post you create should include some type of creative, like images, GIFs or videos. Make sure these creative assets are high quality. Avoid using blurry images or videos or creative that doesn’t accurately reflect your message.
For more tips on increasing Facebook reach, go to http://bit.ly/3pydfIk
October
Get Creative with Instagram
When it comes to consistent engagement, Instagram (now owned by Facebook) is the number one social channel out there. Recent studies have found the engagement rate on Instagram Is 45% greater than on Facebook. Instagram is the perfect platform to let your creativity run free and, in fact, even have some fun in the process.
If you’re new to Instagram there is a lot to learn. Check out my SlideShare deck to help you get started: http://bit.ly/3rDBKph
November
Become a Twitterholic
Twitter is a powerful tool to help raise awareness of your cause, keep current with research, amplify your advocacy activities, and build collaborative relationships. Twitter thrives on its community and the more you connect with other users the more quickly you will grow your own following.
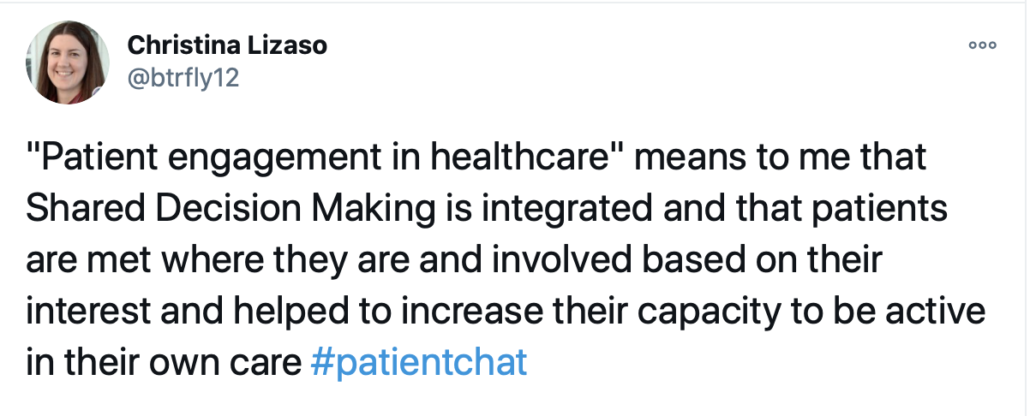
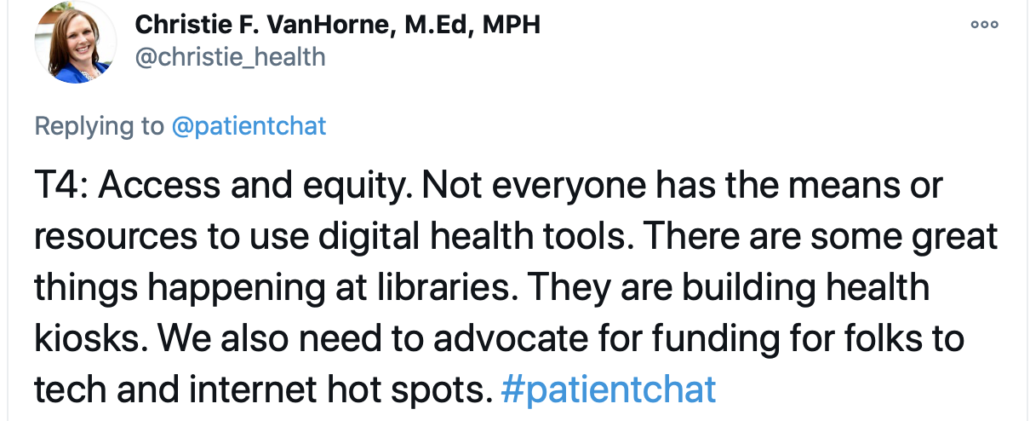
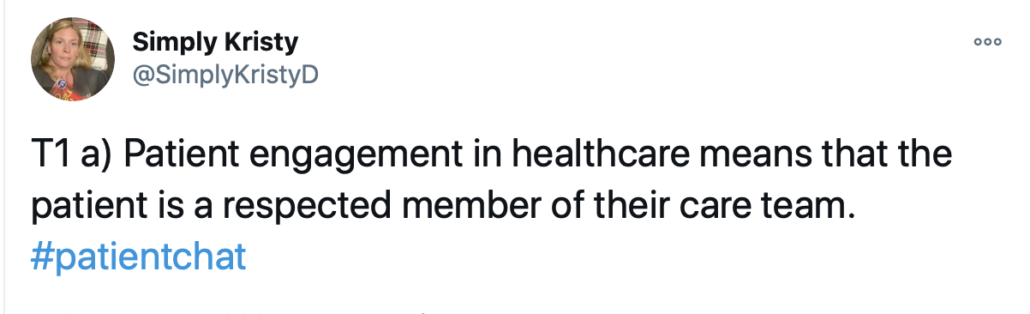
Joining a Twitter chat is a super way to connect and engage. When you attend a Twitter chat regularly, people will get to know you and in this way, you can quickly develop and grow your own network of supporters. Twitter chats can be one-off events, but more usually are recurring weekly chats to regularly connect people, for example #PatientChat held every other Friday at 10:00 am Pacific/1:00 pm Eastern.
Many people tell me they “don’t get” Twitter, but I would encourage you to give it a try. You don’t even have to tweet to take part – you can learn a lot from following the right people and listening.
December
Evaluate Your Progress
It’s the end of your social media year. Time to look back and evaluate how far you’ve come over the previous 12 months.
Some key metrics to track are the number of followers you attract and retain, which social media channels drive the most traffic to your website, the number of comments you get, and how many times your updates have been shared. Most social media platforms have their own basic measurement and analytics tools, which you can use to gain information about views and engagement. Take note of what’s working for you – do more of this – and consider dropping things that aren’t generating much engagement.
Here’s to your social media success!

A Stanford Medicine X e-Patient scholar, Marie Ennis O’Connor is an internationally recognized keynote speaker, writer, and consultant on global trends in patient engagement, digital health and participatory medicine. Marie’s work is informed by her passion for embedding the patient voice at the heart of healthcare values. She writes about the experience of transitioning from breast cancer patient to advocate on her award-winning blog Journeying Beyond Breast Cancer.