How to Create a Month’s Worth of Posts for Your Advocacy Blog
Are you looking for a way to boost your advocacy activities online?
One of the best ways to do this is to create a blog. Blogging shows your commitment and passion for your cause and because a blog is interactive, it’s also an extremely effective way to build a community and engage more people in your cause.
If you are brand new to blogging, and not quite sure how to start a blog, this step-by-step guide will get you up and running.
Many of us who blog start out with great intentions of writing regularly, but over time our inspiration well can run dry. Creating a blog is relatively easy; the challenge lies in consistently creating fresh content. Cancer blogger, Nancy Stordahl (@nancyspoint) recommends a consistent blogging schedule if you want to develop a loyal readership. “This takes commitment,” she explains, “which means posting on a regular schedule that works for you. This might be weekly, every other week or monthly. This way readers know what to expect, plus it keeps you focused. I post weekly (usually the same day) because that’s what works for me. Consistency is key.”
In this article, I want to share with you a month’s worth of things to write about. Whether you’re new to blogging and looking for ideas to get started, or you’ve been blogging for a while but your writing has stalled, the following tips are designed to kick-start your writing efforts. Commit to consistency by writing one blog post a week for the next month with these topic ideas as your guide.
10 Ways to Create a Month’s Worth of Blog Posts
1. Share Facts and Answer Questions for Your Readers
You might like to start by asking your readers what kind of questions they have that you can answer for them. You could use Instagram, Twitter or Facebook to do this or you could search on a question and answer platform like Quora. On Quora you can ask a question about your topic or simply do a search using your topic keyword to find what people are asking about that topic. Make a list of those questions which you feel you could write about. When you have written a blog post on the topic, go back into Quora and answer a question related to the topic. You can include a link to your post in your answer.
2. Recycle Old Posts
Recycling content simply means taking one piece of content and finding a new way to create content around it. Identify your most popular content through your blog analytics tool. Now brainstorm some ways in which you can take this content and turn into a fresh post. Can you turn it into a video or audio post? Are there any new research or treatment updates you can add since you first published this post? Can you get creative and create an infographic or develop a downloadable checklist using the original post as a starting point? You’ve already spent time and effort in creating your content, now spend a little more time to maximize that effort.
3. Compile a Glossary of Medical Terms
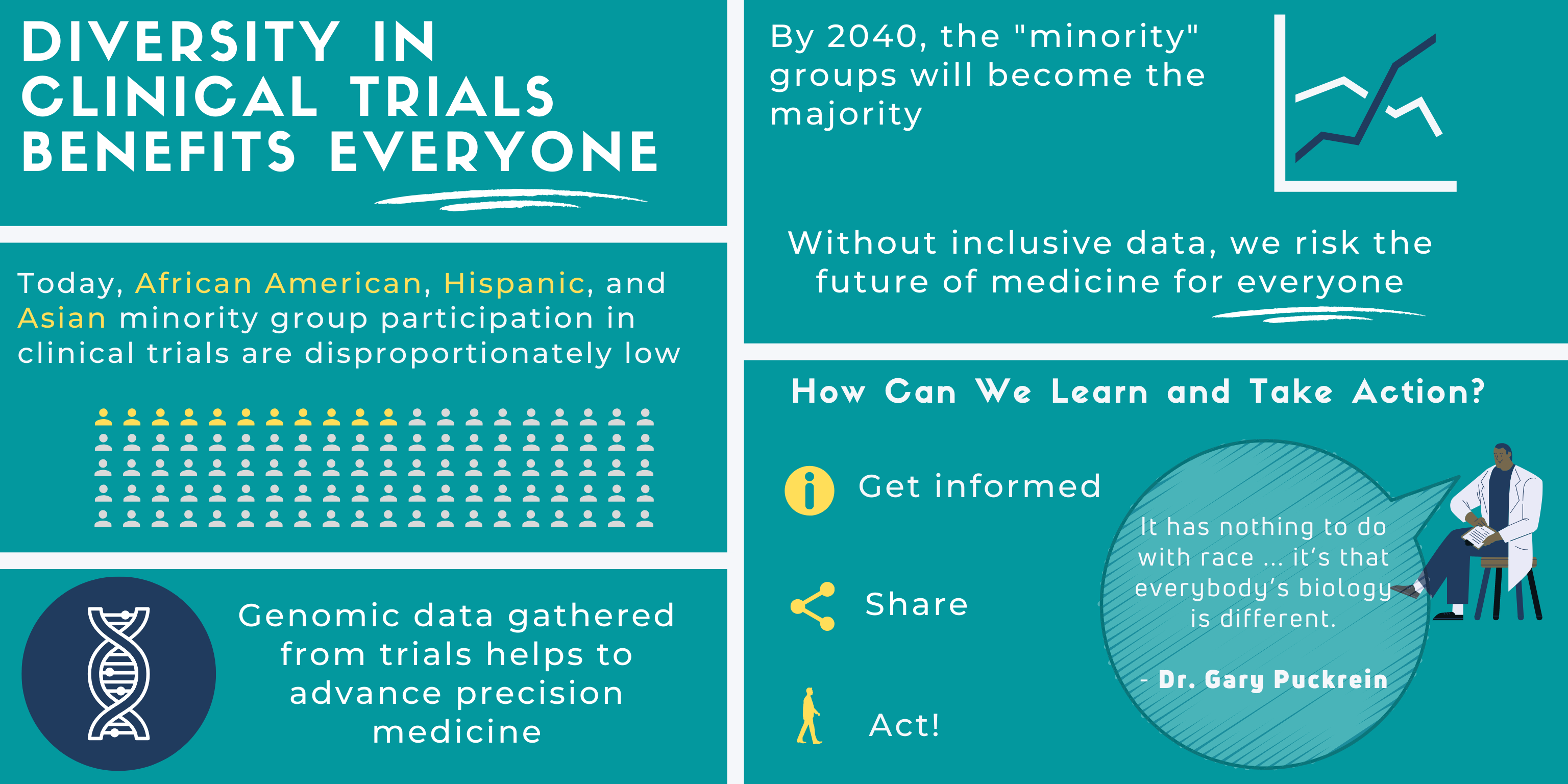
One of the things I remember most when I was a newly diagnosed patient was how mystifying the world of cancer was for me. I had to learn a whole new language consisting of unknown medical terms and scientific jargon to be able to understand my diagnosis. Make the process less mystifying for newly diagnosed patients by putting together a useful list of medical and scientific terms (as I did with this Clinical Trials Jargon Buster) and publishing it on your blog.
4. Share the Latest Medical Research in Your Disease Area
Have you been to a conference where you learned about new medical research? Or read about the latest research in a medical journal? Let your readers know about it through your blog by providing a summary of the key findings and translating the information into easy to understand language for other patients.
5. Create a Reader’s Poll
There are several online tools you can use to create a readers’ poll. If you have a WordPress.com site, then you’ve already got Polldaddy polls built in. You can create, manage, and see results for all of your polls directly in your WordPress.com dashboard. If you use a self-hosted WordPress site, install the Polldaddy WordPress.org plugin. Once you’ve collected your poll data, publish a follow-up post with your findings.
6. Write about a Typical Day in Your Life
What’s it like to live with your condition on a day-by-day basis? What insights can you share to help others understand what a typical day is like for you and patients like you? Can you share helpful tips to cope with common everyday difficulties? Do you have advice for how family and friends can help you navigate your illness? As a person with lived experience you are in a unique position to shed light on what it’s like to cope with your illness by writing about it on your blog.
7. Embed Slide-Decks of Your Talks
Have you recently spoken at an event? Did you use slides in your presentation? Did you know you can upload your slide-decks directly to a platform called SlideShare? This is a great way to develop a portfolio of your speaking work and showcase it on your blog by simply inserting the embed code provided by SlideShare.
8. Invite a Guest Blogger to Write For You
Inviting another patient or healthcare professional you admire to write for you, not only expands your blog’s reach and readership, but adds a valuable new perspective to your site. For example, each week, Nancy Stordahl invites a different metastatic breast cancer patient to share their story on her blog for her regular #MetsMonday post.
9. Create Recurring Content
Creating regular recurring content, like Nancy does with #MetsMonday, is another excellent way to keep consistent with your content creation. Another suggestion is to create a round-up post each week – this could be a round-up of the latest research or a link to useful resources and articles you think would be helpful to share with your readers. Pick a day for this and stick to that day each week so readers know what they can consistently expect from you.
10. Plan Posts around Seasons and Events
This final tip is one of the easiest ways to create content on your blog that you can use on a regular basis. For example a post on how to survive the holiday season, or healthy eating during the holidays is a post you can use year after year. Add the dates of awareness days, such as World Cancer Day, to your calendar as a reminder to create content around these events.

A Stanford Medicine X e-Patient scholar, Marie Ennis O’Connor is an internationally recognized keynote speaker, writer, and consultant on global trends in patient engagement, digital health and participatory medicine. Marie’s work is informed by her passion for embedding the patient voice at the heart of healthcare values. She writes about the experience of transitioning from breast cancer patient to advocate on her award-winning blog Journeying Beyond Breast Cancer.



 “It feels so good,” I said during our telemedicine appointment, “to be away from the hospital for eight weeks in a row.” It’s the longest hospital break I’ve had since being diagnosed with cancer last summer. Before mid-March, I’d been to four to ten medical appointments every month. Being a cancer patient felt like a full or half time job. Because of the pandemic, I’m now treated by my oncology team from the comfort of my own home.
“It feels so good,” I said during our telemedicine appointment, “to be away from the hospital for eight weeks in a row.” It’s the longest hospital break I’ve had since being diagnosed with cancer last summer. Before mid-March, I’d been to four to ten medical appointments every month. Being a cancer patient felt like a full or half time job. Because of the pandemic, I’m now treated by my oncology team from the comfort of my own home.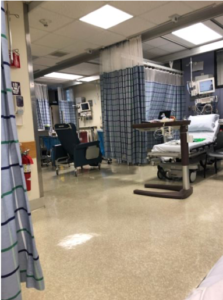 My partner drove me to the hospital on the morning of my surgery. We checked in before 6a.m. and waited, with others, in the lobby.
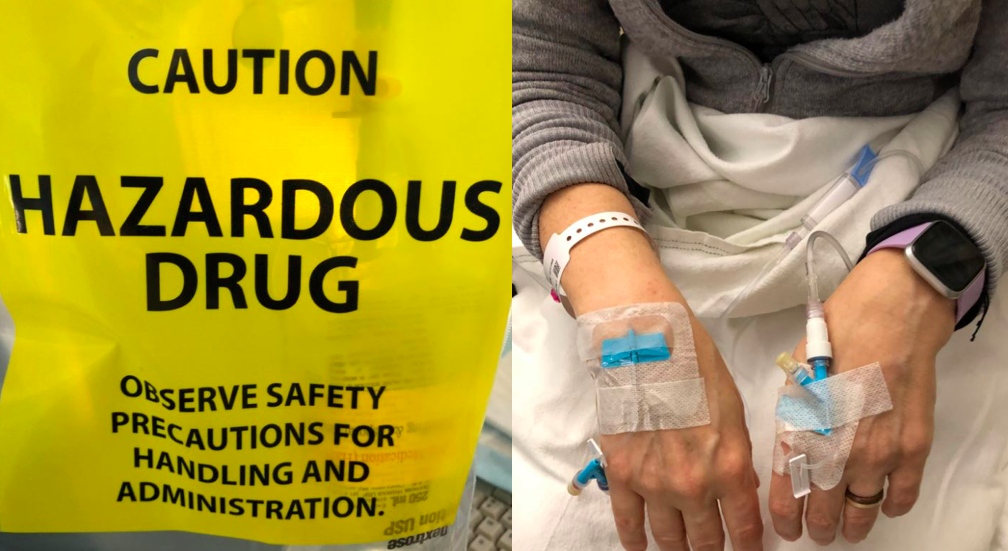
My partner drove me to the hospital on the morning of my surgery. We checked in before 6a.m. and waited, with others, in the lobby. This is me in post-op. My partner took this photo on his phone and was able to share it with my family and friends to let them know I made it through surgery. They were worried because it went hours longer than expected.
This is me in post-op. My partner took this photo on his phone and was able to share it with my family and friends to let them know I made it through surgery. They were worried because it went hours longer than expected. Going home after surgery is comforting and scary. My right leg was giving out from under me because my obturator nerve “got heat” during my surgery. I had trouble standing in the shower or lifting my right leg onto the bed or into a car. I had extensive swelling and bruising on my right side and pelvic area and had a bit of a reaction to the bandage tape. I didn’t know what was normal. And after a phone call to the hospital, I was asked to come back in for a check-up.
Going home after surgery is comforting and scary. My right leg was giving out from under me because my obturator nerve “got heat” during my surgery. I had trouble standing in the shower or lifting my right leg onto the bed or into a car. I had extensive swelling and bruising on my right side and pelvic area and had a bit of a reaction to the bandage tape. I didn’t know what was normal. And after a phone call to the hospital, I was asked to come back in for a check-up.